Abstract
Background
We aimed to evaluate the role of obesity on the clinical course and response to treatment in patients with Henoch-Schonlein purpura (HSP).
Methods
Data charts of children with HSP followed in a tertiary hospital between 2000 and 2018 were reviewed retrospectively. Persistent purpura was defined as skin involvement persisting for ≥ 30 days. Mild nephropathy was defined as the presence of microscopical hematuria and/or non-nephrotic proteinuria, while severe nephropathy as nephrotic proteinuria, nephritic syndrome, and/or kidney insufficiency. Obese and non-obese patients were compared for demographic, clinical, and laboratory parameters.
Results
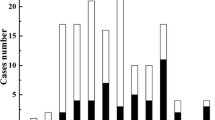
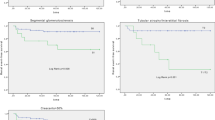
There were 199 patients (M/F, 104/95; median (IQR) presenting age 7.1 (5.0–9.2) years; follow-up period 17.5 (6–50) months). Obese patients (n = 35 (17.6%)) had significantly higher rate of persistent purpura (46% vs 21%), severe renal involvement (58% vs 31%), high-grade renal histopathological lesions (83% vs 39%), hypertension (29% vs 9%), and increased erythrocyte sedimentation rate (79% vs 56%). Obese patients also showed delayed improvement of cutaneous (25 vs 14 days), articular (12.5 vs 10.0 days), and kidney (280 vs 57 days) symptoms. Obese children used steroids for significantly longer period of time (236 vs 40 days). Furthermore, need for immunosuppressive medications were higher in obese patients (40% vs 9%).
Conclusions
Obese children with HSP had higher erythrocyte sedimentation rate, hypertension, and severe renal involvement; showed delayed improvement of skin, joint, and kidney findings; and need more immunosuppressive medications and a longer period of steroid treatment. These findings may be associated with the effect of adipose tissue on inflammation.
Similar content being viewed by others
References
Yang YH, Hung CF, Hsu CR, Wang LC, Chuang YH, Lin YT, Chiang BL (2005) A nationwide survey on epidemiological characteristics of childhood Henoch-Schonlein purpura in Taiwan. Rheumatology (Oxford) 44(5):618–622
Gardner-Medwin JMM, Dolezalova P, Cummins C, Southwood TR (2002) Incidence of Henoch-Schonlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet 360(9341):1197–1202
Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, Buoncompagni A, Lazar C, Bilge I, Uziel Y, Rigante D, Cantarini L, Hilario MO, Silva CA, Alegria M, Norambuena X, Belot A, Berkun Y, Estrella AI, Olivieri AN, Alpigiani MG, Rumba I, Sztajnbok F, Tambic-Bukovac L, Breda L, Al-Mayouf S, Mihaylova D, Chasnyk V, Sengler C, Klein-Gitelman M, Djeddi D, Nuno L, Pruunsild C, Brunner J, Kondi A, Pagava K, Pederzoli S, MartiniA, Ruperto N, Paediatric Rheumatology International Trials Organisation (PRINTO) (2010) EULAR/PRINTO/PRES criteria for Henoch-Schonlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: final classification criteria. Ann Rheum Dis 69(5):798–806
Hahn D, Hodson EM, Willis NS, Craig JC (2015) Interventions for preventing and treating kidney disease in Henoch-Schonlein purpura (HSP). Cochrane Database Syst Rev 8:Cd005128
Chen SY, Kong MS (2004) Gastrointestinal manifestations and complications of Henoch-Schonlein purpura. Chang Gung Med J 27(3):175–181
Sag E, Arici ZS, Ozen S (2017) IgA vasculitis (Henoch–Schönlein purpura) in children. Expert Opin Orphan Drugs 5(5):405–410
Yang YH, Huang YH, Lin YL, Wang LC, Chuang YH, Yu HH, Lin YT, Chiang BL (2006) Circulating IgA from acute stage of childhood Henoch-Schonlein purpura can enhance endothelial interleukin (IL)-8 production through MEK/ERK signalling pathway. Clin Exp Immunol 144(2):247–253
Yang YH, Wang SJ, Chuang YH, Lin YT, Chiang BL (2002) The level of IgA antibodies to human umbilical vein endothelial cells can be enhanced by TNF-alpha treatment in children with Henoch-Schonlein purpura. Clin Exp Immunol 130(2):352–357
Pedersen JK, Svendsen AJ, Horslev-Petersen K (2007) Incidence of rheumatoid arthritis in the southern part of Denmark from 1995 to 2001. Open Rheumatol J 1:18–23
Patterson CC, Dahlquist GG, Gyurus E, Green A, Soltesz G (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 373(9680):2027–2033
Doria A, Sarzi-Puttini P, Shoenfeld Y (2008) Infections, rheumatism and autoimmunity: the conflicting relationship between humans and their environment. Autoimmun Rev 8(1):1–4
de Carvalho JF, Pereira RM, Shoenfeld Y (2009) The mosaic of autoimmunity: the role of environmental factors. Front Biosci (Elite Ed) 1:501–509
Moroni L, Bianchi I, Lleo A (2012) Geoepidemiology, gender and autoimmune disease. Autoimmun Rev 11(6–7):A386–A392
Gomez R, Conde J, Scotece M, Gomez-Reino JJ, Lago F, Gualillo O (2011) What’s new in our understanding of the role of adipokines in rheumatic diseases? Nat Rev Rheumatol 7(9):528–536
Cao H (2014) Adipocytokines in obesity and metabolic disease. J Endocrinol 220(2):T47–T59
Schwarzenberg SJ, Sinaiko AR (2006) Obesity and inflammation in children. Paediatr Respir Rev 7(4):239–246
Zhao YL, Liu ZJ, Bai XM, Wang YC, Li GH, Yan XY (2015) Obesity increases the risk of renal involvement in children with Henoch-Schonlein purpura. Eur J Pediatr 174(10):1357–1363
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL (2007) Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71(10):1028–1035
Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F, De Martino M (2005) Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum:143–153
Ozen S, Marks SD, Brogan P, Groot N, de Graeff N, Avcin T, Bader-Meunier B, Dolezalova P, Feldman BM, Kone-Paut I, Lahdenne P, McCann L, Pilkington C, Ravelli A, van Royen A, Uziel Y, Vastert B, Wulffraat N, Kamphuis S, Beresford MW (2019) European consensus-based recommendations for diagnosis and treatment of immunoglobulin A vasculitis-the SHARE initiative. Rheumatology (Oxford) 58:1607–1616
Koskela M, Ylinen E, Ukonmaanaho EM, Autio-Harmainen H, Heikkila P, Lohi J, Jauhola O, Ronkainen J, Jahnukainen T, Nuutinen M (2017) The ISKDC classification and a new semiquantitative classification for predicting outcomes of Henoch-Schonlein purpura nephritis. Pediatr Nephrol 32(7):1201–1209
Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, Yanovski JA (2017) Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 102(3):709–757
Alper Z, Ercan I, Uncu Y (2018) A meta-analysis and an evaluation of trends in obesity prevalence among children and adolescents in Turkey: 1990 through 2015. J Clin Res Pediatr Endocrinol 10(1):59–67
Gronlund MM, Kaartoaho M, Putto-Laurila A, Laitinen K (2014) Juvenile idiopathic arthritis patients with low inflammatory activity have increased adiposity. Scand J Rheumatol 43(6):488–492
Saulsbury FT (1999) Henoch-Schonlein purpura in children. Report of 100 patients and review of the literature. Medicine (Baltimore) 78(6):395–409
van Greevenbroek MMJ, Schalkwijk CG, Stehouwer CDA (2013) Obesity-associated low-grade inflammation in type 2 diabetes mellitus: causes and consequences. Neth J Med 71(4):174–187
Qin BD, Yang M, Fu HT, Ma N, Wei TT, Tang QQ, Hu Z, Liang Y, Yang Z, Zhong R (2015) Body mass index and the risk of rheumatoid arthritis: a systematic review and dose-response meta-analysis. Arthritis Res Ther 29:17–86
Cook DG, Mendall MA, Whincup PH, Carey IM, Ballam L, Morris JE, Miller GJ, Strachan DP (2000) C-reactive protein concentration in children: relationship to adiposity and other cardiovascular risk factors. Atherosclerosis 149(1):139–150
Caballero AE, Bousquet-Santos K, Robles-Osorio L, Montagnani V, Soodini G, Porramatikul S, Hamdy O, Nobrega AC, Horton ES (2008) Overweight Latino children and adolescents have marked endothelial dysfunction and subclinical vascular inflammation in association with excess body fat and insulin resistance. Diabetes Care 31(3):576–582
Sinicato NA, Postal M, Peres FA, Pelicari KD, Marini R, dos Santos AO, Ramos CD, Appenzeller S (2014) Obesity and cytokines in childhood-onset systemic lupus erythematosus. J Immunol Res 2014:162047
Yilmaz A, Emre S, Agachan B, Bilge I, Yilmaz H, Ergen A, Isbir T, Sirin A (2009) Effect of paraoxonase 1 gene polymorphisms on clinical course of Henoch-Schonlein purpura. J Nephrol 22(6):726–732
Bogdanovic R (2009) Henoch-Schonlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatr 98(12):1882–1889
Yu HH, Liu PH, Yang YH, Lee JH, Wang LC, Chen WJ, Chiang BL (2015) Chemokine MCP1/CCL2 and RANTES/CCL5 gene polymorphisms influence Henoch-Schonlein purpura susceptibility and severity. J Formos Med Assoc 114(4):347–352
Amoli MM, Thomson W, Hajeer AH, Calvino MC, Garcia-Porrua C, Ollier WE, Gonzalez-Gay MA (2002) Interleukin 1 receptor antagonist gene polymorphism is associated with severe renal involvement and renal sequelae in Henoch-Schonlein purpura. J Rheumatol 29(7):1404–1407
López-Mejías R, Genre F, Remuzgo-Martínez S, Pérez BS, Castañeda S, Llorca J, Ortego-Centeno N, Ubilla B, Mijares V, Pina T, Calvo-Río V, Miranda-Filloy JA, Parejo AN, Argila D, Sánchez-Pérez J, Rubio E, Luque ML, Blanco-Madrigal JM, Galíndez-Aguirregoikoa E, Martín J, Blanco R, González-Gay MA (2016) Interleukin 1 beta (IL1ss) rs16944 genetic variant as a genetic marker of severe renal manifestations and renal sequelae in Henoch-Schonlein purpura. Clin Exp Rheumatol 34(3 Suppl 97):84–88
Anil M, Aksu N, Kara OD, Bal A, Anil AB, Yavascan O, Un B (2009) Henoch-Schonlein purpura in children from western Turkey: a retrospective analysis of 430 cases. Turk J Pediatr 51(5):429–436
Nong BR, Huang YF, Chuang CM, Liu CC, Hsieh KS (2007) Fifteen-year experience of children with Henoch-Schonlein purpura in southern Taiwan, 1991-2005. J Microbiol Immunol Infect 40(4):371–376
Wang X, Zhu Y, Gao L, Wei S, Zhen Y, Ma Q (2016) Henoch-Schonlein purpura with joint involvement: analysis of 71 cases. Pediatr Rheumatol Online J 14(1):20
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the local ethics committee (4730-GOA) (2019/11-03).
Conflict of interest The authors declare that they have no conflicts of interest.
Additional information
There are no prior publications or submissions with any overlapping information, including studies and patients.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dundar, H.A., Pektanc, M., Bayram, M.T. et al. Obesity is associated with severe clinical course in children with Henoch-Schonlein purpura. Pediatr Nephrol 35, 2327–2333 (2020). https://doi.org/10.1007/s00467-020-04672-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04672-7