Abstract
Purpose
Oblique lateral interbody fusion (OLIF) L5–S1 is essentially to perform an anterior lumbar interbody fusion (ALIF) in the lateral position. Because the surgical procedures are performed “obliquely” over the left common iliac vein (LCIV), ensuring that the vein is protected which is particularly important. We aimed to evaluate the configuration of LCIV and its risk of mobilization during anterior approach at L5–S1 segment.
Methods
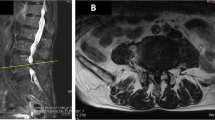
This study involved 65 consecutive patients who underwent anterior lumbar fusion (ALIF, n = 39; OLIF, n = 26) at the L5–S1 segment. Three independent examiners evaluated the configuration of the LCIV at the L5–S1 disc on axial magnetic resonance images of the lumbar spine. The LCIV was categorized into three types according to the difficulty of mobilization: type I (no requirement for mobilization; LCIV runs laterally for more than two-thirds of the length of the left side of the L5–S1 disc), type II (easy mobilization; LCIV obstructs the L5–S1 disc space, but the perivascular adipose tissue is present under the LCIV), and type III (potentially difficult mobilization; no perivascular adipose tissue under the LCIV). The patient records were reviewed for vascular complications.
Results
There were 21 men and 44 women in this study, with a mean age of 63.4 years (range 19–83 years). Type I LCIV configuration was found in 32 (49.2%) patients, type II in 18 (27.7%), and type III in 15 (23.1%). There were 7 (10.8%) patients with LCIV injury (type I, n = 0; type II, n = 2; type III, n = 5) (P = 0.003). Intraobserver reliability for the LCIV classification ranged from substantial to excellent, and interobserver reliability ranged from moderate to excellent.
Conclusions
Preoperative evaluation for anterior approach to the L5–S1 segment should take account of the LCIV position, as well as the difficulty of its mobilization. The type III LCIV configuration showed a high rate of vascular injury.



Similar content being viewed by others
References
Mayer HM (2000) The ALIF concept. Eur Spine J 9(Suppl 1):S35–S43
Brau SA (2002) Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results and complications. Spine J 2:216–223
Hynes R (2014) Oblique lateral interbody fusion (OLIF) technique and complications in 457 levels L1 to S1. In: International Society for the Advancement of Spine Surgery
Davis TT, Hynes RA, Fung DA et al (2014) Retroperitoneal oblique corridor to the L2–S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 21:785–793
Ohtori S, Mannoji C, Orita S et al (2015) Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J 9:565–572
Fujibayashi S, Hynes RA, Otsuki B et al (2015) Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine 40:E175–E182
Abe K, Orita S, Mannoji C et al (2016) Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine 42:55–62
Silvestre C, Mac-Thiong JM, Hilmi R et al (2012) Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J 6:89–97
Wakita H, Shiga Y, Ohtori S et al (2015) Less invasive corrective surgery using oblique lateral interbody fusion (OLIF) including L5–S1 fusion for severe lumbar kyphoscoliosis due to L4 compression fracture in a patient with Parkinson’s disease: a case report. BMC Res Notes 8:126
Capellades J, Pellise F, Rovira A et al (2000) Magnetic resonance anatomic study of iliocava junction and left iliac vein positions related to L5–S1 disc. Spine 25:1695–1700
Datta JC, Janssen ME, Beckham R et al (2007) The use of computed tomography angiography to define the prevertebral vascular anatomy prior to anterior lumbar procedures. Spine 32:113–119
Fantini GA, Pappou IP, Girardi FP et al (2007) Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine 32:2751–2758
Hamdan AD, Malek JY, Schermerhorn ML et al (2008) Vascular injury during anterior exposure of the spine. J Vasc Surg 48:650–654
Tribus CB, Belanger T (2001) The vascular anatomy anterior to the L5–S1 disk space. Spine 26:1205–1208
Mobbs RJ, Phan K, Daly D et al (2016) Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Glob Spine J 6:147–154
Bateman DK, Millhouse PW, Shahi N et al (2015) Anterior lumbar spine surgery: a systematic review and meta-analysis of associated complications. Spine J 15:1118–1132
Quraishi NA, Konig M, Booker SJ et al (2013) Access related complications in anterior lumbar surgery performed by spinal surgeons. Eur Spine J 22(Suppl 1):S16–S20
Jarrett CD, Heller JG, Tsai L (2009) Anterior exposure of the lumbar spine with and without an “access surgeon”: morbidity analysis of 265 consecutive cases. J Spinal Disord Tech 22:559–564
Szasz T, Webb RC (2012) Perivascular adipose tissue: more than just structural support. Clin Sci (Lond, Engl: 1979) 122:1–12
Brown NK, Zhou Z, Zhang J et al (2014) Perivascular adipose tissue in vascular function and disease: a review of current research and animal models. Arterioscler Thromb Vasc Biol 34:1621–1630
Villacorta L, Chang L (2015) The role of perivascular adipose tissue in vasoconstriction, arterial stiffness, and aneurysm. Hormone Mol Biol Clin Investig 21:137–147
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Sasso RC, Best NM, Mummaneni PV et al (2005) Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 30:670–674
Brau SA, Delamarter RB, Schiffman ML et al (2004) Vascular injury during anterior lumbar surgery. Spine J 4:409–412
Garg J, Woo K, Hirsch J et al (2010) Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg 51:946–950 (discussion 50)
Woods KR, Billys JB, Hynes RA (2017) Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17:545–553
Phan K, Maharaj M, Assem Y et al (2016) Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF). J Clin Neurosci 31:23–29
Zhang F, Xu H, Yin B et al (2016) Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. Eur Spine J 26(3):646–650. doi:10.1007/s00586-016-4645-7
Oikawa Y, Eguchi Y, Watanabe A et al (2017) Anatomical evaluation of lumbar nerves using diffusion tensor imaging and implications of lateral decubitus for lateral transpsoas approach. Eur Spine J
Acknowledgements
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chung, NS., Jeon, CH., Lee, HD. et al. Preoperative evaluation of left common iliac vein in oblique lateral interbody fusion at L5–S1. Eur Spine J 26, 2797–2803 (2017). https://doi.org/10.1007/s00586-017-5176-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5176-6