Abstract
Purpose
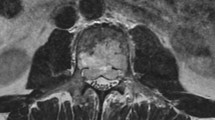
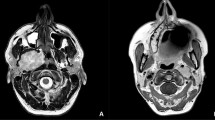
Cervicothoracic paravertebral neoplasms extending into the mediastinum pose a surgical challenge due the complex regional anatomy, their biological nature, rarity and surgeon’s unfamiliarity with the region. We aim to define a surgical access framework addressing the aforementioned complexities whilst achieving oncological clearance.
Methods
We carried out a retrospective review of 28 consecutive patients operated in two tertiary referral centres between 1998 and 2015. Pathology was located paravertebrally from C6 to T4 with superior mediastinum invasion. Patients were operated jointly by a spinal and a thoracic surgeon.
Results
Tumours were classified according to subclavian fossa involvement as anteromedial, anterolateral and posterior and according to histology in benign nerve sheath tumour group (n = 10) and malignant bone or soft tissue tumours (n = 18). Three surgical routes were utilised: (1) median sternotomy (n = 11), (2) anterior cervical transsternal approach (n = 7) and (3) high posterolateral thoracotomy (n = 10). Resection was en bloc with wide margins in 22 cases, marginally complete in 3 and incomplete in 3. Complications included Horner’s syndrome (n = 3), infection (n = 2) and transient neurological deficit (n = 4). In the nerve sheath tumour group, no recurrence or reoperation took place with a median follow-up of 4.5 years. In the malignant bone and soft tissue group, 96% of the patients were alive at 1 year, 67% at 2 years and 33% at 5 years. No vascular injuries or operative related deaths were observed.
Conclusions
Classification of cervicothoracic paravertebral neoplasms with mediastinal extension according to the relationship with the subclavicular fossa and dual speciality involvement allows for a structured surgical approach and provides minimal morbidity/maximum resection and satisfactory oncological outcomes.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.






Similar content being viewed by others
References
Birch R, Bonney G, Marshall RW (1990) A surgical approach to the cervicothoracic spine. J Bone Jt Surg Br 72:904–907
Cauchoix J, Binet JP (1957) Anterior surgical approaches to the spine. Ann R Coll Surg Engl 21:237–243
Dartevelle PG, Chapelier AR, Macchiarini P, Lenot B, Cerrina J, Ladurie FL, Parquin FJ, Lafont D (1993) Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025–1034
Grunenwald D, Spaggiari L (1997) Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 63:563–566
Ladas G, Rhys-Evans PH, Goldstraw P (1999) Anterior cervical–transsternal approach for resection of benign tumors at the thoracic inlet. Ann Thorac Surg 67:785–789
Mazel C, Grunenwald D, Laudrin P, Marmorat JL (2003) Radical excision in the management of thoracic and cervicothoracic tumors involving the spine: results in a series of 36 cases. Spine 28:782–792
Panagopoulos N, Livaditis V, Koletsis E, Alexopoulos P, Prokakis C, Baltayiannis N, Hatzimichalis A, Tsakiridis K, Zarogoulidis P, Zarogoulidis K, Katsikogiannis N, Kougioumtzi I, Machairiotis N, Tsiouda T, Machairiotis N, Madesis A, Vretzakis G, Kolettas A, Dougenis D (2014) Therapeutic modalities for Pancoast tumors. J Thorac Dis 6(Suppl 1):S180–S193
Shaw RR, Paulson DL, Kee JL (1961) Treatment of superior sulcus tumor by irradiation followed by resection. Ann Surg 154:29–40
Yamazaki T, McLoughlin GS, Patel S, Rhines LD, Fourney DR (2009) Feasibility and safety of en bloc resection for primary spine tumors: a systematic review by the Spine Oncology Study Group. Spine 34:S31–S38
Talac R, Yaszemski MJ, Currier BL, Fuchs B, Dekutoski MB, Kim CW, Sim FH (2002) Relationship between surgical margins and local recurrence in sarcomas of the spine. Clin Orthop Relat Res 397:127–132
Boriani S, Saravanja D, Yamada Y, Varga PP, Biagini R, Fisher CG (2009) Challenges of local recurrence and cure in low grade malignant tumors of the spine. Spine 34:S48–S57
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prezerakos, G.K., Sayal, P., Kourliouros, A. et al. Paravertebral tumours of the cervicothoracic junction extending into the mediastinum: surgical strategies in a no man’s land. Eur Spine J 27, 902–912 (2018). https://doi.org/10.1007/s00586-018-5512-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5512-5