Abstract
Aims
Gestational diabetes mellitus (GDM) is a medical complication of any degree of glucose intolerance with onset or first recognition during pregnancy. Although visfatin is commonly considered to be related to GDM, studies revealed inconsistent results. This study aimed to clarify the relationship between visfatin and GDM.
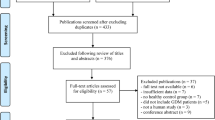
Methods
The protocol for this study was registered in PROSPERO (No. CRD42018086204) in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). PubMed and Embase databases were used to search for relevant studies published up to September 30, 2017. The difference of visfatin levels between women with GDM and the controls was measured by standardised mean difference (SMD) and 95% confidence interval (CI).
Results
Twenty-six studies that were published in 24 articles met the inclusion criteria, in which 2305 participants (1033 with GDM, mean age 31.39 years and 1272 controls, and mean age 29.99 years) were included. The quantitative meta-analysis revealed no significant difference in circulating visfatin levels between women with GDM and the controls (SMD = 0.249, 95% CI = − 0.079 to 0.576, P = 0.137). Subgroup analyses were performed referring to body mass index (BMI) where inconsistent results have been observed between cases and controls groups. For the ten studies, in which the level of BMI in women with GDM was higher than that in the control group, the pooled result showed that circulating visfatin was significantly higher among women with GDM than the controls (SMD = 0.367, 95% CI = 0.06 to 0.728, P = 0.046). Of other 16 studies BMI-matched, the pooled SMD illustrated no difference of visfatin.
Conclusions
Our study elucidates that visfatin is not independently associated with GDM. Visfatin is linked to GDM through maternal overweight/obesity, which is one of the major factors leading to the development of GDM.




Similar content being viewed by others
References
Daly B, Toulis KA, Thomas N et al (2018) Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. PLoS Med 15(1):e1002488
American Diabetes Association (2015) Classification and diagnosis of diabetes. Diabetes Care 38(Suppl):S8–S16
Yang H, Wei Y, Gao X et al (2009) Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16,286 pregnant women in China. Diabet Med 26(11):1099–1104
Lobo TF, Torloni MR, Gueuvoghlanian-Silva BY, Mattar R, Daher S (2013) Resistin concentration and gestational diabetes: a systematic review of the literature. J Reprod Immunol 97(1):120–127
Noureldeen AF, Qusti SY, Al-Seeni MN, Bagais MH (2014) Maternal leptin, adiponectin, resistin, visfatin and tumor necrosis factor-alpha in normal and gestational diabetes. Indian J Clin Biochem 29(4):462–470
Görkem Ü, Küçükler FK, Toğrul C, Güngör T (2016) Are adipokines associated with gestational diabetes mellitus? J Turk Ger Gynecol Assoc 17(4):186–190
Griffin ME, Coffey M, Johnson H et al (2000) Universal vs. risk factor based screening for gestational diabetes mellitus: detection rates, gestation at diagnosis and outcome. Diabet Med 17(1):26–32
Sorbye LM, Skjaerven R, Klungsoyr K, Morken NH (2017) Gestational diabetes mellitus and interpregnancy weight change: a population-based cohort study. PLoS Med 14(8):e1002367
Shimomura I, Hammer RE, Ikemoto S, Brown MS, Goldstein JL (1999) Leptin reverses insulin resistance and diabetes mellitus in mice with congenital lipodystrophy. Nature 401(6748):73–76
Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444(7121):840–846
Kaaja R, Rönnemaa T (2008) Gestational diabetes: pathogenesis and consequences to mother and offspring. Rev Diabet Stud 5(4):194–202
Adeghate E (2008) Visfatin: structure, function and relation to diabetes mellitus and other dysfunctions. Curr Med Chem 15(18):1851–1862
Liang Z, Wu Y, Xu J, Fang Q, Chen D (2016) Correlations of serum visfatin and metabolisms of glucose and lipid in women with gestational diabetes mellitus. J Diabetes Investig 7(2):247–252
Kaygusuz I, Gumus II, Yılmaz S et al (2013) Serum levels of visfatin and possible interaction with iron parameters in gestational diabetes mellitus. Gynecol Obstet Investig 75(3):203–209
Ferreira AF, Rezende JC, Vaikousi E, Akolekar R, Nicolaides KH (2011) Maternal serum visfatin at 11–13 weeks of gestation in gestational diabetes mellitus. Clin Chem 57(4):609–613
Ma Y, Cheng Y, Wang J, Cheng H, Zhou S, Li X. The changes of visfatin in serum and its expression in fat and placental tissue in pregnant women with gestational diabetes. Diabetes Res Clin Pract 90(1):60–65
Gok DE, Yazici M, Uckaya G et al (2011) The role of visfatin in the pathogenesis of gestational diabetes mellitus. J Endocrinol Investig 34(1):3–7
Coskun A, Ozkaya M, Kiran G, Kilinc M, Arikan DC (2010) Plasma visfatin levels in pregnant women with normal glucose tolerance, gestational diabetes and pre-gestational diabetes mellitus. J Matern Fetal Neonatal Med 23(9):1014–1018
Lewandowski KC, Stojanovic N, Press M et al (2007) Elevated serum levels of visfatin in gestational diabetes: a comparative study across various degrees of glucose tolerance. Diabetologia 50(5):1033–1037
Krzyzanowska K, Krugluger W, Mittermayer F et al (2006) Increased visfatin concentrations in women with gestational diabetes mellitus. Clin Sci (Lond) 110(5):605–609
Hossein-nezhad A, Mirzaei K, Maghbooli Z, Rahmani M, Larijani B (2010) Resistin, adiponectin and visfatin; can adipocytokines predict gestational diabetes mellitus and early post partum metabolic syndrome? Iran J Diabetes Lipid Disord 9:1–8
Lei C (2009) The analysis of serum adiponectin and visfatin levels in pregnancy with different glucose tolerance and the effect on the secretary function of beta cell. Dissertation. Ningxia Medical University, Yinchuan
Abell SK, Shorakae S, Harrison CL et al (2017) The association between dysregulated adipocytokines in early pregnancy and development of gestational diabetes. Diabetes Metab Res Rev 33(8):e2926
Karatas A, Tunçay Işikkent N, Ozlü T, Demirin H (2014) Relationship of maternal serum resistin and visfatin levels with gestational diabetes mellitus. Gynecol Endocrinol 30(5):355–358
Boyadzhieva M, Atanasova I, Zacharieva S, Kedikova S (2013) Adipocytokines during pregnancy and postpartum in women with gestational diabetes and healthy controls. J Endocrinol Investig 36(11):944–949
Skvarca A, Tomazic M, Krhin B, Blagus R, Janez A (2012) Adipocytokines and insulin resistance across various degrees of glucose tolerance in pregnancy. J Int Med Res 40(2):583–589
Maitland RA, Seed PT, Briley AL et al (2014) Prediction of gestational diabetes in obese pregnant women from the UK Pregnancies Better Eating and Activity (UPBEAT) pilot trial. Diabet Med 31(8):963–970
Oncul M, Tuten A, Erman H et al (2013) Maternal and cord blood apelin, resistin and visfatin levels in gestational diabetes mellitus. Minerva Med 104(5):527–535
Rezvan N, Hosseinzadeh-Attar MJ, Masoudkabir F, Moini A, Janani L, Mazaherioun M (2012) Serum visfatin concentrations in gestational diabetes mellitus and normal pregnancy. Arch Gynecol Obstet 285(5):1257–1262
Szamatowicz J, Kuźmicki M, Telejko B et al (2009) Serum visfatin concentration is elevated in pregnant women irrespectively of the presence of gestational diabetes. Ginekol Pol 80(1):14–18
Telejko B, Kuzmicki M, Zonenberg A et al (2009) Visfatin in gestational diabetes: serum level and mRNA expression in fat and placental tissue. Diabetes Res Clin Pract 84(1):68–75
Akturk M, Altinova AE, Mert I et al (2008) Visfatin concentration is decreased in women with gestational diabetes mellitus in the third trimester. J Endocrinol Investig 31(7):610–613
Haider DG, Handisurya A, Storka A et al (2007) Visfatin response to glucose is reduced in women with gestational diabetes mellitus. Diabetes Care 30(7):1889–1891
Chan TF, Chen YL, Lee CH et al (2006) Decreased plasma visfatin concentrations in women with gestational diabetes mellitus. J Soc Gynecol Investig 13(5):364–367
Hou H, Ge S, Zhao L et al (2017) An updated systematic review and meta-analysis of association between adiponectin gene polymorphisms and coronary artery disease. OMICS 21(6):340–351
Hou H, Zhao Y, Yu W et al (2018) Association of obstructive sleep apnea with hypertension: a systematic review and meta-analysis. J Glob Health 8(1):010405
Thakkinstian A, McEvoy M, Minelli C et al (2005) Systematic review and meta-analysis of the association between {beta}2-adrenoceptor polymorphisms and asthma: a HuGE review. Am J Epidemiol 162(3):201–211
Hou H, Sun T, Li C et al (2017) An overall and dose–response meta-analysis of red blood cell distribution width and CVD outcomes. Sci Rep 7:43420
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Elsaid A, Abdel-Aziz AF, Elmougy R, Elwaseef AM (2014) Association of polymorphisms G(−174)C in IL-6 gene and G(−1082)A in IL-10 gene with traditional cardiovascular risk factors in patients with coronary artery disease. Indian J Biochem Biophys 51(4):282–292
Papageorgiou SN (2014) Meta-analysis for orthodontists: part II—is all that glitters gold? J Orthod 41(4):327–336
Ma HH, Yang SY, Wang P, Zhang JF (2017) Evaluation of the value of plasma concentration of copeptin in the first prenatal visit to diagnose gestational diabetes mellitus. Acta Diabetol 54(12):1123–1129
Burlina S, Dalfrà MG, Barison A et al (2017) Plasma phospholipid fatty acid composition and desaturase activity in women with gestational diabetes mellitus before and after delivery. Acta Diabetol 54(1):45–51
Jarrar MH, Baranova A, Collantes R et al (2008) Adipokines and cytokines in non-alcoholic fatty liver disease. Aliment Pharmacol Ther 27(5):412–421
Sethi JK, Vidal-Puig A (2005) Visfatin: the missing link between intra-abdominal obesity and diabetes? Trends Mol Med 11(8):344–347
Lobo TF, Torloni MR, Mattar R, Nakamura MU, Alexandre SM, Daher S (2018) Adipokine levels in overweight women with early-onset gestational diabetes mellitus. J Endocrinol Investig. https://doi.org/10.1007/s40618-018-0894-0
Rasouli N, Kern PA (2008) Adipocytokines and the metabolic complications of obesity. J Clin Endocrinol Metab 93:S64–S73
Galic S, Oakhill JS, Steinberg GR (2010) Adipose tissue as an endocrine organ. Mol Cell Endocrinol 316(2):129–139
Lowe LP, Metzger BE, Lowe WL Jr, Dyer AR, McDade TW, McIntyre HD (2010) Inflammatory mediators and glucose in pregnancy: results from a subset of the hyperglycemia and adverse pregnancy outcome (HAPO) study. J Clin Endocrinol Metab 95(12):5427–5434
Mottola MF, Artal R (2016) Role of exercise in reducing gestational diabetes mellitus. Clin Obstet Gynecol 59(3):620–628
Haider DG, Holzer G, Schaller G et al (2006) The adipokine visfatin is markedly elevated in obese children. J Pediatr Gastroenterol Nutr 43(4):548–549
Berndt J, Klöting N, Kralisch S et al (2005) Plasma visfatin concentrations and fat depot-specific mRNA expression in humans. Diabetes 54(10):2911–2916
Acknowledgements
We would like to thank Wei Wang, Edith Cowan University School of Medical and Health Sciences, for his help with conducting a scoping review for this study.
Author information
Authors and Affiliations
Contributions
HH, AD, and XJ designed the study. WZ, DZ, ZM HW, KZ, XF, and YL conducted the literature search, performed data extraction, and assessed study quality. HH and XJ conducted the statistical analyses. HH and AD wrote the manuscript. All authors interpreted data and revised the manuscript for important intellectual content. HH conceived of the study idea, supervised the study, and is the guarantor.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical standards
This study used published, aggregate data and did not involve human participants or animals. Consequently, research ethics board review was not required.
Informed consent
Not applicable.
Additional information
Managed by Antonio Secchi.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, W., Zhao, D., Meng, Z. et al. Association between circulating visfatin and gestational diabetes mellitus: a systematic review and meta-analysis. Acta Diabetol 55, 1113–1120 (2018). https://doi.org/10.1007/s00592-018-1188-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1188-x