Abstract
Aims
Enteroviruses, especially coxsackieviruses B (CV-B), have been associated with the pathogenesis of type 1 diabetes (T1D). An anti-CV-B4 neutralizing activity in saliva of T1D patients was previously reported. Our aim was to study the association between the saliva anti-CV-B4 neutralizing activity and immune parameters in T1D patients in comparison with non-diabetic individuals.
Methods
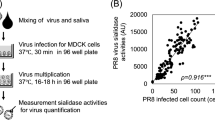
Saliva and blood samples were collected from 15 T1D patients and 8 controls. The anti-CV-B4 and anti-poliovirus type 1 (PV-1) activities of saliva and serum samples were determined by a plaque neutralization assay. Quantification of serum cytokines was performed by ELISA and the frequencies of lymphocyte subsets were evaluated using flow cytometry.
Results
The levels of salivary anti-CV-B4 neutralizing activity were higher in T1D patients than in controls (p = 0.02), whereas the serum levels of anti-CV-B4 neutralizing activity and the saliva and serum levels of anti-PV-1 neutralizing activity were not different. The proportions of effector CD4+ T cells and CD19+ B cells, but not those of CD4+ T cells, CD8+ T cells and Foxp3+ regulatory T cells, were higher in T1D patients than in controls (p = 0.02 and p = 0.01 respectively). Moreover, serum IFN-γ levels were lower in T1D patients compared to controls (p = 0.03) while IL-4 and IL-10 were not different. There was an association between saliva anti-CV-B4 activity, down-regulation of IFN-γ and B cell expansion in peripheral blood of T1D patients.
Conclusion
The association between saliva anti-CV-B4 activity and disturbance of immune system in T1D patients deserves further investigation.



Similar content being viewed by others
References
Zell R, Delwart E, Gorbalenya AE et al (2017) ICTV virus taxonomy profile: picornaviridae. J Gen Virol 98:2421–2422. https://doi.org/10.1099/jgv.0.000911
Hober D, Sauter P (2010) Pathogenesis of type 1 diabetes mellitus: Interplay between enterovirus and host. Nat Rev Endocrinol 6:279–289. https://doi.org/10.1038/nrendo.2010.27
Jaïdane H, Sauter P, Sane F et al (2010) Enteroviruses and type 1 diabetes: towards a better understanding of the relationship. Rev Med Virol. https://doi.org/10.1002/rmv.647
Yeung W-CG, Rawlinson WD, Craig ME (2011) Enterovirus infection and type 1 diabetes mellitus: systematic review and meta-analysis of observational molecular studies. BMJ 342:d35–d35. https://doi.org/10.1136/bmj.d35
Tapparel C, Siegrist F, Petty TJ, Kaiser L (2013) Picornavirus and enterovirus diversity with associated human diseases. Infect Genet Evol 14:282–293
Oikarinen S, Martiskainen M, Tauriainen S et al (2011) Enterovirus RNA in blood is linked to the development of type 1 diabetes. Diabetes 60:276–279. https://doi.org/10.2337/db10-0186
Oikarinen M, Tauriainen S, Oikarinen S et al (2012) Type 1 diabetes is associated with enterovirus infection in gut mucosa. Diabetes 61:687–691. https://doi.org/10.2337/db11-1157
Krogvold L, Edwin B, Buanes T et al (2015) Detection of a low-grade enteroviral infection in the islets of langerhans of living patients newly diagnosed with type 1 diabetes. Diabetes 64:1682–1687. https://doi.org/10.2337/db14-1370
Alidjinou EK, Chehadeh W, Weill J et al (2015) Monocytes of patients with type 1 diabetes harbour enterovirus RNA. Eur J Clin Invest 45:918–924. https://doi.org/10.1111/eci.12485
Hober D, Alidjinou EK (2013) Enteroviral pathogenesis of type 1 diabetes: queries and answers. Curr Opin Infect Dis 26:263–269. https://doi.org/10.1097/QCO.0b013e3283608300
Alidjinou EK, Sané F, Engelmann I et al (2014) Enterovirus persistence as a mechanism in the pathogenesis of type 1 diabetes. Discov Med 18:273–282
Racaniello VR (2013) Picornaviridae: the viruses and their replication. In: Fields virology. Philadelphia, PA, USA, pp 453–490
Cesta MF (2006) Normal structure, function, and histology of mucosa-associated lymphoid tissue. Toxicol Pathol 34:599–608. https://doi.org/10.1080/01926230600865531
Neutra MR, Kozlowski PA (2006) Mucosal vaccines: the promise and the challenge. Nat Rev Immunol 6:148–158. https://doi.org/10.1038/nri1777
Blutt SE, Conner ME (2013) The gastrointestinal frontier: IgA and viruses. Front Immunol 4:1–12. https://doi.org/10.3389/fimmu.2013.00402
Kim S-H, Jang Y-S (2017) The development of mucosal vaccines for both mucosal and systemic immune induction and the roles played by adjuvants. Clin Exp Vaccine Res 6:15. https://doi.org/10.7774/cevr.2017.6.1.15
Kiyono H, Fukuyama S (2004) Nalt-versus Peyer’s-patch-mediated mucosal immunity. Nat Rev Immunol 4:699–710. https://doi.org/10.1038/nri1439
Badia-Boungou F, Sane F, Alidjinou EK et al (2017) Marker of coxsackievirus-B4 infection in saliva of patients with type 1 diabetes. Diabetes Metab Res Rev 33:e2916. https://doi.org/10.1002/dmrr.2916
Holmgren J, Czerkinsky C (2005) Mucosal immunity and vaccines. Nat Med 11:S45. https://doi.org/10.1038/nm1213
Lycke N (2012) Recent progress in mucosal vaccine development: potential and limitations. Nat Rev Immunol 12:592–605. https://doi.org/10.1038/nri3251
Macpherson AJ, Hunziker L, McCoy K, Lamarre A (2001) IgA responses in the intestinal mucosa against pathogenic and non-pathogenic microorganisms. Microbes Infect 3:1021–1035
American Diabetes Association (2018) Standards of medical care in diabetes—2018 abridged for primary care providers. Clin Diabetes 36:14–37. https://doi.org/10.2337/cd17-0119
Sane F, Caloone D, Gmyr V et al (2013) Coxsackievirus B4 can infect human pancreas ductal cells and persist in ductal-like cell cultures which results in inhibition of Pdx1 expression and disturbed formation of islet-like cell aggregates. Cell Mol Life Sci 70:4169–4180. https://doi.org/10.1007/s00018-013-1383-4
Thevenin T, Lobert PE, Hober D (2013) Inactivation of an enterovirus by airborne disinfectants. BMC Infect Dis 13:2–5. https://doi.org/10.1186/1471-2334-13-177
Nekoua MP, Fachinan R, Atchamou AK et al (2016) Modulation of immune cells and Th1/Th2 cytokines in insulin-treated type 2 diabetes mellitus. Afr Health Sci 16:712–724. https://doi.org/10.4314/ahs.v16i3.11
Tauriainen S, Oikarinen S, Oikarinen M, Hyöty H (2011) Enteroviruses in the pathogenesis of type 1 diabetes. Semin Immunopathol 33:45–55. https://doi.org/10.1007/s00281-010-0207-y
Green J, Casabonne D, Newton R (2004) Coxsackie B virus serology and type 1 diabetes mellitus: a systematic review of published case–control studies. Diabet Med 21:507–514. https://doi.org/10.1111/j.1464-5491.2004.01182.x
Wan YY, Flavell R (2009) How diverse—CD4 effector T cells and their functions. J Mol Cell Biol 1:20–36
Zhu J, Yamane H, Paul W (2010) Differentiation of effector CD4 T cell populations. Annu Rev Immunol 28:445–489. https://doi.org/10.1146/annurev-immunol-030409-101212.Differentiation
Halminen M, Simell O, Knip M, Ilonen J (2001) Cytokine expression in unstimulated PBMC of children with type 1 diabetes and subjects positive for diabetes-associated autoantibodies. Scand J Immunol 53:510–513. https://doi.org/10.1046/j.1365-3083.2001.00904.x
Kukreja A, Cost G, Marker J et al (2002) Multiple immuno-regulatory defects in type-1 diabetes. J Clin Investig 109:131–140. https://doi.org/10.1172/JCI200213605
Karlsson Faresjö MGE, Ernerudh J, Ludvigsson J (2004) Cytokine profile in children during the first 3 months after the diagnosis of type 1 diabetes. Scand J Immunol 59:517–526. https://doi.org/10.1111/j.0300-9475.2004.01420.x
Chatzigeorgiou A, Harokopos V, Mylona-Karagianni C et al (2010) The pattern of inflammatory/anti-inflammatory cytokines and chemokines in type 1 diabetic patients over time. Ann Med 42:426–438. https://doi.org/10.3109/07853890.2010.495951
Walker LSK, von Herrath M (2016) CD4 T cell differentiation in type 1 diabetes. Clin Exp Immunol 183:16–29. https://doi.org/10.1111/cei.12672
Brandtzaeg P (2010) Function of mucosa-associated lymphoid tissue in antibody formation. Immunol Investig 39:303–355. https://doi.org/10.3109/08820131003680369
Lindley S, Dayan CM, Bishop A et al (2005) Defective suppressor function in CD4+ CD25+ T-cells from patients with type 1 diabetes. Diabetes 54:92–99. https://doi.org/10.2337/diabetes.54.1.92
Brusko TM, Wasserfall CH, Clare-Salzler MJ et al (2005) Functional defects and the influence of age on the frequency of CD4+ CD25+ T-cells in type 1 diabetes. Diabetes 54:1407–1414. https://doi.org/10.2337/diabetes.54.5.1407
Aghili B, Amirzargar AA, Rajab A et al (2015) Altered suppressor function of regulatory T cells in type 1 diabetes. Iran J Immunol 12:240–251. doi: IJIv12i4A2
Putnam AL, Vendrame F, Dotta F, Gottlieb PA (2005) CD4(+)CD25(high) regulatory T cells in human autoimmune diabetes. J Autoimmun 24:55–62. https://doi.org/10.1016/j.jaut.2004.11.004
Brusko T, Wasserfall C, McGrail K et al (2007) No alterations in the frequency of FOXP3+ regulatory T-cells in type 1 diabetes. Diabetes 56:604–612. https://doi.org/10.2337/db06-1248
Hamari S, Kirveskoski T, Glumoff V et al (2016) Analyses of regulatory CD4+ CD25+ FOXP3+ T cells and observations from peripheral T cell subpopulation markers during the development of type 1 diabetes in children. Scand J Immunol 83:279–287. https://doi.org/10.1111/sji.12418
Zargari Samani O, Mahmoodnia L, Izad M et al (2018) Alteration in CD8+ T cell subsets in enterovirus-infected patients: an alarming factor for type 1 diabetes mellitus. Kaohsiung J Med Sci. https://doi.org/10.1016/j.kjms.2017.12.010
Acknowledgements
This work was supported by Ministère de l’Education Nationale de la Recherche et de la Technologie, Université Lille 2 (Equipe d’accueil 3610), Centre Hospitalier Régional et Universitaire de Lille, Institut des Sciences Biomédicales Appliquées (ISBA) and Université d’Abomey-Calavi (République du Benin). We thank Institut de Recherche pour le Développement (IRD-UMR216) and CERPAGE (Centre d’Etude et de Recherche sur le Paludisme associé à la Grossesse et à l’Enfance) who provided the flow cytometry platform. M. P. N was supported by a “CABRI 2016” scholarship of Université Lille 2 and a “Programme Eiffel 2017” scholarship of Ministère des Affaires étrangères et du Développement international de la République Française.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Federici.
Rights and permissions
About this article
Cite this article
Nekoua, M.P., Yessoufou, A., Alidjinou, E.K. et al. Salivary anti-coxsackievirus-B4 neutralizing activity and pattern of immune parameters in patients with type 1 diabetes: a pilot study. Acta Diabetol 55, 827–834 (2018). https://doi.org/10.1007/s00592-018-1158-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1158-3