Abstract
Purpose
The objective of this retrospective chart and radiographic review was to present the clinical outcomes and complication rate of a staged approach to modern dual growing-rod (GR) surgery when treating children with severe early onset scoliosis.
Methods
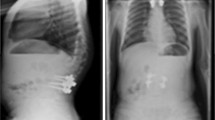
Fifteen patients received a 6-mm dual GR system. During Stage 1, pairs of end vertebra were exposed in a subperiosteal fashion, instrumented, grafted, and fused. Stage 2 was performed, on average, 5 months later (range 8–35 weeks) and the fused foundations were connected with two growing rods under skull-femoral traction. Clinical and operative notes were reviewed and all complications were recorded. Radiographic measurements were assessed at pre-index, with intraoperative traction during Stage 1, post-Stage 2 and at most recent follow-up. Statistical analyses were performed to evaluate change in scoliosis and kyphosis.
Results
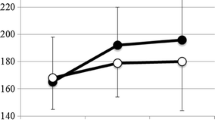
At initial surgery, the average age was 8.17 ± 1.5 years. The mean Cobb angle was 88.1° ± 14.0°, corrected to 60.3° ± 8.7° (p < 0.001) with intraoperative traction in Stage 1, preserved after Stage 2 instrumentation (59.5° ± 9.6°, p = 0.69), and maintained with subsequent lengthenings (60.6° ± 12.8°, p = 0.73). Hyperkyphosis (11/15 patients) improved from 70.8° ± 15.7° to 46.6° ± 9.7° (p < 0.001). At minimum 2-year follow-up (range 24–80 months, mean 49.5), the complication rate was 14 (0.93 complications/patient), including 6 rod breakages, 6 superficial infections, and 2 deep infections. No anchor migration or pull-out was noted. Seven patients have undergone definitive posterior spinal fusion.
Conclusions
Staged insertion of dual GR systems permits strong distraction, with acceptable correction of severe deformities and minimal complications.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.





Similar content being viewed by others
References
Akbarnia B, Marks D, Boachie-Adjei O, Thompson A, Asher M (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine (Phila Pa 1976) 30:S46–S57
Akbarnia B, Breakwell L, Marks D, McCarthy R, Thompson A, Canale S, Kostial P, Tambe A, Asher M, Growing Rod Study Group (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine (Phila Pa 1976) 33:984–990. https://doi.org/10.1097/brs.0b013e31816c8b4e
Olgun Z, Ahmadiadli H, Alanay A, Yazici M (2012) Vetebral body growth during rod instrumentation: growth preservation or stimulation? J Pediatr Orthop 32:184–189. https://doi.org/10.1097/BPO.0b013e3182471915
Yazici M, Olgun Z (2013) Growing rod concepts: state of the art. Eur Spine J Suppl 2:S118–S130. https://doi.org/10.1007/s00586-012-2327-7
Dede O, Demirkiran G, Yazici M (2014) 2014 Update on the ‘growing spine surgery’ for young children with scoliosis. Curr Opin Pediatr 26:57–63. https://doi.org/10.1097/MOP.0000000000000036
Bess S, Akbarnia B, Thompson G, Sponseller P, Shah S, El Sebaie H, Boachie-Adjei O, Karlin L, Canale S, Poe-Kochert C, Skaggs D (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Jt Surg Am 92:2533–2543
Watanabe K, Uno K, Suzuki T, Kawakami N, Tsuiji T, Yanagida H, Ito M, Hirano T, Yamazaki K, Minami S, Kotani T, Taneichi H, Imagama S, Takeshita K, Yamamoto T, Matsumoto M (2013) Risk factors for complications associated with growing rod surgery for early-onset scoliosis. Spine (Phila Pa 1976) 38:E464–E468
Liang J, Li S, Xu D, Zhuang Q, Ren Z, Chen X, Gao N (2015) Risk factors for predicting complications associated with growing rod surgery for early-onset scoliosis. Clin Neurol Neurosurg 136:15–19. https://doi.org/10.1016/j.clineuro.2015.05.026
Sankar W, Acevedo D, Skaggs D (2010) Comparison of complications among growing spinal implants. Spine (Phila Pa 1976) 35:2091–2096. https://doi.org/10.1097/brs.0b013e3181c6edd7
Mahar A, Bagheri R, Oka R, Kostial P, Akbarnia B (2008) Biomechanical comparison of different anchors (foundations) for the pediatric dual growing rod technique. Spine J 8:933–939
Jain S, Modi H, Suh S, Yang J, Hong J (2009) Pedicle shifting or migration as one of the causes of curve progression after posterior fusion: an interesting case report and review of literature. J Pediatr Orthop 18:369–374. https://doi.org/10.1097/BPB.0b013e32832f59b0
Zhou X, Zhang H, Sucato D, Johnston C (2014) Effect of dual screws across the vertebral neurocentral synchondrosis on spinal canal development in an immature spine: a porcine model. J Bone Jt Surg Am 96:e146. https://doi.org/10.2106/JBJS.M.01365
Marchetti P, Faldini A (1978) End fusions in the treatment of some progressing or severe scoliosis in childhood or early adolescence. Orthop Trans 2:271–275
Moe J, Kharrat K, Winter R, Cummine J (1984) Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop Relat Res 185:35–45
R Core Team. R: a language and environment for statistical computing. (2014) R Foundation for Statistical Computing. http://www.R-project.org. Accessed 30 Aug 2017
Kabirian N, Akbarnia B, Pawelek J, Alam M, Mundis G Jr, Acacio R, Thompson G, Marks D, Gardner A, Sponseller P, Skaggs D, Growing Spine Study Group (2014) Deep surgical site infection following 2344 growing-rod procedures for early-onset scoliosis: risk factors and clinical consequences. J Bone Jt Surg Am 96:e128
Zeller R, Ghanem I, Miladi L, Dubousset J (1994) Posterior spinal fusion in neuromuscular scoliosis using a tibial strut graft. Spine (Phila Pa 1976) 19:1628–1631
Schroerlucke S, Akbarnia B, Pawelek J, Salari P, Mundis G Jr, Yazici M, Emans J, Sponseller P, Growing Spine Study Group (2012) How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine 37:1303–1309. https://doi.org/10.1097/brs.0b013e318246d8a0
Yang J, McElroy M, Akbarnia B, Salari P, Oliveira D, Thompson G, Emans J, Yazici M, Skaggs D, Shah S, Kostial P, Sponseller P (2010) Growing rods for spinal deformity: characterizing consensus and variation in current use. J Pediatr Orthop 30:264–270. https://doi.org/10.1097/BPO.0b013e3181d40f94
Oetgen M, Blakemore L (2012) Growing rods in early-onset scoliosis. Semin Spine Surg 24:155–163
Hu H, Hui H, Zhang H, Huang D, Liu Z, Zhao Y, He S, Zhang X, He B, Hao D (2016) The impact of posterior temporary internal distraction on stepwise corrective surgery for extremely severe and rigid scoliosis greater than 130°. Eur Spine J 25:557–568. https://doi.org/10.1007/s00586-015-4013-2
Rushton P, Siddique I, Crawford R, Birch N, Gibson MJ, Hutton MJ (2017) Magnetically controlled growing rods in the treatment of early-onset scoliosis. Bone Joint J 99-B:708–712. https://doi.org/10.1302/0301-620x.99b6
Thompson W, Thakar C, Rolton D, Wilson-MacDonald J, Nnadi C (2016) The use of magnetically-controlled growing rods to treat children with early-onset scoliosis; early radiological results in 19 children. Bone Joint J 98-B:1240–1247. https://doi.org/10.1302/0301-620x.98b9.37545
Hosseini P, Pawelek J, Mundis G, Yaszay B, Ferguson J, Helenius I, Cheung K, Demirkiran G, Alanay A, Senkoylu A, Elsebaie H, Akbarnia B (2016) Magnetically controlled growing rods for early-onset scoliosis: a multicenter study of 23 cases with minimum 2 years follow-up. Spine (Phila PA 1976) 41:1456–1462. https://doi.org/10.1097.0000000000001561
Rolton D, Thakar C, Wilson-MacDonald J, Nnadi C (2016) Radiological and clinical assessment of the distraction achieved with remotely exandable growing rods in early onset scoliosis. Eur Spine J 25:3371–3376. https://doi.org/10.1007/s00586-015-4223-4
Teoh K, Winson D, James S, Jones A, Howes J, Davies P, Ahuja S (2016) Magnetic controlled growing rods for early-onset scoliosis: a 4-year follow-up. Spine J 16:S34–S39
Gomez J, Grzywna A, Hanstein R, Emans J, Hresko M, Hedequist D, Karlin L, Glotzbecker M (2017) Staged growing rods with preimplantation of spinal anchors for complex early onset scoliosis. J Pediatr Orthop 37:e606–e611. https://doi.org/10.1097/BPO.0000000000000957
Shah S, Karatas A, Dhawale A, Dede O, Mundis G Jr, Holmes L Jr, Yorgova P, Neiss G, Johnston C, Emans J, Thompson G, Pawelek J, Akbarnia B, Growing Spine Study Group (2014) The effect of serial growing rod lengthening on the sagittal profile and pelvic parameters in early-onset scoliosis. Spine (Phila Pa 1976) 39:e1311–e1317. https://doi.org/10.1097/brs.0000000000000565
Sankar W, Skaggs D, Yazici M, Johnston C, Shah S, Javidan P, Kadakia R, Day T, Akbarnia B (2011) Lengthening of dual growing rods and the law of diminishing returns. Spine (Phila Pa 1976) 36:806–809. https://doi.org/10.1097/brs.0b013e318214d78f
Noordeen H, Shah S, Elsebaie H, Garrido E, Farooq N, Al-Mukhtar M (2001) In vivo distraction force and length measurements of growing rods: which factors influence the ability to lengthen? Spine (Phila Pa 1976) 36:2299–2303. https://doi.org/10.1097/brs.0b013e31821b8e16
Flynn J, Tomlinson L, Pawelek J, Thompson G, McCarthy R, Akbarnia B, Growing Spine Study Group (2013) Growing-rod graduates: lessons learned from ninety-nine patients who completed lengthening. J Bone Jt Surg Am 95:1745–1750. https://doi.org/10.2106/jbjs.l.01386
Yang J, Sponseller P, Thompson G, Akbarnia B, Emans J, Yazici M, Skaggs D, Shah S, Salari P, Poe-Kochert C, Growing Rod Study Group (2011) Growing rod fractures: risk factors and opportunities for prevention. Spine (Phila Pa 1976) 36:1639–1644. https://doi.org/10.1097/brs.0b013e31822a982f
Mineiro J, Weinstein S (2002) Subcutaneous rodding for progressive spinal curvatures: early results. J Pediatr Orthop 22:290–295
Acaroglu E, Yazici M, Alanay A, Surat A (2002) Three-dimensional evolution of scoliotic curve during instrumentation without fusion in young children. J Pediatr Orthop 22:492–496
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Zeller receives royalties from Spinevision (excluding personal use) and is an unpaid consultant for Paradigm Spine. None of the authors has received any grant or financial support for the present study.
Additional information
At the time this study was conducted Sebastiaan Schelfaut was an Orthopaedic Fellow at the Hospital for Sick Children, Toronto, ON, Canada.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schelfaut, S., Dermott, J.A. & Zeller, R. Staged insertion of growing rods in severe scoliosis. Eur Spine J 27, 2203–2212 (2018). https://doi.org/10.1007/s00586-018-5552-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5552-x