Abstract
Aims
We evaluate prevalence of new abnormal glucose tolerance (AGT) in post-MI survivors without known diabetes (DM) if guidelines are followed and compare the ability of admission (APG), fasting (FPG) and 2-h post-load plasma glucose (2h-PG) to predict prognosis.
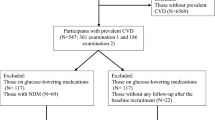
Methods
A total of 674 patients were followed up for 4 years for incidence of major adverse cardiovascular events (MACE) of cardiovascular death, non-fatal re-infarction or non-haemorrhagic stroke. Ability of models including APG, FPG and 2h-PG to predict MACE was compared.
Results
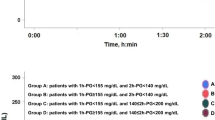
Of the total, 93–96% of impaired glucose tolerance and 64–75% of DM would be missed with current guidelines. MACE was higher in the upper quartiles of 2h-PG. When 2h-PG and FPG were included simultaneously in models, only 2h-PG predicted MACE (HR 1.12, CI 1.04–1.20, p = 0.0012), all cause mortality (HR 1.17, CI 1.05–1.30, p = 0.0039), cardiovascular mortality (HR 1.17, CI 1.02–1.33, p = 0.0205) and non-fatal MI (HR 1.10, CI 1.01–1.20, p = 0.0291). Adding 2h-PG significantly improved ability of models including FPG (χ2 = 16.01, df = 1, p = 0.0001) or FPG and APG (χ2 = 17.36, df = 1, p = 0.000) to predict MACE. Model including 2h-PG only had the lowest Akaike’s information criteria and highest Akaike weights suggesting that this was the best in predicting events. Adding 2h-PG to models including FPG or APG with other co-variates yielded continuous net reclassification improvement (NRI) of 0.22 (p = 0.026) and 0.27 (p = 0.005) and categorical NRI of 0.09 (p = 0.032) and 0.12 (p = 0.014), respectively. Adding 2 h-PG to models including only FPG, only APG and both yielded integrated discrimination improvement of 0.012 (p = 0.015), 0.022 (p = 0.001) and 0.013 (p = 0.014), respectively.
Conclusions
AGT is under-diagnosed on current guidelines. 2h-PG is a better predictor of prognosis compared to APG and FPG.


Similar content being viewed by others
Change history
05 March 2018
Unfortunately, name of co-author “Thozhukat” was misspelled in the original publication and the same is corrected here. The original article has been corrected.
References
National Institute for Health and Care Excellence. Clinical guideline [CG130]: Hyperglycaemia in acute coronary syndromes: management. https://www.niceorguk/guidance/cg130
Ryden L, Grant PJ, Anker SD et al (2013) ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 34:3035–3087
Senthinathan A, Kelly V, Dzingina M et al (2011) Hyperglycaemia in acute coronary syndromes: summary of NICE guidance. BMJ 343:d6646
Bartnik M, Ryden L, Malmberg K et al (2007) Oral glucose tolerance test is needed for appropriate classification of glucose regulation in patients with coronary artery disease: a report from the Euro Heart Survey on Diabetes and the Heart. Heart 93:72–77
de Mulder M, Oemrawsingh RM, Stam F, Boersma E, Umans VA (2012) Comparison of diagnostic criteria to detect undiagnosed diabetes in hyperglycaemic patients with acute coronary syndrome. Heart 98:37–41
Hage C, Lundman P, Ryden L, Mellbin L (2013) Fasting glucose, HbA1c, or oral glucose tolerance testing for the detection of glucose abnormalities in patients with acute coronary syndromes. Eur J Prev Cardiol 20:549–554
Doerr R, Hoffmann U, Otter W et al (2011) Oral glucose tolerance test and HbA(1)c for diagnosis of diabetes in patients undergoing coronary angiography: [corrected] the Silent Diabetes Study. Diabetologia 54:2923–2930
Tenerz A, Nilsson G, Forberg R et al (2003) Basal glucometabolic status has an impact on long-term prognosis following an acute myocardial infarction in non-diabetic patients. J Intern Med 254:494–503
Timmer JR, Hoekstra M, Nijsten MW et al (2011) Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation 124:704–711
Pararajasingam G, Hofsten DE, Logstrup BB et al (2016) Newly detected abnormal glucose regulation and long-term prognosis after acute myocardial infarction: Comparison of an oral glucose tolerance test and glycosylated haemoglobin A1c. Int J Cardiol 214:310–315
Aggarwal B, Shah GK, Randhawa M et al (2016) Utility of glycated hemoglobin for assessment of glucose metabolism in patients with ST-segment elevation myocardial infarction. Am J Cardiol 117:749–753
Gustafsson I, Kistorp CN, James MK et al (2007) Unrecognized glycometabolic disturbance as measured by hemoglobin A1c is associated with a poor outcome after acute myocardial infarction. Am Heart J 154:470–476
Kitada S, Otsuka Y, Kokubu N et al (2010) Post-load hyperglycemia as an important predictor of long-term adverse cardiac events after acute myocardial infarction: a scientific study. Cardiovasc Diabetol 9:75
Tamita K, Katayama M, Takagi T et al (2007) Impact of newly diagnosed abnormal glucose tolerance on long-term prognosis in patients with acute myocardial infarction. Circ J 71:834–841
Bartnik M, Malmberg K, Norhammar A et al (2004) Newly detected abnormal glucose tolerance: an important predictor of long-term outcome after myocardial infarction. Eur Heart J 25:1990–1997
Knudsen EC, Seljeflot I, Abdelnoor M et al (2011) Impact of newly diagnosed abnormal glucose regulation on long-term prognosis in low risk patients with ST-elevation myocardial infarction: a follow-up study. BMC Endocr Disord 11:14
George A, Bhatia RT, Buchanan GL et al (2015) Impaired glucose tolerance or newly diagnosed diabetes mellitus diagnosed during admission adversely affects prognosis after myocardial infarction: an observational study. PLoS ONE 10:e0142045
Lenzen M, Ryden L, Ohrvik J et al (2006) Diabetes known or newly detected, but not impaired glucose regulation, has a negative influence on 1-year outcome in patients with coronary artery disease: a report from the Euro Heart Survey on diabetes and the heart. Eur Heart J 27:2969–2974
Tamita K, Katayama M, Takagi T et al (2012) Newly diagnosed glucose intolerance and prognosis after acute myocardial infarction: comparison of post-challenge versus fasting glucose concentrations. Heart 98:848–854
Mazurek M, Kowalczyk J, Lenarczyk R et al (2012) The prognostic value of different glucose abnormalities in patients with acute myocardial infarction treated invasively. Cardiovasc Diabetol 11:78
Ritsinger V, Tanoglidi E, Malmberg K et al (2014) Sustained prognostic implications of newly detected glucose abnormalities in patients with acute myocardial infarction: long-term follow-up of the Glucose Tolerance in Patients with Acute Myocardial Infarction cohort. Diabetes Vasc Dis Res 12:23
Thygesen K, Alpert JS, White HD (2007) Universal definition of myocardial infarction. Eur Heart J 28:2525–2538
Ryden L, Standl E, Bartnik M et al (2007) Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 28:88–136
American Diabetes Association (1997) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20:1183–1197
Genuth S, Alberti KG, Bennett P et al (2003) Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26:3160–3167
American Diabetes Association (2012) Standards of medical care in diabetes–2012. Diabetes Care 35(Suppl 1):S11–S63
Y Sakamoto, M Ishiguro, G Kitagawa (1986) Akaike information criterion statistics. Springer, Netherlands
Wagenmakers EJ, Farrell S (2004) AIC model selection using Akaike weights. Psychon Bull Rev 11:192–196
Bartnik M, Ryden L, Ferrari R et al (2004) The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The Euro Heart Survey on diabetes and the heart. Eur Heart J 25:1880–1890
Norhammar A, Tenerz A, Nilsson G et al (2002) Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet 359:2140–2144
The DECODE Study Group (2001) Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med 161:397–405
Knudsen EC, Seljeflot I, Abdelnoor M et al (2009) Abnormal glucose regulation in patients with acute ST-elevation myocardial infarction-a cohort study on 224 patients. Cardiovasc Diabetol 8:6
Suleiman M, Hammerman H, Boulos M et al (2005) Fasting glucose is an important independent risk factor for 30-day mortality in patients with acute myocardial infarction: a prospective study. Circulation 111:754–760
Avezum A, Makdisse M, Spencer F et al (2005) Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J 149:67–73
Mandelzweig L, Battler A, Boyko V et al (2006) The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 27:2285–2293
Smith NL, Barzilay JI, Shaffer D et al (2002) Fasting and 2-hour postchallenge serum glucose measures and risk of incident cardiovascular events in the elderly: the Cardiovascular Health Study. Arch Intern Med 162:209–216
Qiao Q, Pyorala K, Pyorala M et al (2002) Two-hour glucose is a better risk predictor for incident coronary heart disease and cardiovascular mortality than fasting glucose. Eur Heart J 23:1267–1275
Sinnaeve PR, Steg PG, Fox KA et al (2009) Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST-segment elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med 169:402–409
Ravid M, Berkowicz M, Sohar E (1975) Hyperglycemia during acute myocardial infarction. A six-year follow-up study. JAMA 233:807–809
Ando T, Okada S, Niijima Y et al (2010) Impaired glucose tolerance, but not impaired fasting glucose, is a risk factor for early-stage atherosclerosis. Diabet Med 27:1430–1435
Choi ES, Rhee EJ, Choi JH et al (2010) The association of brachial-ankle pulse wave velocity with 30-minute post-challenge plasma glucose levels in korean adults with no history of type 2 diabetes. Korean Diabetes J 34:287–293
Mellen PB, Bittner V, Herrington DM (2007) Post-challenge glucose predicts coronary atherosclerotic progression in non-diabetic, post-menopausal women. Diabet Med 24:1156–1159
Hanefeld M, Koehler C, Henkel E et al (2000) Post-challenge hyperglycaemia relates more strongly than fasting hyperglycaemia with carotid intima-media thickness: the RIAD Study. Risk factors in impaired glucose tolerance for atherosclerosis and diabetes. Diabet Med 17:835–840
Temelkova-Kurktschiev TS, Koehler C, Henkel E et al (2000) Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23:1830–1834
Wallander M, Malmberg K, Norhammar A, Ryden L, Tenerz A (2008) Oral glucose tolerance test: a reliable tool for early detection of glucose abnormalities in patients with acute myocardial infarction in clinical practice: a report on repeated oral glucose tolerance tests from the GAMI study. Diabetes Care 31:36–38
Tenerz A, Norhammar A, Silveira A et al (2003) Diabetes, insulin resistance, and the metabolic syndrome in patients with acute myocardial infarction without previously known diabetes. Diabetes Care 26:2770–2776
Hage C, Malmberg K, Ryden L, Wallander M (2010) The impact of infarct type on the reliability of early oral glucose tolerance testing in patients with myocardial infarction. Int J Cardiol 145:259–260
Moura FA, Figueiredo VN, Teles BS et al (2015) Glycosylated hemoglobin is associated with decreased endothelial function, high inflammatory response, and adverse clinical outcome in non-diabetic STEMI patients. Atherosclerosis 243:124–130
Liu XJ, Wan ZF, Zhao N et al (2015) Adjustment of the GRACE score by Hemoglobin A1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol 19:110
Geng J, Zhang Y, Wang B et al (2017) Glycosylated hemoglobin levels and clinical outcomes in nondiabetic patients with coronary artery disease: a meta-analysis. Medicine (Baltimore) 96:e6784
Shin D, Ahn J, Cha KS et al (2016) Impact of initial glycosylated hemoglobin level on cardiovascular outcomes in prediabetic patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis 27:40–46
Lazzeri C, Valente S, Chiostri M et al (2015) Glycated haemoglobin and long-term mortality in patients with ST Elevation Myocardial Infarction. J Cardiovasc Med (Hagerstown) 16:404–408
Shahim B, De Bacquer D, De Backer G et al (2017) The prognostic value of fasting plasma glucose, two-hour postload glucose, and HbA1c in patients with coronary artery disease: a report from EUROASPIRE IV—a survey from the European Society of Cardiology. Diabetes Care 40:1233–1240
Tailakh MA, Friger M, Zahger D et al (2017) Prospective study of the impact of diabetes mellitus newly diagnosed by glycated hemoglobin on outcomes in patients undergoing percutaneous coronary intervention. Eur J Intern Med 37:69–74
Kowalczyk J, Mazurek M, Zielinska T et al (2015) Prognostic significance of HbA1c in patients with AMI treated invasively and newly detected glucose abnormalities. Eur J Prev Cardiol 22:798–806
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Managed by Massimo Federici.
The original version of this article was revised: The co-author name “Thozhukat” was misspelled in the original publication and the same is corrected here.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chattopadhyay, S., George, A., John, J. et al. Two-hour post-challenge glucose is a better predictor of adverse outcome after myocardial infarction than fasting or admission glucose in patients without diabetes. Acta Diabetol 55, 449–458 (2018). https://doi.org/10.1007/s00592-018-1114-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1114-2