Abstract
Background
The prevalence of cervical block vertebrae is unknown. Furthermore, there is no consensus on the cause of adjacent segment degeneration (ASD) after cervical fusion.
Questions/purposes
(1) What is the incidence of cervical block vertebrae? Is there a gender difference? (2) Among cervical block vertebrae cases, is ASD related to age and segment? And what is the specific relationship? (3) What are the imaging findings and characteristics of this disease?
Patients and methods
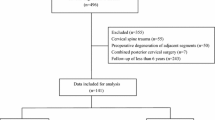
We retrospectively diagnosed cervical block vertebrae cases with bony fusions in any segments of the cervical spine without intervertebral fusion surgery of 33,762 patients reported from 2006 to 2011 in north China. Then the X-ray of the obtained cases were observed and counted. The primary outcome was incidence of ASD according to age and segment. The secondary outcome measures were C2–7 angle in fusion (single segment fusion of lower cervical vertebra) and control groups (randomly selected cases of non-fusion), Cobb’s angle of fusion segments, and curvature of each lower cervical segment in the control group.
Results
A total of 218 cervical block vertebrae cases were found, with a incidence of 0.65%, and C2–3 represented the highest number of fusion segment cases. There were no significant differences in the incidence by sex. Varying degrees of degeneration in the adjacent segment was present in 112 cases (51.4%). The incidence of ASD increased with age, with the ASD growth rate reaching its peak at the age of 51–60 years (55.08%). Cervical curvature shows no significant difference between patients with cervical block vertebrae and normal individuals. The segmental curvature was lower in the fusion group than in the control group, with statistical significance achieved in fusion segments located in C4–5, C5–6, and C6–7, but not C3–4.
Conclusions
Fusion segments located in C4–5, C5–6, and C6–7 are more prone to ASD than C3–4. The incidence of ASD in patients with vertebral fusion increases with age.
Level of evidence
III.



Similar content being viewed by others
References
Mcmaster MJ, Ohtsuka K (1982) The natural history of congenital scoliosis. A study of two hundred and fifty-one patients. J Bone Jt Surg Am 64(8):1128–1147
Mcmaster MJ, Singh H (1999) Natural history of congenital kyphosis and kyphoscoliosis. A study of one hundred and twelve patients. J Bone Jt Surg Am 81(10):1367–1383
Shands AR Jr, Eisberg HB (1955) The incidence of scoliosis in the state of Delaware; a study of 50,000 minifilms of the chest made during a survey for tuberculosis. J Bone Jt Surg Am 37-A(6):1243–1249
Wynne-Davies R (1975) Congenital vertebral anomalies: etiology and relationship to spina bifida cystica. J Med Genet 12(3):280–288
Hutchinson J (1894) Deformity of shoulder girdle. Br Med J 1:669–673
Clarke JJ (1906) A note on a case of congenital deformity of the spine. Am J Orthop Surg 24(2):160–162
Bayrakli F, Guclu B, Yakicier C et al (2013) Mutation in MEOX1 gene causes a recessive Klippel–Feil syndrome subtype. BMC Genet 14:95
Duncan PA (1977) Embryologic pathogenesis of renal agenesis associated with cervical vertebral anomalies (Klippel–Feil phenotype). Birth Defects Orig Artic Ser 13(3D):91–101
Basu SN (1961) Klippel–Feil syndrome. Indian J Pediatr 28:57
Gunderson CH, Greenspan RH, Glaser GH, Lubs HA (1967) The Klippel–Feil syndrome: genetic and clinical reevaluation of cervical fusion. Medicine (Baltimore) 46(6):491–512
Michie I, Clark M (1968) Neurological syndromes associated with cervical and craniocervical anomalies. Arch Neurol 18(3):241–247
Mosberg WH Jr (1953) The Klippel–Feil syndrome; etiology and treatment of neurologic signs. J Nerv Ment Dis 117:479–491
Shoul MI, Ritvo M (1952) Clinical and roentgenological manifestations of the Klippel–Feil syndrome (congenital fusion of the cervical vertebrae, brevicollis); report of eight additional cases and review of the literature. Am J Roentgenol Radium Ther Nucl Med 68(3):369–385
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15(6):602–617
Robinson RA, Smith GW (1955) Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp 5(96):223–224
Lund T, Oxland TR (2011) Adjacent level disk disease—is it really a fusion disease? Orthop Clin N Am 42(4):529–541
Chung JY, Kim SK, Jung ST, Lee KB (2014) Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J 14(10):2290–2298
Papanastassiou ID, Baaj AA, Dakwar E, Eleraky M, Vrionis FD (2011) Failure of cervical arthroplasty in a patient with adjacent segment disease associated with Klippel–Feil syndrome. Indian J Orthop 45(2):174–177
Falk RH, Mackinnon J (1976) Klippel–Feil syndrome associated with aortic coarctation. Heart 38(11):1220–1221
Li JX, Sun DY (1982) X-ray diagnostics. People’s Medical Publishing House, Beijing, pp 69–70
Brown MW, Templeton AW, Hodges FJ 3rd (1964) The incidence of acquired and congenital fusions in the cervical spine. Am J Roentgenol Radium Ther Nucl Med. 92:1255–1259
Gray SW, Romaine CB, Skandalakis JE (1964) Congenital fusion of the cervical vertebrae. Surg Gynecol Obstet 118:373–385
Lee CK, Weiss AB (1981) Isolated congenital cervical block vertebrae below the axis with neurological symptoms. Spine 2:118–124
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y et al (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 35(1):36–43
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Jt Surg Am 81(4):519–528
Karasick D, Schweitzer ME, Vaccaro AR (1998) The traumatized cervical spine in Klippel–Feil syndrome: imaging features. AJR Am J Roentgenol 170(1):85–88
Schwab JS, Diangelo DJ, Foley KT (2006) Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine (Phila Pa 1976) 31(21):2439–2448
Yi S, Kim SH, Shin HC, Kim KN, Yoon DH (2007) Cervical arthroplasty in a patient with Klippel–Feil syndrome. Acta Neurochir (Wien) 149(8):805–809
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Informed consent
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Rights and permissions
About this article
Cite this article
Ma, X., Du, Y., Wang, S. et al. Adjacent segment degeneration after intervertebral fusion surgery by means of cervical block vertebrae. Eur Spine J 27, 1401–1407 (2018). https://doi.org/10.1007/s00586-017-5371-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5371-5