Abstract
Purpose
It is unknown whether positive psychological changes (e.g., in life perspective, self-perception, and social relationships) after being diagnosed with ovarian cancer can reduce anxiety and depression in patients and their partners. The first aim of the present study was to assess differences in anxiety and depression between patients diagnosed with an ovarian tumor and their partners. The second aim was to explore the mutual associations of patients’ and partners’ posttraumatic growth and their anxiety and depressive symptoms.
Methods
Participants included 130 Dutch couples of which one partner was diagnosed with a borderline ovarian tumor or ovarian cancer between 2000 and 2010, as registered by the Netherlands Cancer Registry. In September 2011, a questionnaire was sent including the Hospital Anxiety and Depression Scale (anxiety and depression) and Cancer Survivors (Partners) Unmet Needs measure (positive psychological changes).
Results
A one-way multivariate analysis of variance showed that patients reported higher anxiety than partners, without differences in depression. Contrasting to our expectations, an actor-partner interdependence model revealed no mutual dyadic associations between positive psychological changes and anxiety or depressive symptoms.
Conclusions
Based on these findings, positive psychological change seems to be an independent construct unrelated to anxiety or depression in couples diagnosed with ovarian tumors. Still, as ovarian tumor patients and partners suffer from high anxiety and depression, further research investigating how these feelings can be reduced in couples dealing with an ovarian tumor is necessary.
Similar content being viewed by others
Background
Ovarian tumors can be distinguished in borderline ovarian tumors and ovarian cancer. Borderline tumors of the ovary (also called tumors of low-malignant potential) are a heterogeneous group of lesions defined histologically by atypical epithelial proliferation without stromal invasion. Borderline ovarian tumors are mostly diagnosed at an earlier stage, resulting in an excellent prognosis with a 5-year survival of 98%, while in contrast, ovarian cancer has an overall 5-year survival of 38–46% [1,2,3]. Due to the poor prognosis of ovarian cancer, patients and their loved ones are prone to psychological problems such as anxiety and depression after diagnosis [4,5,6]. For borderline ovarian tumors, evidence on the psychological burden is lacking, although it is known patients correlate the malignant potential of their tumor close to that of ovarian cancer even though they are aware their prognosis is more favorable [7].
Caregivers of cancer patients are just as likely as patients to suffer from psychological distress, including negative affect [8]. It is unclear if there are any differences between ovarian tumor patients and partners in experienced anxiety or depression. Several studies in gynecological and breast cancer patients and partners reported that partners of female cancer patients experience higher levels of negative affect, including depression, anxiety, phobic anxiety, and overall distress than patients themselves [8,9,10]. In contrast, a meta-analysis showed female patients report more psychological stress than their partners [11]. This meta-analysis included few studies involving gynecological cancers (9%) and few studies covering patients with advanced stage cancers (8%), which results in too little clarity to draw conclusions on differences in experienced anxiety and depression between ovarian tumor patients and partners.
Although being diagnosed with cancer often leads to anxiety and depression, patients can also experience positive psychological changes following a cancer diagnosis [12]. Positive psychological changes are often measured as posttraumatic growth (PTG), which is defined as “positive psychological change experienced as a result of the struggle with highly challenging life circumstances” [13]. It includes benefits such as positive changes in self-perception (e.g., viewing oneself as mentally stronger and as more capable to cope with problems in the future), social relationships (e.g., feeling more connected to others, knowing who one’s real friends are), and life perspective (e.g., being more appreciative of the small things in life, finding greater meaning in intrinsically important priorities) [14]. Between 53 and 90% of cancer patients report to experience some level of PTG [12, 15, 16]. Moreover, cancer patients who experience PTG generally tend to report higher levels of positive affect and lower levels of negative affect than patients who do not experience PTG [17, 18]. Similarly, partners of ovarian tumor patients might experience positive psychological changes as well. Two studies, of which one involving couples suffering from various forms of cancer and one including gynecological cancer couples exclusively, found couples experience similar levels of PTG, indicating patients share their psychological growth with their partners [19, 20].
So far, there are no published data on the association of positive psychological changes and anxiety and depression of ovarian tumor couples. The current study aims to assess (1) differences between patients and partners with ovarian cancer and borderline ovarian tumors in severity of anxiety and depression, (2) differences in anxiety and depression of patients with ovarian cancer and borderline ovarian tumors, and (3) the association between positive psychological changes and anxiety and depression on patients and partners, and their mutual influence. This involves analyzing the direct effects of one’s positive psychological changes on their anxiety and depression and the mutual effects of one’s positive psychological changes on their partner’s anxiety and depression. Since the literature shows conflicting conclusions about anxiety, depression, and positive psychological changes among couples suffering from ovarian tumors, no hypotheses are formed.
Methods
Design, setting, and participants
In this population-based cross-sectional study, participants were diagnosed with ovarian cancer or a borderline ovarian tumor between 1 January 2000 and 1 July 2010 as registered in the Netherlands Cancer Registry (NCR). Ethical approval for the study was obtained from the Medical Ethics Committee of the Elisabeth-TweeSteden Hospital.
Data collection
In September 2011, 719 women diagnosed with an ovarian tumor were invited to participate via their gynecologists (Fig. 1). Participants received a letter and paper questionnaires from their (ex-)attending specialist. Two questionnaires had been sent to them: one version for the ovarian tumor patient and one version for their partner. By returning the questionnaire, they provided informed consent. The data collection was done within PROFILES (Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship), a registry for studies on the physical and psychosocial impact of cancer and its treatment from a dynamic, growing population-based cohort of cancer survivors [21]. PROFILES is linked directly to the NCR. In 2012, 130 couples completed both the patient and partner questionnaires (90 ovarian, 40 borderline ovarian) (Fig. 1).
Clinical and sociodemographic characteristics
Clinical information (i.e., date of birth, date of diagnosis, stage, grade) and information about socioeconomic status were obtained from the NCR [22]. Further sociodemographic information (i.e., gender of partner, marital status, education) was collected from the questionnaires. Comorbidity at the time of survey was assessed with the adapted Self-administered Comorbidity Questionnaire [23].
Instruments
The Dutch translation of the Hospital Anxiety and Depression Scale (HADS) was used to determine the amount of anxiety and depressive symptoms [24]. Participants responded to seven anxiety items and seven depression items referring to current feelings on a 4-point scale. The HADS is deemed a highly reliable screening instrument for Dutch somatically ill patients to determine distress (Cronbach’s alpha = .90) [25]. However, among caregivers of cancer patients, the total HADS (the combination of the anxiety and depression subscales) is not supported to measure distress [26], and the unidimensional anxiety and depression scales are considered more valid as separate scales, with Cronbach’s alpha values of .90 and .86, respectively [26]. Since the following study included both cancer patients and partners, anxiety and depression were included in analyses as separate constructs.
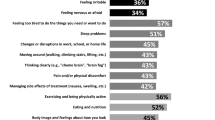
Additionally, the six positive outcome items of CaS(P)UN (Cancer Survivors (Partners) Unmet Needs measure) were included to measure positive psychological changes, also indicated as benefit-finding and posttraumatic growth [27]. CaSUN items were included in the patient questionnaire. CaSPUN items were included in the partner questionnaire. CaS(P)UN items offer four response options (“yes, but I have always been like this,” “yes, this has been a positive outcome,” “no, and I would like help to achieve this,” or “no, and this is not important to me”). Sensitivity analyses on each individual CaS(P)UN item for anxiety and depression showed similar effects across all CaS(P)UN items as none of the items predicted anxiety or depression for patients or partners. Therefore, for each patient, the total number of times the option “yes, this has been a positive outcome” on each of the six questions was computed and taken as indication of the level of experienced positive psychological changes. Thus, PTG was transformed into a sum variable with a range from 0 to 6. The content of the items within the questionnaires for patient and partner were identical. Although no research has been done on the validation of the six positive outcome items of CaS(P)UN for measuring PTG, the items were still used since no other specific measurement of PTG experienced by partners was found and Hodgkinson et al. [27] implied PTG and positive psychological changes are similar concepts.
Statistical analyses
Statistical analyses were performed using SPSS Statistics 22.0. Two-sided p values lower than .05 were considered significant unless specified otherwise. To determine the required number of participating couples, a post hoc power analysis was performed using G*Power 3.1.9.2. The necessary n is measured by using “linear multiple regression: fixed model, R2 deviation from zero” as the statistical test used concerning the second research question. The following settings were used: medium effect size = .15, α error probability = .05, power (1 − β error probability) = .95, and number of predictors = 2. Results showed 107 couples are required to reach the preferred power level. The current study used more than 107 couples (n = 130) accounting for missing values.
First, descriptive statistics were calculated for the sociodemographic, medical, and psychological data of ovarian tumor patients and partners and were described by means, standard deviations, and percentages. Anxiety and depression tend to be comorbid [28], thus predicting a high interdependency level between anxiety and depression. Therefore, a one-way multivariate analysis of variance (MANOVA) was performed to answer the first research question, since this procedure (1) examines mean differences between the dependent variables while accounting for their interdependency, (2) shows the relationship between anxiety and depression rather than examining each of them in isolation, and (3) prevents the risk of an inflated type 1 error, which could be caused if two separate univariate analyses of variance (ANOVAs) were performed on anxiety and depression [29, 30]. By performing a MANOVA with two dependent variables, it is necessary to apply a Bonferroni adjusted alpha level of .025 [31]. Analyses were adjusted for age as a possible confounder.
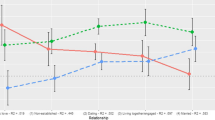
The second research question involved whether symptoms of anxiety and depression in patients and partners are associated with positive psychological changes. A multilevel model in the form of a two-intercept model, the actor-partner interdependence model (APIM), was used. The multilevel model takes into account the correlation of patient and partner data [32]. Additionally, by applying the APIM, it is possible to calculate the effect of one’s independent variable on their own dependent variable (i.e., actor effect), as well as the effect of one’s independent variable on the dependent variable of their partner (i.e., partner effect) [33]. All continuous variables were centered on the sample mean. All dichotomous variables were coded as 1 and − 1. The APIM was performed with a heterogeneous compound symmetry (HCS) as we assumed patients and partners are distinguishable members within their dyad with equal influence on each other [32].
The two-intercept model involves dropping the ordinary intercept from the model in order to include two dummy variables as intercepts [32]. The following two dummy variables were created: patient (patient = 1, partner = 0) and partner (patient = 0, partner = 1). The dummy variables corresponded to the individual intercepts for each of the patient and partner variables. The separate predictor variables for patients and partners were created by multiplying the dummy variables with the positive psychological changes experienced by patient (PatientPTG) and the positive psychological changes experienced by partner (PartnerPTG). This resulted in the following regression equations: [Anxiety = Patient + Partner + PatientPTG + PartnerPTG] and [Depression = Patient + Partner + PatientPTG + PartnerPTG]. Consequently, a single model showed the effect of both patient and partner PTG on patient- and partner-dependent variables (either anxiety or depression). In total, two models were created: one with anxiety and one with depression as the dependent variable. We combined ovarian cancer and borderline ovarian tumors for these analyses as we did not expect the association between positive psychological changes and anxiety and depression to be different between these tumor types and because we had a sufficient sample size for the analyses.
Results
Patients and partners
Ovarian cancer patients were on average 61 years of age, and their partners were on average 63. Borderline ovarian tumor patients were on average 57 years of age, and their partners were on average 60 (Table 1). On average, patients were diagnosed with an ovarian tumor 6 years prior to questionnaire completion.
Anxiety and depression
Patients and partners reported different levels of their combined anxiety and depression score (Table 2). Further inspection showed a statistical difference for anxiety (Wilks’ lambda = .04; p = .01). Patients reported higher levels of anxiety (M = 5.6, SD = 3.7) than partners (M = 4.4, SD = 3.6). This difference is mainly attributable to ovarian cancer patients (M = 6.0; SD = 3.8) and their partners (M = 4.6, SD = 3.6). No differences were found on depression between patients (M = 4.0, SD = 4.2) and partners (M = 3.9, SD = 3.5).
For borderline ovarian tumors, there were no differences on anxiety or depression between patients (resp. M = 4.8, SD = 3.4; M = 3.5, SD = 3.9) and partners (M = 4.1, SD = 3.5; M = 2.7, SD = 2.8).
Comparing couples based on diagnosis, results showed partners of patients with ovarian cancer reported higher levels of depression (M = 4.4, SD = 3.6) than partners of patients with a borderline ovarian tumor (M = 2.7, SD = 2.8).
Positive psychological changes
There were no significant actor or partner effects found between patients’ or partners’ positive psychological changes and patients’ and partners’ anxiety or depression (Fig. 2).
Besides using the sum score for positive psychological changes, sensitivity analyses including each individual CaS(P)UN item were conducted, showing similar results as none of the items predicted anxiety or depression for patients or partners.
Discussion
Women with an ovarian tumor experience higher anxiety than their partners, though no significant difference in depressive symptoms was found. However, the results showed that both patients with ovarian cancer and their partners experienced higher levels of anxiety and depression, although this was only significant for depression in partners. In contrast to our expectations, positive psychological changes experienced by either the patient or partner were not associated with their own or their partner’s anxiety or depression levels.
Contrasting to our results, most other studies examining anxiety and depression among couples with gynecological tumors either found no difference between patients and partners on anxiety or depression [34] or found partners suffered more from distress than patients [8, 9]. These contrasts in findings may be explained by differences between our study and earlier studies. First, our study used a population-based sample, unlike two studies which used a clinical sample [9, 34].
Second, previous studies differ from the current study by their patient characteristics. One study included multiple cancer diagnoses besides gynecological cancer types [34], and consequently, it was unclear whether variations in anxiety and depression were attributed to patients with ovarian tumors. Another study exclusively included recovered patients who survived for more than 5 years since diagnosis [9]. Couples where the patient has been recovered from cancer have a different foundation for their anxiety and depression (e.g., dealing with the psychological aftermath of surviving cancer) from couples in whom the patient is uncertain about surviving cancer. The current study used a population-based sample unlike previous studies which used clinical samples.
Furthermore, all studies that reported that partners suffered from higher or equal levels of negative effect involved non-European participants [8, 9, 34]. There might be cultural differences between Dutch and non-European couples dealing with ovarian tumors, explaining the dyadic variation in anxiety and depression.
Finally, previous studies performed different analyses, which did not take into account the possible combined effects of anxiety and depression. As a result, the current study did not include the overlap between anxiety and depression but measured anxiety and depression as separate constructs. We showed anxiety is the factor that impacts distress.
In line with previous research, we found that ovarian cancer patients and borderline ovarian tumor patients reported no differences in anxiety or depression levels [7]. However, we did observe a trend in higher anxiety and depression levels among ovarian cancer patients compared to borderline ovarian tumor patients. These results indicate that even though the biological prognosis for ovarian cancer is less favorable than that for a borderline ovarian tumor, the psychological stress levels of both types of patients are not so different.
Consistent with our findings, several other studies found no associations between positive psychological changes and negative emotions like anxiety and depression [35,36,37]. A possible explanation is that experiencing positive psychological changes and experiencing negative feelings like anxiety and depression actually are entirely different constructs which co-exist without influencing each other. After all, someone with a potentially fatal disease like ovarian cancer can feel more positive and conscious about one’s self-perception, social relations, and life perspective due to the disease, while still feeling anxious and depressed about the possible consequences of the disease [38]. Another possibility may be that levels of positive psychological changes, anxiety, and depression fluctuate over time among survivors. Longitudinal studies are needed to assess changes over time in positive psychological changes, anxiety, and depression.
Limitations
There are several limitations that should be considered when interpreting the results of the present study. The sum of the six positive outcome items of the CaS(P)UN was used to measure the positive psychological changes, even though according to Hodgkinson et al. [27], the positive change items should be considered separately. To support our approach, we performed sensitivity analyses on all individual items, showing similar findings for anxiety and depression as with the sum score. In retrospect, another questionnaire like the Posttraumatic Growth Inventory (PTGI) could have been used [39] as PTG and positive psychological changes are similar constructs. However, the PTGI and other similar measurements were not validated among partners of patients diagnosed with cancer. As we included partners in our study, we used the CaS(P)UN questionnaires.
Another limitation of the study is the inclusion of both women diagnosed with ovarian cancer and women diagnosed with a borderline ovarian tumor for the second research question. Patients with a borderline ovarian tumor were included to achieve the required amount of participants for proper analyses. The prognosis of borderline ovarian tumor is better than the prognosis of ovarian cancer due to early diagnoses resulting in survival rates of 95% 5 years after diagnosis [40]. Therefore, the experienced anxiety, depression, and positive psychological changes may be different for patients with borderline ovarian tumors than for ovarian cancer patients. However, our study analyses showed no differences between patients with ovarian cancer and patients with borderline ovarian tumors.
Although for the first research question multicollinearity between anxiety and depression was taken into account by performing a MANOVA, for the second research question, two separate APIM analyses were conducted for anxiety and depression to analyze the effect of positive psychological changes. Therefore, anxiety was a potential confounding variable in the model examining the effect of positive psychological changes on depression. Similarly, in the model examining the effect of positive psychological changes on anxiety, depression was a potential confounding variable. We did not add depression and anxiety as covariates as this might have led to over-adjustment.
The response percentage of patients ranged between 43 and 57%, while for partners, this ranged from 70 to 30% for ovarian cancer and borderline ovarian tumor, respectively. These numbers limit the generalizability of our results as, for instance, non-respondents may experience lower quality of life or worse health compared to respondents.
A final limitation is that respondents were couples who voluntarily responded to a self-report questionnaire in an uncontrolled setting. Couples could have influenced each other or could have been influenced by other situational factors leading to biased responses. Also, only voluntary respondents were included, whereas there is a possibility anxiety and depression are more or less prevalent among non-respondents. This may have led to an underrepresentation of anxiety and depression in couples dealing with ovarian tumors.
Strengths
In spite of several limitations, the current study displayed several strengths such as the population-based sampling supporting generalizability.
Additionally, the current study seemingly is the first study which incorporated patients with ovarian tumors, their partners, anxiety, depression, and positive psychological changes. Subsequently, strong analyses were used to analyze (dyadic) associations between these concepts, including the MANOVA and APIM procedure.
Furthermore, robust analyses were performed to test the research questions. The data requested accurate analyses due to the highly interdependent nature of patient and partner variables. The APIM which was chosen as a measure for the analyses considers dyadic interdependence while analyzing the influence of individuals on themselves and on one another [41]. Similarly, the MANOVA was a strong measure which took into account the comorbidity between depression and anxiety.
Implications
It is noteworthy our study found the level of anxiety and depression for patients and partners surpassed the advised clinical cutoff scores for cancer patients (HADS-Depression ≥ 2; HADS-Anxiety ≥ 3) [42]. This confirms once more that even though patients experience more anxiety than partners, distress is a relevant issue for both patients and partners dealing with ovarian tumors. It is necessary to inform couples about the possible psychological consequences of the diagnosis. As results showed there were no actor or partner effects of positive psychological changes on anxiety or depression, couples with ovarian tumors should be educated that they might experience anxiety or depression besides positive psychological changes after diagnosis. Moreover, couples should have access to psycho-education about the differences and similarities in anxiety and depression experienced by patients and partners to better understand each other. Further research could explore which dyadic mechanisms could influence anxiety and depression in ovarian tumor patients and partners and which dyadic interventions might be appropriate to support both patients and partners.
Conclusion
The present study showed that patients diagnosed with ovarian tumors suffer more from anxiety than their partners, though no difference on depression was found. There may be a trend that ovarian cancer patients and their partners experience higher levels of anxiety and depression than patients with a borderline ovarian tumor and their partners, although differences are small and only significant for depression experienced by partners. Positive psychological changes experienced by patients and partners were not associated with anxiety or depression of patient or partner, indicating positive psychological changes have no effect on distress. As patients and partners had elevated levels of anxiety and depression, couples dealing with ovarian tumors should have access to supportive care to deal with their distress levels. Future research should assess whether dyadic interventions are appropriate.
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA: A Cancer J Clinicians 66(1):7–30. https://doi.org/10.3322/caac.21332
Cijfers over kanker [Numbers about cancer]. (2015) Integraal Kankercentrum Nederland. http://www.cijfersoverkanker.nl/nkr/index 2011
Cadron I, Leunen K, Van Gorp T, Amant F, Neven P, Vergote I (2007) Management of borderline ovarian neoplasms. J Clin Oncol Off J Am Soc Clin Oncol 25(20):2928–2937. https://doi.org/10.1200/JCO.2007.10.8076
Arden-Close E, Gidron Y, Moss-Morris R (2008) Psychological distress and its correlates in ovarian cancer: a systematic review. Psychooncology 17(11):1061–1072. https://doi.org/10.1002/pon.1363
Harrison J, Haddad P, Maguire P (1995) The impact of cancer on key relatives: a comparison of relative and patient concerns. Eur J Cancer 31A(11):1736–1740
Bodurka-Bevers D, Basen-Engquist K, Carmack CL, Fitzgerald MA, Wolf JK, de Moor C, Gershenson DM (2000) Depression, anxiety, and quality of life in patients with epithelial ovarian cancer. Gynecol Oncol 78(3 Pt 1):302–308. https://doi.org/10.1006/gyno.2000.5908
Fotopoulou C, Bugariu M, Braicu EI, Lichtenegger W, Sehouli J (2010) What are the individual perceptions of patients with borderline tumours of the ovary in regard to pathogenesis and prognosis? A structured survey on 60 women. J Psychosom Obstet Gynaecol 31(4):265–272. https://doi.org/10.3109/0167482X.2010.528091
Price MA, Butow PN, Costa DS, King MT, Aldridge LJ, Fardell JE, DeFazio A, Webb PM, Australian Ovarian Cancer Study G, Australian Ovarian Cancer Study Group Quality of Life Study I (2010) Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Med J Aust 193 (5 Suppl):S52–S57
Gilbar O, Steiner M, Atad J (1995) Adjustment of married couples and unmarried women to gynaecological cancer. Psycho-Oncology 4(3):203–211. https://doi.org/10.1002/pon.2960040306
Hasson-Ohayon I, Goldzweig G, Braun M, Galinsky D (2010) Women with advanced breast cancer and their spouses: diversity of support and psychological distress. Psychooncology 19(11):1195–1204. https://doi.org/10.1002/pon.1678
Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC (2008) Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull 134(1):1–30. https://doi.org/10.1037/0033-2909.134.1.1
Collins RL, Taylor SE, Skokan LA (1990) A better world or a shattered vision? Changes in life perspectives following victimization. Soc Cogn 8(3):263–285. https://doi.org/10.1521/soco.1990.8.3.263
Tedeschi RG, Calhoun LG (2004) Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 15(1):1–18. https://doi.org/10.1207/s15327965pli1501_01
Calhoun LG, Tedeschi RG (2014) Handbook of posttraumatic growth: research and practice. Routledge, New York
Taylor SE, Lichtman RR, Wood JV (1984) Attributions, beliefs about control, and adjustment to breast cancer. J Pers Soc Psychol 46(3):489–502
Sears SR, Stanton AL, Danoff-Burg S (2003) The yellow brick road and the emerald city: benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol 22(5):487–497. https://doi.org/10.1037/0278-6133.22.5.487
Barskova T, Oesterreich R (2009) Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil Rehabil 31(21):1709–1733. https://doi.org/10.1080/09638280902738441
Updegraff JA, Taylor SE (2000) From vulnerability to growth: positive and negative effects of stressful life events. In: Harvey J, Miller E (eds) Loss and trauma: general and close relationship perspectives. Brunner-Routledge, Philadelphia, pp 3–28
Zwahlen D, Hagenbuch N, Carley MI, Jenewein J, Buchi S (2010) Posttraumatic growth in cancer patients and partners—effects of role, gender and the dyad on couples’ posttraumatic growth experience. Psychooncology 19(1):12–20. https://doi.org/10.1002/pon.1486
Stafford L, Judd F (2010) Partners of long-term gynaecologic cancer survivors: psychiatric morbidity, psychosexual outcomes and supportive care needs. Gynecol Oncol 118(3):268–273. https://doi.org/10.1016/j.ygyno.2010.05.019
van de Poll-Franse LV, Horevoorts N, van Eenbergen M, Denollet J, Roukema JA, Aaronson NK, Vingerhoets A, Coebergh JW, de Vries J, Essink-Bot ML, Mols F, Profiles Registry G (2011) The Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer 47(14):2188–2194. https://doi.org/10.1016/j.ejca.2011.04.034
van Duijn C, Keij I (2002) Sociaal-economische status indicator op postcode niveau [in Dutch]. Maandstatistiek van de bevolking 50:32–35
Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN (2003) The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum 49(2):156–163. https://doi.org/10.1002/art.10993
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6):361–370
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM (1997) A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 27(2):363–370
Lambert S, Pallant JF, Girgis A (2011) Rasch analysis of the Hospital Anxiety and Depression Scale among caregivers of cancer survivors: implications for its use in psycho-oncology. Psychooncology 20(9):919–925. https://doi.org/10.1002/pon.1803
Hodgkinson K, Butow P, Hobbs KM, Hunt GE, Lo SK, Wain G (2007) Assessing unmet supportive care needs in partners of cancer survivors: the development and evaluation of the Cancer Survivors’ Partners Unmet Needs measure (CaSPUN). Psychooncology 16(9):805–813. https://doi.org/10.1002/pon.1138
Mineka S, Watson D, Clark LA (1998) Comorbidity of anxiety and unipolar mood disorders. Annu Rev Psychol 49:377–412. https://doi.org/10.1146/annurev.psych.49.1.377
Pallant JF (2010) SPSS survival manual: a step by step guide to data analysis using SPSS, 4th edn. Open University Press/McGraw-Hill, Maidenhead
Bagozzi RP, Yi Y (1989) On the use of structural equation models in experimental designs. J Mark Res 26(3):271–284. https://doi.org/10.2307/3172900
Bender R, Lange S (2001) Adjusting for multiple testing—when and how? J Clin Epidemiol 54(4):343–349
Kenny DA, Kashy DA, Cook WL (2006) Dyadic data analysis. Guilford, New York
Campbell L, Kashy DA (2002) Estimating actor, partner, and interaction effects for dyadic data using PROC MIXED and HLM: a user-friendly guide. Pers Relat 9(3):327–342
Compas BE, Worsham NL, Epping-Jordan JE, Grant KE, Mireault G, Howell DC, Malcarne VL (1994) When mom or dad has cancer: markers of psychological distress in cancer patients, spouses, and children. Health Psychol 13(6):507–515
Cadell S, Regehr C, Hemsworth D (2003) Factors contributing to posttraumatic growth: a proposed structural equation model. Am J Orthopsychiatry 73(3):279–287
Cordova MJ, Cunningham LL, Carlson CR, Andrykowski MA (2001) Posttraumatic growth following breast cancer: a controlled comparison study. Health Psychol 20(3):176–185
Jaarsma TA, Pool G, Sanderman R, Ranchor AV (2006) Psychometric properties of the Dutch version of the Posttraumatic Growth Inventory among cancer patients. Psychooncology 15(10):911–920. https://doi.org/10.1002/pon.1026
Bower JE, Kemeny ME, Taylor SE, Fahey JL (1998) Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. J Consult Clin Psychol 66(6):979–986
Tedeschi RG, Calhoun LG (1996) The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 9(3):455–471
Longacre TA, McKenney JK, Tazelaar HD, Kempson RL, Hendrickson MR (2005) Ovarian serous tumors of low malignant potential (borderline tumors): outcome-based study of 276 patients with long-term (> or =5-year) follow-up. Am J Surg Pathol 29(6):707–723
Cook WL, Kenny DA (2005) The actor–partner interdependence model: a model of bidirectional effects in developmental studies. Int J Behav Dev 29(2):101–109. https://doi.org/10.1080/01650250444000405
Singer S, Kuhnt S, Gotze H, Hauss J, Hinz A, Liebmann A, Krauss O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br J Cancer 100(6):908–912. https://doi.org/10.1038/sj.bjc.6604952
Acknowledgements
We would like to thank all patients and their doctors for their participation in the study. Special thanks go to research assistants. In addition, we want to thank the following hospitals for their cooperation: Amphia Hospital, Breda; Catharina Hospital, Eindhoven; Elkerliek Hospital, Helmond and Deurne; Jeroen Bosch Hospital, ‘s-Hertogenbosch; Maxima Medical Centre, Eindhoven and Veldhoven; Sint Anna Hospital, Geldrop; Elisabeth-TweeSteden Hospital, Tilburg and Waalwijk; VieCuri Hospital, Venlo and Venray; and Instituut Verbeeten, Tilburg.
Funding
The data collection of this study was funded by the Comprehensive Cancer Centre the Netherlands, Eindhoven, The Netherlands, and an investment grant of the Netherlands Organization for Scientific Research (NWO no. 480-08-009). NPM Ezendam is supported by a Research Fellowship from the Dutch Cancer Society (no. UVT 2014-6632). The funding sources had no involvement in the study design; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval for the study was obtained from the Medical Ethics Committee of the Elisabeth-TweeSteden Hospital. All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Camara, C., Caroline Vos, M., de Rooij, B.H. et al. The role of positive psychological changes in anxiety and depression of patients with ovarian tumors and their partners: an observational study from the population-based PROFILES registry. Support Care Cancer 27, 423–431 (2019). https://doi.org/10.1007/s00520-018-4327-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4327-6