Abstract
Purpose
To assess the effectiveness of healthy lifestyle–based interventions in lung cancer survivors.
Methods
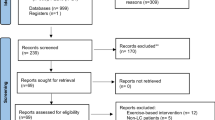
We performed a literature search using PubMed, Web of Science, and Science Direct (last search March 2022). Quality assessment and risk of bias were assessed using the Downs and Black scale and the Cochrane tool. A systematic review and meta-analysis of randomized controlled trials were performed. We included controlled trials testing the effect of healthy lifestyle–based interventions in lung cancer survivors versus a control intervention where lung cancer patients had no treatment, were receiving the usual care, or had not an active role in the intervention. The data were pooled and a meta-analysis was completed for quality of life, psychological distress, and cancer-related symptoms.
Results
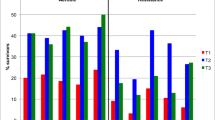
We selected 14 studies, which included 1519 patients with lung cancer. The treatment status of these patients was heterogeneous. Healthy lifestyle programs were applied isolated or in combination with usual care in most of the studies. The components of the healthy lifestyle programs were also heterogeneous. Results showed significant differences in favor of healthy lifestyle–based interventions in comparison to the control group for quality of life (p = 0.01), psychological distress (p = 0.05), and cancer-related symptoms (p = 0.03).
Conclusions
The findings indicated a beneficial effect of healthy lifestyle–based interventions for improving quality of life, psychological distress, and cancer-related symptoms in lung cancer patients. However, this review could not show any conclusion about the better treatment moment to apply healthy lifestyle–based interventions.
Review registration
PROSPERO Identifier: CRD42021292152.
Review registration date
19/12/2021.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 00:1e22
Anand P, Kunnumakkara AB, Kunnumakara AB et al (2008) Cancer is a preventable disease that requires major lifestyle changes. Pharm Res 25:2097–2116
Hemminki K, Lönnstedt I, Vaittinen P, Lichtenstein P (2001) Estimation of genetic and environmental components in colorectal and lung cancer and melanoma 20(1): 107–116. https://doi.org/10.1002/1098-2272(200101)20:1<107:aid-gepi9>3.0.co;2-4
Von Haehling S, Anker SD (2010) Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle 1:1–5
Peters R, Ee N, Peters J, Beckett N, Booth A, Rockwood K, Anstey KJ (2019) Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: the implied potential for targeted risk reduction. TherAdv Chronic Dis 10. https://doi.org/10.1177/2040622319880392
Parsons A, Daley A, Begh R, Aveyard P (2010) Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ 340:b5569
Lam TK, Gallicchio L, Lindsley K et al (2009) Cruciferous vegetable consumption and lung cancer risk: a systematic review. Cancer Epidemiol Biomarkers Prev 18(1):184–195
Blok AC, Blonquist TM, Nayak MM et al (2018) Feasibility and acceptability of “healthy directions” a lifestyle intervention for adults with lung cancer. Psychooncology 27(1):250–257
Holland JC, Andersen B, Breitbart WS et al (2013) Distress management: clinical practice guidelines in oncology. J Natl Compr Canc Netw 11:190–209
Porter LS, Keefe FJ, Garst J, McBride CM, Baucom D (2008) Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: associations with symptoms and distress. Pain 137(2):306–315
Somayaji D, Blok AC, Hayman LL, Colson Y, Jaklisch M, Cooley ME (2019) Enhancing behavioral change among lung cancer survivors participating in a lifestyle risk reduction intervention: a qualitative study. Support Care Cancer 27(4):1299–1308. https://doi.org/10.1007/s00520-018-4631-1
Mosher CE, Sloane R, Morey MC et al (2009) Associations between lifestyle factors and quality of life among older long-term breast, prostate, and colorectal cancer survivors. Cancer 115(17):4001–4009
Irwin ML, Cartmel B, Harrigan M et al (2017) Effect of the livestrong at the YMCA exercise program on physical activity, fitness, quality of life, and fatigue in cancer survivors. Cancer 123(7):1249–1258
Aggarwal A, Lewison G, Idir S et al (2016) The state of lung cancer research: a global analysis. J Thorac Oncol 11(7):1040–1050
Linden W, Vodermaier A, Mackenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 141:343e351
Glanz K, Bishop DB (2010) The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 31(1):399–418. https://doi.org/10.1146/annurev.publhealth.012809.103604
Bandura A (2004) Health promotion by social cognitive means. Health Educ Behav 31(2):143–164. https://doi.org/10.1177/1090198104263660
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189. https://doi.org/10.1016/j.jclinepi.2021.03.001
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Hoboken
Akers J, Aguiar-Ibáñez R, Baba-Akbari A (2009) Systematic reviews: CRD’s guidance for undertaking reviews in health care. Centre for Reviews and Dissemination, University of York, York
World Health Organization (2011) Burden of disease from environmental noise: Quantification of healthy life years lost in Europe. World Health Organization. Regional Office for Europe, Copenhagen
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384. https://doi.org/10.1136/jech.52.6.377
Deeks JJ, Dinnes J, D’Amico R et al (2003) International Stroke Trial Collaborative Group, European Carotid Surgery Trial Collaborative Group. Evaluating non-randomised intervention studies. Health Technol Assess 7(27):1–173. https://doi.org/10.3310/hta7270
Saunders LD, Soomro GM, Buckingham J et al (2003) Assessing the methodological quality of nonrandomized intervention studies. West J Nurs Res 25(2):223–237. https://doi.org/10.1177/0193945902250039
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. Brit Med J 343:5928. https://doi.org/10.1136/bmj.d5928
Holroyd-Leduc JM (2002) Critical Evaluation of Research in Physical Rehabilitation: Towards Evidence-Based Practice. In: Helewa A, Walker JM. WB Saunders Company, 2000, Philadelphia. BMJ Evidence-Based Medicine 7(5):135–135
Sun Y, Wang X, Li N et al (2021) Influence of psychological nursing and health education on depression, anxiety and life quality of elderly patients with lung cancer. Psychogeriatrics 21(4):521–527
Güneş IH, Karadağ G, Kul S (2020) Effect of breathing relaxation exercise training on the self-care agency and functional life of the lung cancer patients: a randomized controlled trial. World Cancer Research Journal 7:e1619. https://doi.org/10.32113/wcrj_20207_1619
Zhu X, Han S, Chu H et al (2020) Influence of self-management exercise intervention on the cancer related fatigue severity and self-management efficacy of patients with non-small cell lung cancer after operation. JPMA 70:88–93
Edbrooke L, Aranda S, Granger CL (2019) Multidisciplinary home-based rehabilitation in inoperable lung cancer: a randomised controlled trial. Thorax 74(8):787–796
Huang CC, Kuo HP, Lin YE et al (2019) Effects of a web-based health education program on quality of life and symptom distress of initially diagnosed advanced non-small cell lung cancer patients: a randomized controlled trial. J Cancer Educ 34(1):41–49
Geerse OP, Hoekstra-Weebers JEHM, Stokroos MH et al (2017) Structural distress screening and supportive care for patients with lung cancer on systemic therapy: a randomised controlled trial. Eur J Cancer 72:37–45
Yorke J, Lloyd-Williams M, Smith J et al (2015) Management of the respiratory distress symptom cluster in lung cancer: a randomised controlled feasibility trial. Support Care Cancer 23(11):3373–3384
Yount SE, Rothrock N, Bass M et al (2014) A randomized trial of weekly symptom telemonitoring in advanced lung cancer. J Pain Symptom Manage 47(6):973–989
Rodríguez CF, Fernández EV, García PF, Fernández SG (2014) Efectos de la activación conductual en la calidad de vida y estado emocional de los pacientes con cáncer de pulmón. Psicooncología: investigación y clínica biopsicosocial en oncología 11(2):199–215
Schofield P, Ugalde A, Gough K et al (2013) A tailored, supportive care intervention using systematic assessment designed for people with inoperable lung cancer: a randomised controlled trial. Psychooncology 22(11):2445–2453
Chan CW, Richardson A, Richardson J (2011) Managing symptoms in patients with advanced lung cancer during radiotherapy: results of a psychoeducational randomized controlled trial. J Pain Symptom Manage 41(2):347–357
Temel JS, Greer JA, Admane S et al (2011) Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non–small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 29(17):2319–2326
Wilkie D, Berry D, Cain K et al (2010) Effects of coaching patients with lung cancer to report cancer pain. West J Nurs Res 32(1):23–46
Goldberg RJ, Wool MS (1985) Psychotherapy for the spouses of lung cancer patients: assessment of an intervention. Psychother Psychosom 43(3):141–150
Green AC, Hayman LL, Cooley ME (2015) Multiple health behavior change in adults with or at risk for cancer: a systematic review. Am J Health Behav 39(3):380–394. https://doi.org/10.5993/AJHB.39.3.11
Sebio-Garcia R, Yáñez-Brage MI, Giménez-Moolhuyzen E, Granger CL, Denehy L (2016) Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 23(3):486–497. https://doi.org/10.1093/icvts/ivw152
Granger CL, Connolly B, Denehy L, Hart N, Antippa P, Lin KY, Parry SM (2017) Understanding factors influencing physical activity and exercise in lung cancer: a systematic review. Support Care Cancer 25(3):983–999. https://doi.org/10.1007/s00520-016-3484-8
McBride CM, Emmons KM, Lipkus IM (2003) Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res 18(2):156–170
Adams RN, Mosher CE, Blair CK, Snyder DC, Sloane R, Demark-Wahnefried W (2015) Cancer survivors’ uptake and adherence in diet and exercise intervention trials: an integrative data analysis. Cancer 121(1):77–83
Rock CL, Doyle C, Demark-Wahnefried W et al (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):243–274
Sezgin E, Militello LK, Huang Y, Lin S (2020) A scoping review of patient-facing, behavioral health interventions with voice assistant technology targeting self-management and healthy lifestyle behaviors. Transl Behav Med 10(3):606–628. https://doi.org/10.1093/tbm/ibz141
Manger S (2019) Lifestyle interventions for mental health. Aust J Gen Pract 48(10):670–673. https://doi.org/10.31128/AJGP-06-19-4964
Spei ME, Samoli E, Bravi F, La Vecchia C, Bamia C, Benetou V (2019) Physical activity in breast cancer survivors: a systematic review and meta-analysis on overall and breast cancer survival. Breast 44:144–152. https://doi.org/10.1016/j.breast.2019.02.001
Riekert K, Ockene JK, Pbert L (2013) The Handbook of Health Behavior Change, 4th edn. Springer Publishing Company, New York NY, p 507
Ashford S, Edmunds J, French DP (2010) What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol 15(2):265–288. https://doi.org/10.1348/135910709X461752
Wu X, Guo X, Zhang Z (2019) The efficacy of mobile phone apps for lifestyle modification in diabetes: systematic review and meta-analysis. JMIR Mhealth Uhealth 157(1):e12297. https://doi.org/10.2196/12297
Seiler A, Klaas V, Tröster G, Fagundes CP (2017) eHealth and mHealth interventions in the treatment of fatigued cancer survivors: a systematic review and meta-analysis. Psychooncology 26(9):1239–1253
Funding
Heredia-Ciuró Alejandro has received financial support through a FPU (“Formación Profesorado Universitario”) grant (FPU:20/01670) of the Spanish Ministry of Education. The author Calvache-Mateo Andrés has received financial support through a FPU (“Formación Profesorado Universitario”) grant (FPU:19/02609) of the Spanish Ministry of Education.
Author information
Authors and Affiliations
Contributions
The author Valenza Marie Carmen had the idea for the article and full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Heredia-Ciuró Alejandro and Martín-Núñez Javier had full access to all the data in the study and takes responsibility for performing the literature search and data analysis. López-López José Antonio, López-López Laura, Granados-Santiago María, and Calvache-Mateo Andrés contributed substantially to draft and critically revise the work, and the writing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Search strategy
Appendix. Search strategy
Pubmed
(neoplas*[Title/Abstract]) OR (metastat*[Title/Abstract])) OR (cancer*[Title/Abstract])) OR (carcino[Title/Abstract])) OR (carcinoma*[Title/Abstract])) OR (onco*[Title/Abstract])) OR (tumor*[Title/Abstract])) OR (tumour*[Title/Abstract])) OR (malignan*[Title/Abstract])) AND (Lung[Title/Abstract])) OR (Lungs[Title/Abstract])) AND (self care[Title/Abstract])) OR (self-care[Title/Abstract])) OR (self manage[Title/Abstract])) OR (self-manage[Title/Abstract])) OR (self efficacy[Title/Abstract])) OR (self-efficacy[Title/Abstract])) OR (home base[Title/Abstract])) OR (home-base[Title/Abstract])) OR (health education[Title/Abstract])) OR (patient education[Title/Abstract])) OR (patient participation[Title/Abstract])) OR (health communication[Title/Abstract])) OR (health promotion[Title/Abstract])) OR (self concept[Title/Abstract])) OR (self-control[Title/Abstract])) OR (self concept[MeSH Terms])) OR (self-regulation[Title/Abstract])) OR (patient autonomy[Title/Abstract])) OR (patient compliance[MeSH Terms])) OR (health behavior[MeSH Terms])) OR (health attitude[Title/Abstract])) OR (illness attitude[Title/Abstract])) OR (patient attitude[Title/Abstract])) OR (choice behavior[MeSH Terms])) OR (illness behavior[MeSH Terms])) OR (Self-management[Title/Abstract])) OR (adaptation, psychological[MeSH Terms])) OR (adjustment disorders[MeSH Terms])) OR (disease management[MeSH Terms])) OR (Adjustment[Title/Abstract]).
Web of Science
(neoplas* OR metastat* OR cancer* OR carcino* OR carcinoma* OR onco* OR tumor* OR tumour* OR malignan*) AND (“Lung” OR “Lungs”) AND (“self care” OR “self-care” OR “self manage” OR “self-manage” OR “self efficacy” OR “self-efficacy” OR “home base” OR “home-base” OR “health education” OR “patient education” OR “patient participation” OR “health communication” OR “health promotion” OR “self concept” OR “Self-control” OR “Self-regulation” OR Patient autonomy* OR “health behavior” OR “Health attitude” OR “Illness attitude” OR Patient attitude* OR “Self management” OR Adjustment*) AND (RCT OR Randomized Controlled Trial).
Science Direct
(*neoplas OR *metastat OR *cancer OR *carcino OR *carcinoma OR *onco OR *tumor OR *tumour OR *malignan) AND (“Lung” OR “Lungs”) AND (“self care” OR “self-care” OR “self manage” OR “self-manage” OR “self efficacy” OR “self-efficacy” OR “home base” OR “home-base” OR “health education” OR “patient education” OR “patient participation” OR “health communication” OR “health promotion” OR “self concept” OR “Self-control” OR “Self-regulation” OR *Patient autonomy OR “health behavior” OR “Health attitude” OR “Illness attitude” OR *Patient attitude OR “Self management” OR *Adjustment) AND (RCT OR Randomized Controlled Trial).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heredia-Ciuró, A., Martín-Núñez, J., López-López, J.A. et al. Effectiveness of healthy lifestyle–based interventions in lung cancer survivors: a systematic review and meta-analysis. Support Care Cancer 31, 71 (2023). https://doi.org/10.1007/s00520-022-07542-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07542-0