Abstract
Background and purpose
There is a lack of evidence on the broad health-care costs of treating spine trauma patients without neurological deficits conservatively. The aim of the present study was to estimate the primary and secondary health-care sector costs associated with conservative treatment of spine fractures as well as their determinants.
Methods
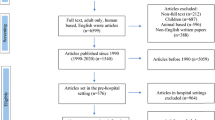
Patients were identified between 1999 and 2008 in the hospital’s administrative system based on relevant diagnostic codes. Inclusion criteria were: (1) spine fractures (C1–L5); (2) age >18; and (3) conservative treatment. Exclusion criteria were: (1) neurological involvement and (2) fractures secondary to osteoporosis/malignancy. Health-care utilization and costs were retrieved from national administrative databases covering the entire health-care sector.
Results
201 cervical, 150 thoracic, and 140 lumbar fracture patients were included in the study. The total health cost was estimated at €18,919 (16,199; 21,756), €8571 (6062; 11,733), €5526 (3473; 7465) for cervical, thoracic, and lumbar regions, respectively. Hospital admissions accounted for the vast majority of costs while primary health care accounted for less than 3 % and prescription medication for less than 2 %. The determinants of costs included fracture site (p < 0.001) and concomitant lower limb injuries (p = 0.009).
Conclusions
Spinal fractures, even mild ones, appear to incur substantial health-care utilization and costs. Health-care costs in conjunction with cervical fractures are more than two-fold of those affiliated with thoracic and lumbar fractures. Among the concomitant injuries, lower limb injuries exert a substantial influence over health-care costs.
Similar content being viewed by others
References
Schoenfeld AJ, Bono CM (2011) Measuring spine fracture outcomes: common scales and checklists. Injury 42:265–270. doi:10.1016/j.injury.2010.11.040
Stadhouder A, Buckens CF, Holtslag HR, Oner FC (2010) Are existing outcome instruments suitable for assessment of spinal trauma patients? J Neurosurg Spine 13:638–647. doi:10.3171/2010.5.SPINE09128
Sørensen HT, Christensen T, Schlosser HK (2009) Use of medical databases in clinical epidemiology. Aarhus University Press, Aarhus
Rivara FP, Mackenzie EJ, Jurkovich GJ, Nathens AB, Wang J, Scharfstein DO (2008) Prevalence of pain in patients 1 year after major trauma. Arch Surg 143:282–287. doi:10.1001/archsurg.2007.61 (discussion 288)
Grotle M, Brox JI, Veierod MB, Glomsrod B, Lonn JH, Vollestad NK (2005) Clinical course and prognostic factors in acute low back pain: patients consulting primary care for the first time. Spine 30:976–982
Atherton K, Wiles NJ, Lecky FE, Hawes SJ, Silman AJ, Macfarlane GJ, Jones GT (2006) Predictors of persistent neck pain after whiplash injury. Emerg Med J EMJ 23:195–201. doi:10.1136/emj.2005.027102
Williamson OD, Epi GD, Gabbe BJ, Physio B, Cameron PA, Edwards ER, Richardson MD, Victorian Orthopaedic Trauma Outcome Registry Project G (2009) Predictors of moderate or severe pain 6 months after orthopaedic injury: a prospective cohort study. J Orthop Trauma 23:139–144. doi:10.1097/BOT.0b013e3181962e29
Von Korff M, Crane P, Lane M, Miglioretti DL, Simon G, Saunders K, Stang P, Brandenburg N, Kessler R (2005) Chronic spinal pain and physical–mental comorbidity in the United States: results from the national comorbidity survey replication. Pain 113:331–339. doi:10.1016/j.pain.2004.11.010
Linton SJ (2000) A review of psychological risk factors in back and neck pain. Spine 25:1148–1156
Holmes A, Williamson O, Hogg M, Arnold C, Prosser A, Clements J, Konstantatos A, O’Donnell M (2010) Predictors of pain 12 months after serious injury. Pain Med 11:1599–1611. doi:10.1111/j.1526-4637.2010.00955.x
Rosenbloom BN, Khan S, McCartney C, Katz J (2013) Systematic review of persistent pain and psychological outcomes following traumatic musculoskeletal injury. J Pain Res 6:39–51. doi:10.2147/JPR.S38878
Efron B, Tibshirani RJ (1993) An introduction to bootstrap. Chapman and Hall, New York
Lauweryns P (2010) Role of conservative treatment of cervical spine injuries. Eur Spine J 19(Suppl 1):S23–S26. doi:10.1007/s00586-009-1116-4
Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V (2003) Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am 85-A:773–781
Siebenga J, Segers MJ, Leferink VJ, Elzinga MJ, Bakker FC, Duis HJ, Rommens PM, Patka P (2007) Cost-effectiveness of the treatment of traumatic thoracolumbar spine fractures: nonsurgical or surgical therapy? Indian J Orthop 41:332–336. doi:10.4103/0019-5413.36997
Søgaard RSJ (2014) Health care costs attributable to hospital-diagnosed back pain: a Longitudinal Register-based Study of the Danish Population. J Health Econ Outcomes Res 1:266–275
Castillo RC, MacKenzie EJ, Wegener ST, Bosse MJ, Group LS (2006) Prevalence of chronic pain seven years following limb threatening lower extremity trauma. Pain 124:321–329. doi:10.1016/j.pain.2006.04.020
Charlson ME, Charlson RE, Peterson JC, Marinopoulos SS, Briggs WM, Hollenberg JP (2008) The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 61:1234–1240. doi:10.1016/j.jclinepi.2008.01.006
Holder HD, Blose JO (1986) Alcoholism treatment and total health care utilization and costs. A four-year longitudinal analysis of federal employees. JAMA 256:1456–1460
Sørensen JSR (2013) Lifetime health care costs of the Danish population. J Health Econ Outcomes Res 1:163–173
Aras EL, Bunger C, Hansen ES et al (2016) Cost-effectiveness of surgical vs. conservative treatment for thoracolumbar burst fractures. Spine (Phila Pa 1976) 41(4):337–343
Rajasekaran S (2010) Thoracolumbar burst fractures without neurological deficit: the role of conservative treatment. Eur Spine J 19(Suppl 1):S40–S47
Bakhsheshian J, Dahdaleh NS, Fakurnejad S et al (2014) Evidence-based management of traumatic thoracolumbar burst fractures: a systematic review of nonoperative management. Neurosurg Focus (United States) 37(1):pE1
Wood KB, Li W, Lebl DS, Ploumis A (2014) Management of thoracolumbar spine fractures. Spine J 14(1):145–164
Abudou M, Chen X, Kong X et al (2013) Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev (England) 6:pCD005079
Acknowledgments
This study was funded by the Danish Strategic Research Council as part of the CESpine project (Grant 2142-08-0017). We gratefully acknowledge the assistance of Filipe Cortes Figueiredo, Lisbon Faculty of Medicine, University of Lisbon, Portugal and Stanislaus Argeny, Medical University of Vienna for data recruitment and organization during their research stay in Denmark. The authors express their appreciation to Linda Nygaard for help in editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Aras, E.L., Bunger, C., Hansen, E.S. et al. Health-care costs of conservative management of spine fractures in trauma patients. Eur Spine J 26, 1438–1446 (2017). https://doi.org/10.1007/s00586-016-4806-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4806-8