Abstract
Purpose
This preliminary study evaluated sleep quality in long-term head and neck cancer survivors, using demographic data and clinical features of the cancers as assessment criteria. In addition, a possible correlation was examined between scores on self-rated questionnaires of sleep quality and assessments of quality of life and oral health status.
Methods
Subjects were 77 head and neck cancer survivors. Sleep quality was evaluated using the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale. Oral and general health status was assessed using The Oral Health Impact Profile (OHIP-14) and the Short-Form Health Survey (SF-36), respectively, and correlated with clinical parameters. Spearman’s correlation coefficients were calculated to examine relationships between variables. Logistic regression analysis was performed to identify independent variables associated with poor sleep quality.
Results
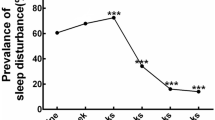
Eighty-three percent of patients had poor sleep quality (global scores ≥5) and 40% had a global Pittsburgh Sleep Quality Index score ≥8, indicating significantly poor sleep quality. Nocturnal enuresis, daytime sleepiness, and early morning awakening were the most common complaints. Extensive neck dissection, a lower SF-36 mental component score, and a higher OHIP-14 psychological disability score were independently associated with poor sleep quality. OHIP-14 global score was linked independently with daytime sleepiness.
Conclusion
This is the first study to demonstrate a high prevalence of poor sleep quality in long-term head and neck cancer survivors. Extensive neck dissection, poor mental health, and psychological disability may contribute to poor sleep quality. Maintaining good oral health-related quality of life could promote better sleep in these patients.
Similar content being viewed by others
References
Argiris A, Karamouzis MV, Raben D, Ferris RL (2008) Head and neck cancer. Lancet 371:1695–1709
Aziz NM (2007) Cancer survivorship research: state of knowledge, challenges and opportunities. Acta Oncol 46:417–432
Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A (2004) Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manag 27:140–148
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP (2005) Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer 114:806–816
Duffy SA, Khan MJ, Ronis DL, Fowler KE, Gruber SB, Wolf GT, Terrell JE (2008) Health behaviors of head and neck cancer patients the first year after diagnosis. Head Neck 30:93–102
Duffy SA, Ronis DL, McLean S, Fowler KE, Gruber SB, Wolf GT, Terrell JE (2009) Pretreatment health behaviors predict survival among patients with head and neck squamous cell carcinoma. J Clin Oncol 27:1969–1975
Emami E, Lavigne G, De Grandmont P, Rompré PH, Feine JS (2012) Perceived sleep quality among edentulous elders. Gerodontology 29:e128–e134
Faiz SA, Balachandran D, Hessel AC, Lei X, Beadle BM, William WN, Bashoura L (2014) Sleep-related breathing disorders in patients with tumors in the head and neck region. Oncologist 19:1200–1206
Fiorentino L, Ancoli-Israel S (2007) Sleep dysfunction in patients with cancer. Curr Treat Options Neurol 9:337–346
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K (1998) Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 51:1037–1044
Gooneratne NS, Dean GE, Rogers AE, Nkwuo JE, Coyne JC, Kaiser LR (2007) Sleep and quality of life in long-term lung cancer survivors. Lung Cancer 58:403–410
Grant M, McMullen CK, Altschuler A, Mohler MJ, Hornbrook MC, Herrinton LJ, Wendel CS, Baldwin CM, Krouse RS (2011) Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncol Nurs Forum 38: 587–596
Johns M (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR (2002) Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59:131–136
Lee K, Cho M, Miaskowski C, Dodd M (2004) Impaired sleep and rhythms in persons with cancer. Sleep Med Rev 8:199–212
Mercadante S, Girelli D, Casuccio A (2004) Sleep disorders in advanced cancer patients: prevalence and factors associated. Support Care Cancer 12:355–359
Morin CM (2000) The nature of insomnia and the need to refine our diagnostic criteria. Psychosom Med 62:483–485
Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Gennatas K, Smyrniotis V, Vassiliou I (2007) The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep 30:737
Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Patiraki E, Galanos A, Vlahos L (2007) Sleep quality in advanced cancer patients. J Psychosom Res 62:527–533
Nesse W, Hoekema A, Stegenga B, van der Hoeven J, de Bont L, Roodenburg J (2006) Prevalence of obstructive sleep apnoea following head and neck cancer treatment: a cross-sectional study. Oral Oncol 42:107–113
Rogers LQ, Courneya KS, Robbins KT, Rao K, Malone J, Seiz A, Reminger S, Markwell SJ, Burra V (2008) Factors associated with fatigue, sleep, and cognitive function among patients with head and neck cancer. Head Neck 30:1310–1317
Sateia MJ, Lang BJ (2008) Sleep and cancer: recent developments. Curr Oncol Rep 10:309–318
Sato Y, Kaiba Y, Yamaga E, Minakuchi S (2012) Reliability and validity of a Japanese version of the Oral Health Impact Profile for edentulous subjects. Gerodontology 29:1033–e1037
Shuman AG, Duffy SA, Ronis DL, Garetz SL, McLean SA, Fowler KE, Terrell JE (2010) Predictors of poor sleep quality among head and neck cancer patients. Laryngoscope 120:1166–1172
Slater G, Pengo MF, Kosky C, Steier J (2013) Obesity as an independent predictor of subjective excessive daytime sleepiness. Respir Med 107:305–309
Theobald DE (2004) Cancer pain, fatigue, distress, and insomnia in cancer patients. Clin Cornerstone 6:S15–S21
Acknowledgements
We would like to thank the patients and their families for their participation in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The experimental procedures were approved by the ethics committee of Tokyo Medical and Dental University (no. 1191). All subjects gave written informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Awarded first place in the poster competition at the 63rd Annual Meeting of the American Academy of Maxillofacial Prosthetics (AAMP); October 1–4, 2016; San Diego, California.
Rights and permissions
About this article
Cite this article
Li, N., Otomaru, T. & Taniguchi, H. Sleep quality in long-term survivors of head and neck cancer: preliminary findings. Support Care Cancer 25, 3741–3748 (2017). https://doi.org/10.1007/s00520-017-3804-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3804-7