Abstract
Purpose
Lumbar central spinal stenosis (LSS) is one of the most common reasons for spine surgery in the elderly patient. Magnetic resonance imaging (MRI) represents the gold standard for the assessment of LSS and can be used to obtain quantitative measures of the dural sac cross-sectional area (DCSA) or qualitative measures (morphological grades A–D) of the rootlet/cerebrospinal fluid ratio. This study investigated the intercorrelation between these two MRI evaluation methods and explored their respective relationships with the patient baseline clinical status and outcome 12 months after surgery.
Methods
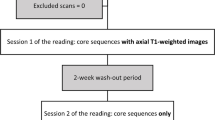
This was a retrospective analysis of prospectively collected data from 157 patients (88 male, 69 female; age 72 ± 7 years) who were undergoing first-time surgery for LSS. Patients with foraminal or isolated lateral stenosis were excluded. The Core Outcome Measures Index (COMI) was completed before and 12 months after surgery. Preoperative T2 axial MRIs were blinded and independently evaluated for DCSA and morphological grade. Spearman rank correlation coefficients described the relationship between the two MRI measures of stenosis severity and between each of these and the COMI baseline and change-scores (pre to 12 months’ postop). Multiple logistic regression analysis (controlling for baseline COMI, age, gender, number of operated levels, health insurance status) was used to analyse the influence of stenosis severity on the achievement of the minimum clinically important change (MCIC) score for COMI and on global treatment outcome (GTO).
Results
There was a correlation of ρ = −0.69 (p < 0.001) between DCSA and morphological grade. There was no significant correlation between COMI baseline scores and either DCSA or morphological grades (p > 0.85). However, logistic regression revealed significant (p < 0.05) associations between stenosis ratings and 12-month outcome, whereby patients with more severe stenosis (as measured using either of the methods) benefited more from the surgery. Patients with a DCSA <75 mm2 or morphological grade D had a 4–13-fold greater odds of achieving the MCIC for COMI or a “good” GTO, compared with patients in the least severe categories of stenosis.
Conclusions
Postoperative outcome was clearly related to the degree of preoperative radiological LSS. The two MRI methods appeared to deliver similar information, as given by the relatively strong correlation between them and their comparable performance in relation to baseline and 12-month outcomes. However, the qualitative morphological grading can be performed in an instant, without measurement tools, and does not deliver less clinically useful information than the more complex and time-consuming measures; as such, it may represent the preferred method in the clinical routine for assessing the extent of radiological stenosis and the likelihood of a positive outcome after decompression.

(reproduced with permission from Wolters Kluwer Health, Inc.)





Similar content being viewed by others
References
Ciol MA, Deyo RA, Howell E, Kreif S (1996) An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc 44:285–290
Turner JA, Ersek M, Herron L, Deyo R (1992) Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine 17:1–8
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303:1259–1265. doi:10.1001/jama.2010.338
Aalto TJ, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, Kroger H, Andrade J, Jimenez R, Tapaninaho A, Turunen V, Savolainen S, Airaksinen O (2006) Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine 31:E648–E663
Mannion AF, Elfering A (2008) Predictors of surgical outcome. In: Boos N, Aebi M (eds) Spinal Disorders. Springer, Berlin
Tomkins-Lane C, Melloh M, Lurie J, Smuck M, Battie MC, Freeman B, Samartzis D, Hu R, Barz T, Stuber K, Schneider M, Haig A, Schizas C, Cheung JP, Mannion AF, Staub L, Comer C, Macedo L, Ahn SH, Takahashi K, Sandella D (2016) ISSLS Prize Winner: consensus on the clinical diagnosis of lumbar spinal stenosis: results of an International Delphi Study. Spine (Phila Pa 1976) 41:1239–1246. doi:10.1097/BRS.0000000000001476
Andreisek G, Hodler J, Steurer J (2011) Uncertainties in the diagnosis of lumbar spinal stenosis. Radiology 261:681–684. doi:10.1148/radiol.11111086
Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, Kulik G (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 35:1919–1924. doi:10.1097/BRS.0b013e3181d359bd
Marawar SV, Ordway NR, Madom IA, Tallarico RA, Palumbo M, Metkar U, Wang D, Huang D, Lavelle WF (2016) Comparison of surgeon rating of severity of stenosis using magnetic resonance imaging, dural cross-sectional area, and functional outcome scores. World Neurosurg 96:165–170. doi:10.1016/j.wneu.2016.08.093
Burgstaller JM, Schuffler PJ, Buhmann JM, Andreisek G, Winklhofer S, Del Grande F, Mattle M, Brunner F, Karakoumis G, Steurer J, Held U, Group LS (2016) Is there an association between pain and magnetic resonance imaging parameters in patients with lumbar spinal stenosis? Spine (Phila Pa 1976) 41:E1053–E1062. doi:10.1097/BRS.0000000000001544
Goni VG, Hampannavar A, Gopinathan NR, Singh P, Sudesh P, Logithasan RK, Sharma A, Bk S, Sament R (2014) Comparison of the Oswestry Disability Index and magnetic resonance imaging findings in lumbar canal stenosis: an observational study. Asian Spine J 8:44–50. doi:10.4184/asj.2014.8.1.44
Hong JH, Lee MY, Jung SW, Lee SY (2015) Does spinal stenosis correlate with MRI findings and pain, psychologic factor and quality of life? Korean J Anesthesiol 68:481–487. doi:10.4097/kjae.2015.68.5.481
Kuittinen P, Sipola P, Saari T, Aalto TJ, Sinikallio S, Savolainen S, Kroger H, Turunen V, Leinonen V, Airaksinen O (2014) Visually assessed severity of lumbar spinal canal stenosis is paradoxically associated with leg pain and objective walking ability. BMC Musculoskelet Disord 15:348. doi:10.1186/1471-2474-15-348
Lohman CM, Tallroth K, Kettunen JA, Lindgren KA (2006) Comparison of radiologic signs and clinical symptoms of spinal stenosis. Spine (Phila Pa 1976) 31:1834–1840. doi:10.1097/01.brs.0000227370.65573.ac
Kim HJ, Suh BG, Lee DB, Lee GW, Kim DW, Kang KT, Chang BS, Lee CK, Yeom JS (2013) The influence of pain sensitivity on the symptom severity in patients with lumbar spinal stenosis. Pain Physician 16:135–144
Moojen WA, Schenck CD, Nijeholt GJ, Jacobs WC, Van der Kallen BF, Arts MP, Peul WC, Vleggeert-Lankamp CL (2015) Preoperative MR imaging in patients with intermittent neurogenic claudication: relevance for diagnosis and prognosis. Spine (Phila Pa 1976). doi:10.1097/brs.0000000000001301
Kim YU, Kong YG, Lee J, Cheong Y, Kim S, Kim HK, Park JY, Suh JH (2015) Clinical symptoms of lumbar spinal stenosis associated with morphological parameters on magnetic resonance images. Eur Spine J 24:2236–2243. doi:10.1007/s00586-015-4197-2
Weber C, Giannadakis C, Rao V, Jakola AS, Nerland U, Nygaard OP, Solberg TK, Gulati S, Solheim O (2016) Is there an association between radiological severity of lumbar spinal stenosis and disability, pain, or surgical outcome?: a multicenter observational study. Spine (Phila Pa 1976) 41:E78–E83. doi:10.1097/BRS.0000000000001166
Sigmundsson FG, Kang XP, Jonsson B, Stromqvist B (2011) Correlation between disability and MRI findings in lumbar spinal stenosis: a prospective study of 109 patients operated on by decompression. Acta Orthop 82:204–210. doi:10.3109/17453674.2011.566150
Sirvanci M, Bhatia M, Ganiyusufoglu KA, Duran C, Tezer M, Ozturk C, Aydogan M, Hamzaoglu A (2008) Degenerative lumbar spinal stenosis: correlation with Oswestry Disability Index and MR imaging. Eur Spine J 17:679–685. doi:10.1007/s00586-008-0646-5
Weiner BK, Patel NM, Walker MA (2007) Outcomes of decompression for lumbar spinal canal stenosis based upon preoperative radiographic severity. J Orthop Surg Res 2:3. doi:10.1186/1749-799X-2-3
Yukawa Y, Lenke LG, Tenhula J, Bridwell KH, Riew KD, Blanke K (2002) A comprehensive study of patients with surgically treated lumbar spinal stenosis with neurogenic claudication. J Bone Jt Surg 84-a:1954–1959 (American volume)
Azimi P, Benzel EC, Shahzadi S, Azhari S, Mohmmadi H (2017) Decision making process in patients with lumbar spinal canal stenosis. J Neurosurg Sci 61:388–394
Azimi P, Mohamed HR, Aghaei HN, Mohseni M (2013) Outcomes of patients diagnosed with lumbar spinal stenosis undergoing laminectomy based on the morphology of the dural sac on MRI. Res Med 36:183–188
Kuittinen P, Sipola P, Leinonen V, Saari T, Sinikallio S, Savolainen S, Kroger H, Turunen V, Airaksinen O, Aalto T (2014) Preoperative MRI findings predict two-year postoperative clinical outcome in lumbar spinal stenosis. PLoS One 9:e106404. doi:10.1371/journal.pone.0106404
Sigmundsson FG, Kang XP, Jonsson B, Stromqvist B (2012) Prognostic factors in lumbar spinal stenosis surgery. Acta Orthop 83:536–542. doi:10.3109/17453674.2012.733915
Steurer J, Nydegger A, Held U, Brunner F, Hodler J, Porchet F, Min K, Mannion AF, Michel B (2010) LumbSten: the lumbar spinal stenosis outcome study. BMC Musculoskelet Disord 11:254. doi:10.1186/1471-2474-11-254
Deyo RA, Battie M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23:2003–2013
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14:1014–1026
Mannion AF, Porchet F, Kleinstück F, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 1. The Core Outcome Measures Index (COMI) in clinical practice. Eur Spine J 18:367–373
Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R (2006) Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine 31:1372–1379 (discussion 1380)
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur Spine J 18:374–379
Citrome L (2014) Quantifying clinical relevance. Innov Clin Neurosci 11:26–30
Lau YYO, Lee RKL, Griffith JF, Chan CLY, Law SW, Kwok KO (2017) Changes in dural sac caliber with standing MRI improve correlation with symptoms of lumbar spinal stenosis. Eur Spine J. doi:10.1007/s00586-017-5211-7
Ishimoto Y, Yoshimura N, Muraki S, Yamada H, Nagata K, Hashizume H, Takiguchi N, Minamide A, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M (2013) Associations between radiographic lumbar spinal stenosis and clinical symptoms in the general population: the Wakayama Spine Study. Osteoarthr Cartil 21:783–788. doi:10.1016/j.joca.2013.02.656
Barz T, Staub LP, Melloh M, Hamann G, Lord SJ, Chatfield MD, Bossuyt PM, Lange J, Merk HR (2014) Clinical validity of the nerve root sedimentation sign in patients with suspected lumbar spinal stenosis. Spine J 14:667–674. doi:10.1016/j.spinee.2013.06.105
Nerland US, Jakola AS, Giannadakis C, Solheim O, Weber C, Nygaard OP, Solberg TK, Gulati S (2015) The risk of getting worse: predictors of deterioration after decompressive surgery for lumbar spinal stenosis: a multicenter observational study. World Neurosurg 84:1095–1102. doi:10.1016/j.wneu.2015.05.055
Mannion AF, Fekete TF, Wertli MM, Mattle M, Nauer S, Kleinstuck FS, Jeszenszky D, Haschtmann D, Becker HJ, Porchet F, Lumbar Spinal Stenosis Outcome Study G (2015) Could less be more when assessing patient-rated outcome in spinal stenosis? Spine (Phila Pa 1976) 40:710–718. doi:10.1097/BRS.0000000000000751
Pratt RK, Fairbank JCT, Virr A (2002) The reliability of the Shuttle Walking Test, the Swiss Spinal Stenosis Questionnaire, the Oxford Spinal Stenosis Score, and the Oswestry Disability Index in the assessment of patients with lumbar spinal stenosis. Spine 27:84–91
Schizas C, Kulik G (2012) Decision-making in lumbar spinal stenosis: a survey on the influence of the morphology of the dural sac. J Bone Jt Surg Br 94:98–101. doi:10.1302/0301-620X.94B1.27420
Lonne G, Odegard B, Johnsen LG, Solberg TK, Kvistad KA, Nygaard OP (2014) MRI evaluation of lumbar spinal stenosis: is a rapid visual assessment as good as area measurement? Eur Spine J 23:1320–1324. doi:10.1007/s00586-014-3248-4
Henderson L, Kulik G, Richarme D, Theumann N, Schizas C (2012) Is spinal stenosis assessment dependent on slice orientation? A magnetic resonance imaging study. Eur Spine J 21(Suppl 6):S760–S764. doi:10.1007/s00586-011-1857-8
Andreisek G, Deyo RA, Jarvik JG, Porchet F, Winklhofer SF, Steurer J, Group LW (2014) Consensus conference on core radiological parameters to describe lumbar stenosis—an initiative for structured reporting. Eur Radiol 24:3224–3232. doi:10.1007/s00330-014-3346-z
Findlay JM, Deis N (2010) Appropriateness of lumbar spine referrals to a neurosurgical service. Can J Neurol Sci 37:843–848
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mannion, A.F., Fekete, T.F., Pacifico, D. et al. Dural sac cross-sectional area and morphological grade show significant associations with patient-rated outcome of surgery for lumbar central spinal stenosis. Eur Spine J 26, 2552–2564 (2017). https://doi.org/10.1007/s00586-017-5280-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5280-7