Abstract
Background/Purpose
The purpose of this study was to obtain the fundamental data necessary to discuss the appropriate operative mode for the resection of main-duct type intraductal papillary mucinous neoplasms (mIPMNs) of the pancreas.
Methods
In 23 patients who underwent total pancreatectomy with preoperative and postoperative diagnoses of mIPMN, the imaging studies and clinicopathological data were collected. The whole pancreatic specimen was histologically evaluated, and the distribution of atypical epithelium was mapped on a schema.
Results
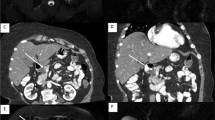
Pathological examination of the specimens revealed that 18 patients had carcinoma in the pancreas; 8 patients had invasive lesions and one patient had lymph node metastasis. Specimens from 5 patients did not bear carcinoma lesions but had widespread borderline lesions in the pancreas. The mapping of lesions in the pancreatic specimens revealed that, at least, borderline or higher lesions were present both in the head and distal pancreas in all patients. In the majority of the specimens, lesions from adenoma to carcinoma co-existed on the same slide, and there were normal cell intervals between the malignant lesions.
Conclusion
We conclude that total pancreatectomy should be performed for mIPMN when dilatation of the main duct suggests possible spread of the lesion to the whole pancreas.


Similar content being viewed by others
References
Ohhashi K, Murakami Y, Maruyama M, Takekoshi T, Ohta H, Ohhashi I, et al. Four cases of mucous secreting pancreatic cancer. Prog Dig Endosc. 1982;20:348–51.
Furukawa T, Takahashi T, Kobari M, Matsuno S. The mucus-hypersecreting tumor of the pancreas. Development and extension visualized by three-dimensional computerized mapping. Cancer. 1992;70:1505–13.
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Longnecker D, Adler G, Hruban R, Kloppel G. Intraductal papillary-mucinous neoplasm of the pancreas. Lyon: IARC press; 2000.
Japan Pancreas Society. General rules for the study of pancreatic cancer. Tokyo: Kanehara; 2002.
Kobari M, Egawa S, Shibuya K, Shimamura H, Sunamura M, Takeda K, et al. Intraductal papillary mucinous tumors of the pancreas comprise 2 clinical subtypes: differences in clinical characteristics and surgical management. Arch Surg. 1999;134:1131–6.
Terris B, Ponsot P, Paye F, Hammel P, Sauvanet A, Molas G, et al. Intraductal papillary mucinous tumors of the pancreas confined to secondary ducts show less aggressive pathologic features as compared with those involving the main pancreatic duct. Am J Surg Pathol. 2000;24:1372–7.
Doi R, Fujimoto K, Wada M, Imamura M. Surgical management of intraductal papillary mucinous tumor of the pancreas. Surgery. 2002;132:80–5.
Matsumoto T, Aramaki M, Yada K, Hirano S, Himeno Y, Shibata K, et al. Optimal management of the branch duct type intraductal papillary mucinous neoplasms of the pancreas. J Clin Gastroenterol. 2003;36:261–5.
Kitagawa Y, Unger T, Taylor S, Kozarek R, Traverso L. Mucus is a predictor of better prognosis and survival in patients with intraductal papillary mucinous tumor of the pancreas. J Gastrointest Surg. 2003;7:12–8.
Sugiyama M, Izumisato Y, Abe N, Masaki T, Mori T, Atomi Y. Predictive factors for malignancy in intraductal papillary-mucinous tumours of the pancreas. Br J Surg. 2003;90:1244–9.
Sohn T, Yeo C, Cameron J, Hruban R, Fukushima N, Campbell K, Lillemoe K. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–97.
Salvia R, Fernández-del Castillo C, Bassi C, Thayer S, Falconi M, Mantovani W, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–85.
Choi B, Kim T, Kim A, Kim K, Park S, Kim P, et al. Differential diagnosis of benign and malignant intraductal papillary mucinous tumors of the pancreas: MR cholangiopancreatography and MR angiography. Korean J Radiol. 2003;4:157–62.
Kim S, Park K, Lee Y, Lee S, Seo D, Lee S, et al. Intraductal papillary mucinous neoplasm of the pancreas: clinical characteristics and treatment outcomes of 118 consecutive patients from a single center. J Hepatobiliary Pancreat Surg. 2008;15:183–8.
Manfredi R, Graziani R, Motton M, Mantovani W, Baltieri S, Tognolini A, et al. Main pancreatic duct intraductal papillary mucinous neoplasms: accuracy of MR imaging in differentiation between benign and malignant tumors compared with histopathologic analysis. Radiology. 2009;253:106–15.
Chari S, Yadav D, Smyrk T, DiMagno E, Miller L, Raimondo M, et al. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology. 2002;123:1500–7.
Maire F, Hammel P, Terris B, Paye F, Scoazec J, Cellier C, et al. Prognosis of malignant intraductal papillary mucinous tumours of the pancreas after surgical resection. Comparison with pancreatic ductal adenocarcinoma. Gut. 2002;51:717–22.
Raimondo M, Tachibana I, Urrutia R, Burgart L, DiMagno E. Invasive cancer and survival of intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol. 2002;97:2553–8.
Wada K, Kozarek R, Traverso L. Outcomes following resection of invasive and noninvasive intraductal papillary mucinous neoplasms of the pancreas. Am J Surg. 2005;189:632–6.
Jang J, Kim S, Ahn Y, Yoon Y, Choi M, Lee K, et al. Multicenter analysis of clinicopathologic features of intraductal papillary mucinous tumor of the pancreas: is it possible to predict the malignancy before surgery? Ann Surg Oncol. 2005;12:124–32.
Raut C, Cleary K, Staerkel G, Abbruzzese J, Wolff R, Lee J, et al. Intraductal papillary mucinous neoplasms of the pancreas: effect of invasion and pancreatic margin status on recurrence and survival. Ann Surg Oncol. 2006;13:582–94.
Schnelldorfer T, Sarr M, Nagorney D, Zhang L, Smyrk T, Qin R, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg. 2008;143:639–46.
Nara S, Shimada K, Kosuge T, Kanai Y, Hiraoka N. Minimally invasive intraductal papillary-mucinous carcinoma of the pancreas: clinicopathologic study of 104 intraductal papillary-mucinous neoplasms. Am J Surg Pathol. 2008;32:243–55.
Stauffer J, Nguyen J, Heckman M, Grewal M, Dougherty M, Gill K, et al. Patient outcomes after total pancreatectomy: a single centre contemporary experience. HPB (Oxford). 2009;11:483–92.
Yang A, Melstrom L, Bentrem D, Ujiki M, Wayne J, Strouch M, et al. Outcomes after pancreatectomy for intraductal papillary mucinous neoplasms of the pancreas: an institutional experience. Surgery. 2007;142:529–34.
Acknowledgments
We thank the following individuals for their contributions to the discussion. Moderator: Tatsuya Aoki, Third Department of Surgery, Tokyo Medical University; commentators: Koji Yamaguchi, Department of Surgery, University of Occupational and Environmental Health; Koichi Aiura, Department of Surgery, Keio University School of Medicine; and Sohei Satoi, Department of Surgery, Kansai Medical University.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ito, T., Doi, R., Yoshizawa, A. et al. The distribution of atypical epithelium in main-duct type intraductal papillary mucinous neoplasms of the pancreas. J Hepatobiliary Pancreat Sci 18, 241–249 (2011). https://doi.org/10.1007/s00534-010-0337-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-010-0337-6