Abstract
Purpose
To investigate the normative value of distance between the spinous processes (inter-spinous process distance, ISPD), correlations between patients’ demographics and ISPD, and determine cutoff ISPD values that result in segmental lordosis in posterior cervical-thoracic arthrodesis with instrumentation.
Methods
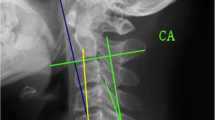
We reviewed patients with visible lower cervical and cervicothoracic spinous processes (C5-T2) on dynamic X-rays. Radiographic measurements included segmental Cobb angles (S-Cobb) and ISPD, defined as the distance between midpoints of the spinous processes. Correlations between patient demographics and ISPD were evaluated. In addition, the cutoff ISPD values that predict segmental lordosis (S-Cobb < 0°) were determined using the receiver operating characteristics (ROC) curve and linear regression model.
Results
We evaluated a total of 153 films on 51 patients. The mean ISPDs in neutral position were 16.0, 20.7, 23.2, and 26.0 mm at C5/6, C6/7, C7/T1, and T1/T2, respectively There were no or only weak correlations between ISPD and age, race, height, body weight, and BMI. We observed significant difference between male and female ISPDs at C7/T1 and T1/T2 (P < 0.05). The ISPDs had moderate/strong correlations with S-Cobb at each segment (− 0.450 ≤ r ≤ − 0.705). Based on the ROC curves, the following cutoff values of ISPD provided 100% positive predictive value for segmental lordosis: < 10 mm at C5-6; < 15 mm at each level from C6 to T2.
Conclusion
ISPD is a simple and useful parameter that correlates with the segmental Cobb angle. During posterior cervical deformity surgery, surgeons can intraoperatively predict adequate segmental lordosis by utilizing the vertebral level specific cutoff values of ISPD.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
References
Lehman RA Jr, Angevine P, Rhim SC, Riew KD (2006) Iatrogenic cervical deformity. Neurosurg Clin N Am 17:247–261, vi. https://doi.org/10.1016/j.nec.2006.05.001
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-part 3: posterior techniques, clinical outcome, and complications. Neurosurgery 81:893–898. https://doi.org/10.1093/neuros/nyx477
Naidich JB, Naidich TP, Garfein C, Liebeskind AL, Hyman RA (1977) The widened interspinous distance: a useful sign of anterior cervical dislocation in the supine frontal projection. Radiology 123:113–116. https://doi.org/10.1148/123.1.113
Pennecot GF, Leonard P, Peyrot Des Gachons S, Hardy JR, Pouliquen JC (1984) Traumatic ligamentous instability of the cervical spine in children. J Pediatr Orthop 4:339–345
Cannada LK, Scherping SC, Yoo JU, Jones PK, Emery SE (2003) Pseudoarthrosis of the cervical spine: a comparison of radiographic diagnostic measures. Spine 28:46–51. https://doi.org/10.1097/01.brs.0000038157.49250.59
Song KS, Piyaskulkaew C, Chuntarapas T, Buchowski JM, Kim HJ, Park MS, Kang H, Riew KD (2014) Dynamic radiographic criteria for detecting pseudarthrosis following anterior cervical arthrodesis. J Bone Joint Surg Am 96:557–563. https://doi.org/10.2106/jbjs.m.00167
Jones EL, Heller JG, Silcox DH, Hutton WC (1997) Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine 22:977–982
Kothe R, Ruther W, Schneider E, Linke B (2004) Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine 29:1869–1875
Neumann P, Wang Y, Karrholm J, Malchau H, Nordwall A (1999) Determination of inter-spinous process distance in the lumbar spine. Evaluation of reference population to facilitate detection of severe trauma. Eur Spine J 8:272–278
Yao Q, Wang S, Shin JH, Li G, Wood K (2013) Motion characteristics of the lumbar spinous processes with degenerative disc disease and degenerative spondylolisthesis. Eur Spine J 22:2702–2709. https://doi.org/10.1007/s00586-013-2918-y
Tozawa R, Katoh M, Aramaki H, Kumamoto T, Fujinawa O (2015) Reliability and validity of an ultrasound-based imaging method for measuring interspinous process distance in the lumbar spine using two different index points. J Phys Ther Sci 27:2333–2336. https://doi.org/10.1589/jpts.27.2333
Ihm EH, Han IB, Shin DA, Kim TG, Huh R, Chung SS (2013) Spinous process morphometry for interspinous device implantation in Korean patients. World Neurosurg 79:172–176. https://doi.org/10.1016/j.wneu.2011.04.027
Jackson ER, Lador R, Ben-Galim PJ, Reitman CA, Hipp JA (2011) Reference data for interpreting widening between spinous processes in the lumbar spine. Spine J 11:336–339. https://doi.org/10.1016/j.spinee.2011.02.005
Kwon B, Kim DH, Marvin A, Jenis LG (2005) Outcomes following anterior cervical discectomy and fusion: the role of interbody disc height, angulation, and spinous process distance. J Spinal Disord Tech 18:304–308
Eubanks AC, Hipp JA, Lador R, Ben-Galim PJ, Reitman CA (2010) Reference data for assessing widening between spinous processes in the cervical spine and the responsiveness of these measures to detecting abnormalities. Spine J 10:230–237. https://doi.org/10.1016/j.spinee.2009.12.025
Greiner TM (2017) Shape analysis of the cervical spinous process. Clin Anat (New York, NY) 30:894–900. https://doi.org/10.1002/ca.22948
Bernhardt M, Bridwell KH (1989) Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine 14:717–721
Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22:1472–1480 (discussion 1480)
Tamai K, Romanu J, Grisdela P Jr, Paholpak P, Zheng P, Nakamura H, Buser Z, Wang JC (2018) Small C7-T1 lordotic angle and muscle degeneration at C7 level were independent radiological characteristics of patients with cervical imbalance: a propensity score-matched analysis. Spine J. https://doi.org/10.1016/j.spinee.2018.01.012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of Columbia University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shimizu, T., Pongmanee, S. & Riew, K.D. Inter-spinous process distance: a novel parameter predicting segmental lordosis during posterior cervical spine deformity surgery. Eur Spine J 28, 1192–1199 (2019). https://doi.org/10.1007/s00586-019-05922-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05922-5