Summary
Background
Hemoglobin A1c (HbA1c) is the major form of glycosylated hemoglobin. There are conflicting data on changes in HbA1c levels in patients with iron deficiency anemia (IDA). The present study aimed to investigate the effects of HbA1c levels in the presence of IDA, the effects of iron treatment on HbA1c levels, as well as the relationship between the severity of anemia and HbA1c levels in patients without diabetes.
Design and methods
A total of 263 patients without diabetes mellitus (DM) who were admitted to Cukurova University, Faculty of Medicine, Department of Endocrinology and Hematology or who were followed up in this clinic and diagnosed as having IDA were included in the study. A total of 131 patients had IDA. The control group comprised 132 age-matched and sex-matched healthy individuals.
Results
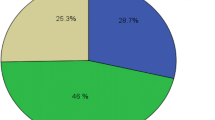
The mean HbA1c level was significantly lower in the group with IDA (5.4%) than in the healthy control group (5.9%; p < 0.05). When the patients were divided into three groups according to the severity of anemia through Hb levels, HbA1c levels were observed to decrease as the severity of the anemia increased (5.5%, 5.4%, and 5%, respectively; p > 0.05). The HbA1c levels of the patients with IDA were higher after iron therapy (from 5.4 ± 0.5 to 5.5 ± 0.3; p = 0.057). The mean hemoglobin (Hb), hematocrit (Hct), mean cell volume (MCV), mean corpusculer hemoglobin (MCH), and ferritin values also increased after iron therapy (p < 0.05).
Conclusion
The study results showed that IDA was associated with low HbA1c levels, and increased after iron therapy. Based on the study findings, it is necessary to consider the possible effects of IDA on HbA1c levels.
Similar content being viewed by others
References
Kim C, Bullard KM, Herman WH, Beckles GL. Association between iron deficiency and A1C levels among adults without diabetes in the national health and nutrition examination survey, 1999-2006. Diabetes Care. 2010;33:780–5.
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet. 1998;352:837–53.
Telen MJ, Kaufman RE. The mature erythrocyte. In: Greer JP, Forester J, et al., editors. Wintrobe’s clinical hematology. 11th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. p. 230.
Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008;93:2447–53.
International Expert Committee. International expert committee report on the role of A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34.
Ioannou GN, Spector J, Scott K, Rockey DC. Iron deficiency and gastrointestinal malignancy. A population-based cohort study. Am J Med. 2002;113:281–7.
Wu AC, Lesperance L, Bernstein H. Screening for iron deficiency. Pediatr Rev. 2002;23:171–8.
DeMaeyer EM, Adiels-Tegman M. The prevalence of anemia in the world. World Health Stat Q. 1985;38:302–16.
Peterson KP, Pavlovich JG, Goldstein D, Little R, England J, Peterson CM. What is hemoglobin A1c? An analysis of glycated hemoglobins by electrospray ionization mass spectrometry. Clin Chem. 1998;44:1951–8.
Duffy TP. Mikrositik ve hipokromik anemiler. In: Goldman L, Ausiello D, editors. Cecil textbook of medicine. İstanbul: Güneş Kitabevi; 2006. pp. 1003–8.
Brooks AP, Metcalfe J, Day JL, Edwards MS. Iron deficiency and glycosylated haemoglobin A1. Lancet. 1980;316(8186):141.
Gram-Hansen P, Eriksen J, Mourits-Andersen T, Olesen L. Glycosylated haemoglobin (HbA1c) in iron- and vitamin B12 deficiency. J Intern Med. 1990;227(2):133–6.
Coban E, Ozdogan M, Timuragaoglu A. Effect of iron deficiency anemia on the levels of hemoglobin A1c in nondiabetic patients. Acta Haematol. 2004;112(3):126–8.
El-Agouza I, Abu Shahla A, Sirdah M. The effect of iron deficiency anaemia on the levels of haemoglobin subtypes: possible consequences for clinical diagnosis. Clin Lab Haematol. 2002;24(28):285–9.
Ford ES, Cowie CC, Li C, Handelsman Y, Bloomgarden ZT. Iron-deficiency anemia, non-iron-deficiency anemia and HbA1c among adults in the US. J Diabetes. 2011;3:67–73.
Sinha N, Mishra TK, Singh T, Gupta N. Effect of iron deficiency anemia on hemoglobin A1c levels. Ann Lab Med. 2012;32(1):17–22. https://doi.org/10.3343/alm.2012.32.1.17.
Prosenz J, Öhlinger T, Müllner EW, et al. Glycated hemoglobin concentrations of red blood cells minimally increase during storage under standard blood banking conditions. Transfusion. 2019;59(2):454–445.
Eberentz-Lhomme C, Ducrocq R, Intrator S, Elion J, Nunez E, Assan R. Haemoglobinopathies: a pitfall in the assessment of glycosylated haemoglobin by ion-exchange chromatography. Diabetologia. 1984;27:596–8.
van Heyningen C, Dalton RG. Glycosylated haemoglobin in iron-deficiency anaemia. Lancet. 1985;1(8433):874.
Goldstein DE, Peth SB, England JD, Hess RL, DaCosta J. Effects of acute changes in blood glucose on HbA1c. Diabetes. 1980;29(8):623–8.
Sluiter WJ, van Essen LH, Reitsma WD, Doorenbos H. Glycosylated haemoglobin and iron deficiency. Lancet. 1980;2(8193):531–2.
Silva JF, Pimentel AL, Camargo JL. Effect of iron deficiency anaemia on HbA1c levels is dependent on the degree of anaemia. Clin Biochem. 2016;49:117–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Çetinkaya Altuntaş, M. Evran, E. Gürkan, M. Sert, and T. Tetiker declare that they have no competing interests.
Ethical standards
The study protocol was approved by the Ethics Committee of Faculty of Medicine Non-invasive Clinical Trials Ethics Committee of Cukurova University (No: 51/Date: 04.03.2016). Written informed consent was obtained from each participant. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Çetinkaya Altuntaş, S., Evran, M., Gürkan, E. et al. HbA1c level decreases in iron deficiency anemia. Wien Klin Wochenschr 133, 102–106 (2021). https://doi.org/10.1007/s00508-020-01661-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01661-6