Abstract
Purpose
Shared decision-making in acute myeloid leukemia (AML) requires understanding patients’ longitudinal experiences of illness, but little is known about the impact of remission status on patient-reported outcomes (PROs). We aimed to explore the association between remission status and PROs 6–12 months following induction chemotherapy.
Methods
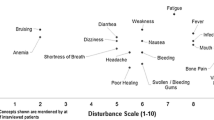
Forty-two patients completed three validated instruments characterizing symptom burden (Patient Care Monitor v2.0), distress (NCCN Distress Thermometer), and QOL (FACT-Leu), as part of a longitudinal observational study. We used regression models to explore the relationship between remission status and PROs, and explore differences by initial disease type (de novo versus secondary/relapsed AML).
Results
Those with secondary or relapsed AML at study onset had marked impairments in all measures compared to de novo AML patients. After 6 months, their mean distress score was 4.8 (> 4.0 warrants intervention), they reported a mean of 14.1 moderate/severe symptoms and had a mean QOL score of 113.6, compared to 1.0, 1.7, and 155.2, respectively, for those with de novo AML (p < .0001). Similarly, patients in relapse had a mean distress score of 5.3, a mean of 12.8 moderate/severe symptoms, and a mean QOL score of 113.4, compared to 1.8, 5.7, and 143.8, respectively, among those in remission (p < .005). These patterns persisted after adjusting for baseline differences (p < .0001).
Conclusion
Remission is associated with markedly better patient well-being in AML. Patients with secondary or relapsed AML face more severe symptom burden, distress, and QOL issues after induction. Interventions are needed to improve AML patients’ experiences of illness.




Similar content being viewed by others
References
Acute Myeloid Leukemia - Cancer Stat Facts, National Cancer Institute- SEER (2017) [Online]. Available: https://seer.cancer.gov/statfacts/html/amyl.html. Accessed: 23-May-2017
Thein MS, Ershler WB, Jemal A, Yates JW, Baer MR (2013) Outcome of older patients with acute myeloid leukemia: an analysis of SEER data over 3 decades. Cancer 119(15):2720–2727. https://doi.org/10.1002/cncr.28129
Kantarjian H, O’Brien S, Cortes J, Giles F, Faderl S, Jabbour E, Garcia-Manero G, Wierda W, Pierce S, Shan J, Estey E (2006) Results of intensive chemotherapy in 998 patients age 65 years or older with acute myeloid leukemia or high-risk myelodysplastic syndrome. Cancer 106(5):1090–1098. https://doi.org/10.1002/cncr.21723
Estey EH (2006) General approach to, and perspectives on clinical research in, older patients with newly diagnosed acute myeloid leukemia. Semin Hematol 43(2):89–95
Schlenk RF, Döhner K, Krauter J, Fröhling S, Corbacioglu A, Bullinger L, Habdank M, Späth D, Morgan M, Benner A, Schlegelberger B, Heil G, Ganser A, Döhner H, German-Austrian Acute Myeloid Leukemia Study Group (2008) Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med 358(18):1909–1918. https://doi.org/10.1056/NEJMoa074306
Boucher N, Johnson K, LeBlanc T (2017) Acute leukemia patients’ unmet needs: qualitative findings and suggested opportunities for early palliative care (SA527A). J Pain Symptom Manag 53(2):407–408. https://doi.org/10.1016/j.jpainsymman.2016.12.206
LeBlanc TW, Fish LJ, Bloom CT, El-Jawahri A, Davis DM, Locke SC, Steinhauser KE, Pollak KI (2016) Patient experiences of acute myeloid leukemia: a qualitative study about diagnosis, illness understanding, and treatment decision-making. Psychooncology. https://doi.org/10.1002/pon.4309
Stalfelt AM (1994) Quality of life during induction treatment of acute myeloid leukaemia. A comparison of three intensive chemotherapy regimens using three instruments for quality of life assessment. Acta Oncol 33(5):477–485. https://doi.org/10.3109/02841869409083922
Stalfelt AM (1994) Quality of life of patients with acute myeloid leukaemia. Leuk Res 18(4):257–267. https://doi.org/10.1016/0145-2126(94)90028-0
Schumacher A, Kessler T, Büchner T, Wewers D, van de Loo J (1998) Quality of life in adult patients with acute myeloid leukemia receiving intensive and prolonged chemotherapy—a longitudinal study. Leukemia 12(4):586–592. https://doi.org/10.1038/sj.leu.2400977
Alibhai SM et al (2007) The impact of acute myeloid leukemia and its treatment on quality of life and functional status in older adults. Crit Rev Oncol Hematol 64(1):19–30. https://doi.org/10.1016/j.critrevonc.2007.07.003
Alibhai S et al (2015) Quality of life and physical function in adults treated with intensive chemotherapy for acute myeloid leukemia improve over time independent of age. J Geriatr Oncol 6(4 // 6220–12 (LLS) *Canadian Institutes of Health Research* // 86697 (CIHR) *Canadian Institutes of Health Research*):262–271
Alibhai SMH, Leach M, Gupta V, Tomlinson GA, Brandwein JM, Saiz FS, Minden MD (2009) Quality of life beyond 6 months after diagnosis in older adults with acute myeloid leukemia. Crit Rev Oncol Hematol 69(2):168–174. https://doi.org/10.1016/j.critrevonc.2008.07.015
Sekeres MA et al (2004) Decision-making and quality of life in older adults with acute myeloid leukemia or advanced myelodysplastic syndrome. Leuk Off J Leuk Soc Am Leuk Res Fund UK 18(4):809–816
LeBlanc TW (2016) Addressing end-of-life quality gaps in hematologic cancers: the importance of early concurrent palliative care. JAMA Intern. Med. 176(2):265
LeBlanc TW and El-Jawahri A (2015) When and why should patients with hematologic malignancies see a palliative care specialist?, In: American society of hematology education program, vol. 2015, no. 1, pp. 471–478
El-Jawahri A, LeBlanc T, VanDusen H, Traeger L, Greer JA, Pirl WF, Jackson VA, Telles J, Rhodes A, Spitzer TR, McAfee S, Chen YBA, Lee SS, Temel JS (Nov. 2016) Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: a randomized clinical trial. JAMA 316(20):2094–2103. https://doi.org/10.1001/jama.2016.16786
LeBlanc TW (2017) Advance care planning and palliative care specialists in malignant hematology and stem-cell transplantation: on why it takes a village. J Oncol Pract, vol. JOP2017026. https://doi.org/10.1200/JOP.2017.026930
LeBlanc TW, Roeland EJ, El-Jawahri A (2017) Early palliative care for patients with hematologic malignancies: is it really so difficult to achieve? Curr Hematolo Malignancy Rep 12(4):300–308. https://doi.org/10.1007/s11899-017-0392-z
Kamal AH, LeBlanc TW, Meier DE (2016) Better palliative care for all: improving the lived experience with cancer. JAMA 316(1):29–30. https://doi.org/10.1001/jama.2016.6491
Loggers ET, LeBlanc TW, El-Jawahri A, Fihn J, Bumpus M, David J, Horak P, Lee SJ (2016) Pretransplantation supportive and palliative care consultation for high-risk hematopoietic cell transplantation patients. Biol Blood Marrow Transplant 22(7):1299–1305. https://doi.org/10.1016/j.bbmt.2016.03.006
Fortner B, Baldwin S, Schwartzberg L, Houts AC (2006) Validation of the cancer care monitor items for physical symptoms and treatment side effects using expert oncology nurse evaluation. J Pain Symptom Manag 31(3):207–214. https://doi.org/10.1016/j.jpainsymman.2005.07.009
Abernethy AP, Herndon JE II, Wheeler JL, Day JM, Hood L, Patwardhan M, Shaw H, Lyerly HK (2009) Feasibility and acceptability to patients of a longitudinal system for evaluating cancer-related symptoms and quality of life: pilot study of an e/Tablet data-collection system in academic oncology. J Pain Symptom Manag 37(6):1027–1038. https://doi.org/10.1016/j.jpainsymman.2008.07.011
Abernethy AP, Zafar SY, Uronis H, Wheeler JL, Coan A, Rowe K, Shelby RA, Fowler R, Herndon JE II (2010) Validation of the patient care monitor (version 2.0): a review of system assessment instrument for cancer patients. J Pain Symptom Manag 40(4):545–558. https://doi.org/10.1016/j.jpainsymman.2010.01.017
Mitchell AJ (2010) Short screening tools for cancer-related distress: a review and diagnostic validity meta-analysis. JNCCN J Natl Compr Cancer Netw 8(4):487–494. https://doi.org/10.6004/jnccn.2010.0035
Jacobsen PB, Donovan KA, Trask PC, Fleishman SB, Zabora J, Baker F, Holland JC (2005) Screening for psychologic distress in ambulatory cancer patients: a multicenter evaluation of the distress thermometer. Cancer 103(7):1494–1502. https://doi.org/10.1002/cncr.20940
Snowden A, White CA, Christie Z, Murray E, McGowan C, Scott R (2011) The clinical utility of the distress thermometer: a review. Br J Nurs 20(4):220–227. 10.12968/bjon.2011.20.4.220
Cella D et al (2012) Measuring health-related quality of life in leukemia: the functional assessment of cancer therapy—Leukemia (FACT-Leu) questionnaire. Value Heal 15(8)
Cella D, Tulsky D, Gray G (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Densitom 11:570–579
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 11(3):207–221. https://doi.org/10.1023/A:1015276414526
NCCN (2014) NCCN Clinical Practice Guidelines in Oncology: Acute Myeloid Leukemia. [Online]. Available: http://williams.medicine.wisc.edu/aml.pdf. Accessed: 05-Jun-2017
Wang C-W, Chow AY, and Chan CL (2017) The effects of life review interventions on spiritual well-being, psychological distress, and quality of life in patients with terminal or advanced cancer: a systematic review and meta-analysis of randomized controlled trials. Palliat Med, p. 26921631770510. https://doi.org/10.1177/0269216317705101
Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R (2013) Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol 31(6):782–793. https://doi.org/10.1200/JCO.2011.40.8922
Creutzfeldt A et al (2016) Integrating patient reported measures as predictive parameters into decisionmaking about palliative chemotherapy: a pilot study. BMC Palliat. Care 15(1):25
Alibhai SMH, Durbano S, Breunis H, Brandwein JM, Timilshina N, Tomlinson GA, Oh PI, Culos-Reed SN (Nov. 2015) A phase II exercise randomized controlled trial for patients with acute myeloid leukemia undergoing induction chemotherapy. Leuk Res 39(11):1178–1186. https://doi.org/10.1016/j.leukres.2015.08.012
Kurland BF, Johnson LL, Diehr PH (Dec. 2012) Accommodation of missing data in supportive and palliative care clinical trials. Curr Opin Support Palliat Care 6(4):465–470. https://doi.org/10.1097/SPC.0b013e328358441d
Funding
This research was supported by a Junior Career Development Award to Dr. LeBlanc from the National Palliative Care Research Center, and a Sojourns Scholars Award to Dr. LeBlanc from the Cambia Health Foundation. Dr. LeBlanc’s research is currently supported by the American Cancer Society (grant number 128776-MRSG-15-185-01-PCSM). Mr. Wolf is supported by the National Institutes of Health funding for the Duke Biostatistics Core (grant number UL1TR001117)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Institutional Review Board of the Duke University School of Medicine approved this protocol. Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors declare that they have no relevant conflicts of interest.
Rights and permissions
About this article
Cite this article
Kayastha, N., Wolf, S.P., Locke, S.C. et al. The impact of remission status on patients’ experiences with acute myeloid leukemia (AML): an exploratory analysis of longitudinal patient-reported outcomes data. Support Care Cancer 26, 1437–1445 (2018). https://doi.org/10.1007/s00520-017-3973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3973-4