Abstract
Purpose
We aimed to evaluate the effectiveness of intervention by a perioperative multidisciplinary support team for radical esophagectomy for esophageal cancer.
Methods
We retrospectively reviewed 85 consecutive patients with esophageal cancer who underwent radical esophagectomy via right thoracotomy or thoracoscopic surgery with gastric tube reconstruction. Twenty-one patients were enrolled in the non-intervention group (group N) from May 2011 to September 2012, 31 patients in the perioperative rehabilitation group (group R) from October 2012 to April 2014, and 33 patients in the multidisciplinary support team group (group S) from May 2014 to September 2015.
Results
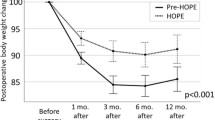
Morbidity rates were 38, 45.2, and 42.4% for groups N, R, and S, respectively. Although there were no significant differences in the incidence of pneumonia among the groups, the durations of fever and C-reactive protein positivity were shorter in group S. Moreover, postoperative oral intake commenced earlier [5.9 (5–8) days] and postoperative hospital stay was shorter [19.6 (13–29) days] for group S.
Conclusions
The intervention by a perioperative multidisciplinary support team for radical esophagectomy was effective in preventing the progression and prolongation of pneumonia as well as earlier ambulation, oral feeding, and shortening of postoperative hospitalization.

Similar content being viewed by others
References
Jafari MD, Halabi WJ, Smith BR, Nguyen VQ, Phelan MJ, Stamos MJ, Nguyen NT (2013) A decade analysis of trends and outcomes of partial versus total esophagectomy in the United States. Ann Surg 258:450–458
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Sugihara K, Mori M (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Markar S, Gronnier C, Duhamel A, Bigourdan JM, Badic B, du Rieu MC, Lefevre JH, Turner K, Luc G, Mariette C (2015) Pattern of postoperative mortality after esophageal cancer resection according to center volume: results from a large European multicenter study. Ann Surg Oncol 22:2615–2623
Kataoka K, Takeuchi H, Mizusawa J, Igaki H, Ozawa S, Abe T, Nakamura K, Kato K, Ando N, Kitagawa Y (2016) Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg (Jun 8) [Epub ahead of print]
Low DE, Alderson D, Cecconello I, Chang AC, Darling GE, DʼJourno XB, Griffin SM, Hölscher AH, Hofstetter WL, Jobe BA, Kitagawa Y, Kucharczuk JC, Law SY, Lerut TE, Maynard N, Pera M, Peters JH, Pramesh CS, Reynolds JV, Smithers BM, van Lanschot JJ (2015) International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 262:286–294
Cao S, Zhao G, Cui J, Dong Q, Qi S, Xin Y, Shen B, Guo Q (2013) Fast-track rehabilitation program and conventional care after esophagectomy: a retrospective controlled cohort study. Support Care Cancer 21:707–714
Li C, Ferri LE, Mulder DS, Ncuti A, Neville A, Lee L, Kaneva P, Watson D, Vassiliou M, Carli F, Feldman LS (2012) An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery 152:606–614
Munitiz V, Martinez-de-Haro LF, Ortiz A, Ruiz-de-Angulo D, Pastor P, Parrilla P (2010) Effectiveness of a written clinical pathway for enhanced recovery after transthoracic (Ivor Lewis) oesophagectomy. Br J Surg 97:714–718
Jiang K, Cheng L, Wang JJ, Li JS, Nie J (2009) Fast track clinical pathway implications in esophagogastrectomy. World J Gastroenterol 15:496–501
Cerfolio RJ, Bryant AS, Bass CS, Alexander JR, Bartolucci AA (2004) Fast tracking after Ivor Lewis esophagogastrectomy. Chest 126:1187–1194
Low DE, Kunz S, Schembre D, Otero H, Malpass T, Hsi A, Song G, Hinke R, Kozarek RA (2007) Esophagectomy—it’s not just about mortality anymore: standardized perioperative clinical pathways improve outcomes in patients with esophageal cancer. J Gastrointest Surg 11:1395–1402
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198
Maessen J, Dejong CH, Hausel J, Nygren J, Lassen K, Andersen J, Kessels AG, Revhaug A, Kehlet H, Ljungqvist O, Fearon KC, von Meyenfeldt MF (2007) A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg 94:224–231
Japan Esophageal Society (2015) Japanese classification of esophageal cancer, 11th edn. Kanehara, Tokyo
Kuwano H, Nishimura Y, Oyama T, Kato H, Kitagawa Y, Kusano M, Shimada H, Takiuchi H, Toh Y, Doki Y, Naomoto Y, Matsubara H, Miyazaki T, Muto M, Yanagisawa A (2015) Guidelines for diagnosis and treatment of carcinoma of the esophagus April 2012 edited by the Japan Esophageal Society. Esophagus 12:1–30
American Thoracic Society and Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Feeney C, Hussey J, Carey M, Reynolds JV (2010) Assessment of physical fitness for esophageal surgery, and targeting interventions to optimize outcomes. Dis Esophagus 23:529–539
Hulzebos EH, Helders PJ, Favié NJ, De Bie RA, Brutel de la Riviere A, Van Meeteren NL (2006) Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 296:1851–1857
Algar FJ, Alvarez A, Salvatierra A, Baamonde C, Aranda JL, López-Pujol FJ (2003) Predicting pulmonary complications after pneumonectomy for lung cancer. Eur J Cardiothorac Surg 23:201–208
Dronkers J, Veldman A, Hoberg E, van der Waal C, van Meeteren N (2008) Prevention of pulmonary complications after upper abdominal surgery by preoperative intensive inspiratory muscle training: a randomized controlled pilot study. Clin Rehabil 22:134–142
Lunardi AC, Cecconello I, Carvalho CR (2011) Postoperative chest physical therapy prevents respiratory complications in patients undergoing esophagectomy. Rev Bras Fisioter 15:160–165
Ito N, Iwaya T, Ikeda K, Kimura Y, Akiyama Y, Konosu M, Ishida K, Fujiwara H, Otsuka K, Nitta H, Kashiwaba M, Koeda K, Nishizuka S, Mizuno M, Sasaki A, Wakabayashi G (2014) Hyperglycemia 3 days after esophageal cancer surgery is associated with an increased risk of postoperative infection. J Gastrointest Surg 18:1547–1556
Acknowledgments
We thank Hiromi Oikawa, Akiko Hatakeyama, Yukiko Shimazaki, Miki Sato, Yuki Suzuki, Yoshie Kakisawa, Takahiro Honda, Yusuke Fujii, Minako Isurugi, Shiho Osuka, Kazumi Ono, Jun-ichi Asaka, Takashi Omoto, Dr. Akiko Abe, Dr. Katsumi Sanjo, and the members of the PMST group of Iwate Medical University School of Medicine. This work was supported by JSPS KAKENHI Grant Number JP26461995.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial ties to disclose. All authors have full control of the primary data and agree to allow the journal to review the data when requested.
Rights and permissions
About this article
Cite this article
Akiyama, Y., Iwaya, T., Endo, F. et al. Effectiveness of intervention with a perioperative multidisciplinary support team for radical esophagectomy. Support Care Cancer 25, 3733–3739 (2017). https://doi.org/10.1007/s00520-017-3801-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3801-x