Abstract
Neonatal acute kidney injury (AKI) is common. Critically ill neonates are at risk for AKI for many reasons including the severity of their underlying illnesses, prematurity, and nephrotoxic medications. In this educational review, we highlight four clinical scenarios in which both the illness itself and the medications indicated for their treatment are risk factors for AKI: sepsis, perinatal asphyxia, patent ductus arteriosus, and necrotizing enterocolitis. We review the available evidence regarding medications commonly used in the neonatal period with known nephrotoxic potential, including gentamicin, acyclovir, indomethacin, vancomycin, piperacillin–tazobactam, and amphotericin. We aim to illustrate the complexity of decision-making involved for both neonatologists and pediatric nephrologists when managing infants with these conditions and advocate for ongoing multidisciplinary collaboration in the development of better AKI surveillance protocols and AKI mitigation strategies to improve care for these vulnerable patients.
Similar content being viewed by others
References
Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S (2013) Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr 162:725–729.e721. https://doi.org/10.1016/j.jpeds.2012.10.002
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, Chishti AS, Woroniecki R, Mammen C, Swanson JR, Sridhar S, Wong CS, Kupferman JC, Griffin RL, Askenazi DJ (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health 1:184–194. https://doi.org/10.1016/s2352-4642(17)30069-x
Criss CN, Selewski DT, Sunkara B, Gish JS, Hsieh L, McLeod JS, Robertson JO, Matusko N, Gadepalli SK (2018) Acute kidney injury in necrotizing enterocolitis predicts mortality. Pediatr Nephrol 33:503–510. https://doi.org/10.1007/s00467-017-3809-y
Gadepalli SK, Selewski DT, Drongowski RA, Mychaliska GB (2011) Acute kidney injury in congenital diaphragmatic hernia requiring extracorporeal life support: an insidious problem. J Pediatr Surg 46:630–635. https://doi.org/10.1016/j.jpedsurg.2010.11.031
Carmody JB, Swanson JR, Rhone ET, Charlton JR (2014) Recognition and reporting of AKI in very low birth weight infants. Clin J Am Soc Nephrol 9:2036–2043. https://doi.org/10.2215/cjn.05190514
Rhone ET, Carmody JB, Swanson JR, Charlton JR (2014) Nephrotoxic medication exposure in very low birth weight infants. J Matern Fetal Neonatal Med 27:1485–1490. https://doi.org/10.3109/14767058.2013.860522
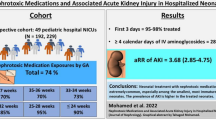
Barhight M, Altaye M, Gist KM, Isemann B, Goldstein SL, Akinbi H (2017) Nephrotoxic medications and associated acute kidney injury in very low birth weight infants. J Clin Nephrol Res 4:1070
Greenhow TL, Hung YY, Pantell RH (2016) Management and outcomes of previously healthy, full-term, febrile infants ages 7 to 90 days. Pediatrics 138(6). https://doi.org/10.1542/peds.2016-0270
Powell EC, Mahajan PV, Roosevelt G, Hoyle JD Jr, Gattu R, Cruz AT, Rogers AJ, Atabaki SM, Jaffe DM, Casper TC, Ramilo O, Kuppermann N (2018) Epidemiology of bacteremia in febrile infants aged 60 days and younger. Ann Emerg Med 71:211–216. https://doi.org/10.1016/j.annemergmed.2017.07.488
Hsieh EM, Hornik CP, Clark RH, Laughon MM, Benjamin DK Jr, Smith PB (2014) Medication use in the neonatal intensive care unit. Am J Perinatol 31:811–821. https://doi.org/10.1055/s-0033-1361933
Kent A, Turner MA, Sharland M, Heath PT (2014) Aminoglycoside toxicity in neonates: something to worry about? Exper Rev Anti Infect Ther 12:319–331
Cantey JB, Lopez-Medina E, Nguyen S, Doern C, Garcia C (2015) Empiric antibiotics for serious bacterial infection in young infants: opportunities for stewardship. Pediatr Emerg Care 31:568–571. https://doi.org/10.1097/pec.0000000000000400
Sullins AK, Abdel-Rahman SM (2013) Pharmacokinetics of antibacterial agents in the CSF of children and adolescents. Paediatr Drugs 15:93–117. https://doi.org/10.1007/s40272-013-0017-5
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR (2006) Empiric use of ampicillin and cefotaxime, compared with ampicillin and gentamicin, for neonates at risk for sepsis is associated with an increased risk of neonatal death. Pediatrics 117:67–74. https://doi.org/10.1542/peds.2005-0179
Baker CJ, Byington CL, Polin RA (2011) Policy statement—recommendations for the prevention of perinatal group B streptococcal (GBS) disease. Pediatrics 128:611–616. https://doi.org/10.1542/peds.2011-1466
Pocket book of hospital care for children: guidelines for the management of common childhood illnesses (2013). Geneva, Switzerland
Caviness AC, Demmler GJ, Almendarez Y, Selwyn BJ (2008) The prevalence of neonatal herpes simplex virus infection compared with serious bacterial illness in hospitalized neonates. J Pediatr 153:164–169. https://doi.org/10.1016/j.jpeds.2008.02.031
Hanna MH, Askenazi DJ, Selewski DT (2016) Drug-induced acute kidney injury in neonates. Curr Opin Pediatr 28:180–187. https://doi.org/10.1097/mop.0000000000000311
Kurinczuk JJ, White-Koning M, Badawi N (2010) Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev 86:329–338. https://doi.org/10.1016/j.earlhumdev.2010.05.010
Douglas-Escobar M, Weiss MD (2015) Hypoxic-ischemic encephalopathy: a review for the clinician. JAMA Pediatr 169:397–403. https://doi.org/10.1001/jamapediatrics.2014.3269
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, Polin RA, Robertson CM, Thoresen M, Whitelaw A, Gunn AJ (2005) Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 365:663–670. https://doi.org/10.1016/s0140-6736(05)17946-x
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, Fanaroff AA, Poole WK, Wright LL, Higgins RD, Finer NN, Carlo WA, Duara S, Oh W, Cotten CM, Stevenson DK, Stoll BJ, Lemons JA, Guillet R, Jobe AH (2005) Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 353:1574–1584. https://doi.org/10.1056/NEJMcps050929
Shankaran S, Pappas A, McDonald SA, Vohr BR, Hintz SR, Yolton K, Gustafson KE, Leach TM, Green C, Bara R, Petrie Huitema CM, Ehrenkranz RA, Tyson JE, Das A, Hammond J, Peralta-Carcelen M, Evans PW, Heyne RJ, Wilson-Costello DE, Vaucher YE, Bauer CR, Dusick AM, Adams-Chapman I, Goldstein RF, Guillet R, Papile LA, Higgins RD (2012) Childhood outcomes after hypothermia for neonatal encephalopathy. N Engl J Med 366:2085–2092. https://doi.org/10.1056/NEJMoa1112066
LaRosa DA, Ellery SJ, Walker DW, Dickinson H (2017) Understanding the full spectrum of organ injury following intrapartum asphyxia. Front Pediatr 5:16. https://doi.org/10.3389/fped.2017.00016
Sarkar S, Askenazi DJ, Jordan BK, Bhagat I, Bapuraj JR, Dechert RE, Selewski DT (2014) Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr Res 75:431–435. https://doi.org/10.1038/pr.2013.230
Jenik AG, Ceriani Cernadas JM, Gorenstein A, Ramirez JA, Vain N, Armadans M, Ferraris JR (2000) A randomized, double-blind, placebo-controlled trial of the effects of prophylactic theophylline on renal function in term neonates with perinatal asphyxia. Pediatrics 105:E45
Bakr AF (2005) Prophylactic theophylline to prevent renal dysfunction in newborns exposed to perinatal asphyxia—a study in a developing country. Pediatr Nephrol 20:1249–1252. https://doi.org/10.1007/s00467-005-1980-z
Eslami Z, Shajari A, Kheirandish M, Heidary A (2009) Theophylline for prevention of kidney dysfunction in neonates with severe asphyxia. Iran J Kidney Dis 3:222–226
Raina A, Pandita A, Harish R, Yachha M, Jamwal A (2016) Treating perinatal asphyxia with theophylline at birth helps to reduce the severity of renal dysfunction in term neonates. Acta Paediatr 105:e448–e451. https://doi.org/10.1111/apa.13469
Sarkar S, Barks JD, Bhagat I, Donn SM (2009) Effects of therapeutic hypothermia on multiorgan dysfunction in asphyxiated newborns: whole-body cooling versus selective head cooling. J Perinatol 29:558–563. https://doi.org/10.1038/jp.2009.37
Saikumar P, Venkatachalam MA (2003) Role of apoptosis in hypoxic/ischemic damage in the kidney. Semin Nephrol 23:511–521
Alaro D, Bashir A, Musoke R, Wanaiana L (2014) Prevalence and outcomes of acute kidney injury in term neonates with perinatal asphyxia. Afr Health Sci 14:682–688. https://doi.org/10.4314/ahs.v14i3.26
Kirkley MJ, Boohaker L, Griffin R, Soranno DE, Gien J, Askenazi D, Gist KM (2019) Acute kidney injury in neonatal encephalopathy: an evaluation of the AWAKEN database. Pediatr Nephrol 34:169–176. https://doi.org/10.1007/s00467-018-4068-2
Hadzimuratovic E, Skrablin S, Hadzimuratovic A, Dinarevic SM (2014) Postasphyxial renal injury in newborns as a prognostic factor of neurological outcome. J Matern Fetal Neonatal Med 27:407–410. https://doi.org/10.3109/14767058.2013.818646
Choi DW, Park JH, Lee SY, An SH (2018) Effect of hypothermia treatment on gentamicin pharmacokinetics in neonates with hypoxic-ischaemic encephalopathy: a systematic review and meta-analysis. J Clin Pharm Ther 43:484–492. https://doi.org/10.1111/jcpt.12711
Bijleveld YA, de Haan TR, van der Lee HJ, Groenendaal F, Dijk PH, van Heijst A, de Jonge RC, Dijkman KP, van Straaten HL, Rijken M, Zonnenberg IA, Cools F, Zecic A, Nuytemans DH, van Kaam AH, Mathot RA (2016) Altered gentamicin pharmacokinetics in term neonates undergoing controlled hypothermia. Br J Clin Pharmacol 81:1067–1077. https://doi.org/10.1111/bcp.12883
Ting JY, Kwan E, McDougal A, Osiovich H (2015) Pharmacokinetics of gentamicin in newborns with moderate-to-severe hypoxic-ischemic encephalopathy undergoing therapeutic hypothermia. Indian J Pediatr 82:119–125. https://doi.org/10.1007/s12098-014-1527-z
Cies JJ, Habib T, Bains V, Young M, Menkiti OR (2018) Population pharmacokinetics of gentamicin in neonates with hypoxemic-ischemic encephalopathy receiving controlled hypothermia. Pharmacotherapy 38:1120–1129. https://doi.org/10.1002/phar.2186
Rao SC, Srinivasjois R, Moon K (2016) One dose per day compared to multiple doses per day of gentamicin for treatment of suspected or proven sepsis in neonates. Cochrane Database Syst Rev 12:Cd005091. https://doi.org/10.1002/14651858.CD005091.pub4
Frymoyer A, Meng L, Bonifacio SL, Verotta D, Guglielmo BJ (2013) Gentamicin pharmacokinetics and dosing in neonates with hypoxic ischemic encephalopathy receiving hypothermia. Pharmacotherapy 33:718–726. https://doi.org/10.1002/phar.1263
Chock VY, Frymoyer A, Yeh CG, Van Meurs KP (2018) Renal saturation and acute kidney injury in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia. J Pediatr 200:232–239.e231. https://doi.org/10.1016/j.jpeds.2018.04.076
Sweetman DU, Molloy EJ (2013) Biomarkers of acute kidney injury in neonatal encephalopathy. Eur J Pediatr 172:305–316. https://doi.org/10.1007/s00431-012-1890-6
Benitz W (2015) Patent ductus arteriosus. Fanaroff and Martin’s neonatal-perinatal medicine, vol 10th. Elsevier Saunders, Philadelphia, PA
Gien J (2008) Controversies in the management of patent ductus arteriosus. NeoReviews 9:e477–e482. https://doi.org/10.1542/neo.9-10-e477
Fowlie PW, Davis PG, McGuire W (2010) Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Cochrane Database Syst Rev (7):Cd000174. https://doi.org/10.1002/14651858.CD000174.pub2
Slaughter JL, Reagan PB, Bapat RV, Newman TB, Klebanoff MA (2016) Nonsteroidal anti-inflammatory administration and patent ductus arteriosus ligation, a survey of practice preferences at US children’s hospitals. Eur J Pediatr 175:775–783. https://doi.org/10.1007/s00431-016-2705-y
Whelton A (1999) Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Am J Med 106:13s–24s
Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, Solimano A, Vincer M, Wright LL (2001) Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N Engl J Med 344:1966–1972. https://doi.org/10.1056/nejm200106283442602
Akima S, Kent A, Reynolds GJ, Gallagher M, Falk MC (2004) Indomethacin and renal impairment in neonates. Pediatr Nephrol 19:490–493. https://doi.org/10.1007/s00467-003-1402-z
Constance JE, Reith D, Ward RM, Balch A, Stockmann C, Korgenski EK, Thorell EA, Sherwin CMT (2017) Risk of nonsteroidal anti-inflammatory drug-associated renal dysfunction among neonates diagnosed with patent ductus arteriosus and treated with gentamicin. J Perinatol 37:1093–1102. https://doi.org/10.1038/jp.2017.80
Majed B, Bateman DA, Uy N, Lin F (2019) Patent ductus arteriosus is associated with acute kidney injury in the preterm infant. Pediatr Nephrol 34:1129–1139. https://doi.org/10.1007/s00467-019-4194-5
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, Ting JY, Sehgal A, Malikiwi A, Harabor A, Soraisham AS, McNamara PJ (2015) A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr 167:1354–1361.e1352. https://doi.org/10.1016/j.jpeds.2015.09.028
Polat TB, Celik IH, Erdeve O (2016) Early predictive echocardiographic features of hemodynamically significant patent ductus arteriosus in preterm VLBW infants. Pediatr Int 58:589–594. https://doi.org/10.1111/ped.12915
Clyman RI, Liebowitz M, Kaempf J, Erdeve O, Bulbul A, Hakansson S, Lindqvist J, Farooqi A, Katheria A, Sauberan J, Singh J, Nelson K, Wickremasinghe A, Dong L, Hassinger DC, Aucott SW, Hayashi M, Heuchan AM, Carey WA, Derrick M, Fernandez E, Sankar M, Leone T, Perez J, Serize A (2019) PDA-TOLERATE trial: an exploratory randomized controlled trial of treatment of moderate-to-large patent ductus arteriosus at 1 week of age. J Pediatr 205:41–48.e46. https://doi.org/10.1016/j.jpeds.2018.09.012
Gersony WM, Peckham GJ, Ellison RC, Miettinen OS, Nadas AS (1983) Effects of indomethacin in premature infants with patent ductus arteriosus: results of a national collaborative study. J Pediatr 102:895–906
El-Mashad AE, El-Mahdy H, El Amrousy D, Elgendy M (2017) Comparative study of the efficacy and safety of paracetamol, ibuprofen, and indomethacin in closure of patent ductus arteriosus in preterm neonates. Eur J Pediatr 176:233–240. https://doi.org/10.1007/s00431-016-2830-7
Ohlsson A, Shah PS (2018) Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low birth weight infants. Cochrane Database Syst Rev 4:Cd010061. https://doi.org/10.1002/14651858.CD010061.pub3
Van Overmeire B (2007) Common clinical and practical questions on the use of intravenous ibuprofen lysine for the treatment of patent ductus arteriosus. J Pediatr Pharmacol Ther 12:194–206. https://doi.org/10.5863/1551-6776-12.3.194
Ohlsson A, Walia R, Shah SS (2018) Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev 9:Cd003481. https://doi.org/10.1002/14651858.CD003481.pub7
Van Overmeire B, Van de Broek H, Van Laer P, Weyler J, Vanhaesebrouck P (2001) Early versus late indomethacin treatment for patent ductus arteriosus in premature infants with respiratory distress syndrome. J Pediatr 138:205–211. https://doi.org/10.1067/mpd.2001.110528
Stephens BE, Gargus RA, Walden RV, Mance M, Nye J, McKinley L, Tucker R, Vohr BR (2008) Fluid regimens in the first week of life may increase risk of patent ductus arteriosus in extremely low birth weight infants. J Perinatol 28:123–128. https://doi.org/10.1038/sj.jp.7211895
Barrington K, Brion LP (2002) Dopamine versus no treatment to prevent renal dysfunction in indomethacin-treated preterm newborn infants. Cochrane Database Syst Rev (3):Cd003213. https://doi.org/10.1002/14651858.Cd003213
Brion LP, Campbell DE (2001) Furosemide for symptomatic patent ductus arteriosus in indomethacin-treated infants. Cochrane Database Syst Rev (3):Cd001148. https://doi.org/10.1002/14651858.Cd001148
Anabrees JA, Aifaleh KM (2012) Fluid restriction and prophylactic indomethacin in extremely low birth weight infants. J Clin Neonatol 1:1–5. https://doi.org/10.4103/2249-4847.92228
Benitz WE (2016) Patent ductus arteriosus in preterm infants. Pediatrics 137:e20153730. https://doi.org/10.1542/peds.2015-3730
Hull MA, Fisher JG, Gutierrez IM, Jones BA, Kang KH, Kenny M, Zurakowski D, Modi BP, Horbar JD, Jaksic T (2014) Mortality and management of surgical necrotizing enterocolitis in very low birth weight neonates: a prospective cohort study. J Am Coll Surg 218:1148–1155. https://doi.org/10.1016/j.jamcollsurg.2013.11.015
Heida FH, Hulscher JB, Schurink M, van Vliet MJ, Kooi EM, Kasper DC, Pones M, Bos AF, Benkoe TM (2015) Bloodstream infections during the onset of necrotizing enterocolitis and their relation with the pro-inflammatory response, gut wall integrity and severity of disease in NEC. J Pediatr Surg 50:1837–1841. https://doi.org/10.1016/j.jpedsurg.2015.07.009
Lin PW, Stoll BJ (2006) Necrotising enterocolitis. Lancet 368:1271–1283. https://doi.org/10.1016/s0140-6736(06)69525-1
Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O'Neill PJ, Chow AW, Dellinger EP, Eachempati SR, Gorbach S, Hilfiker M, May AK, Nathens AB, Sawyer RG, Bartlett JG (2010) Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis 50:133–164. https://doi.org/10.1086/649554
McKamy S, Hernandez E, Jahng M, Moriwaki T, Deveikis A, Le J (2011) Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr 158:422–426. https://doi.org/10.1016/j.jpeds.2010.08.019
Carreno J, Smiraglia T, Hunter C, Tobin E, Lomaestro B (2018) Comparative incidence and excess risk of acute kidney injury in hospitalised patients receiving vancomycin and piperacillin/tazobactam in combination or as monotherapy. Int J Antimicrob Agents 52:643–650. https://doi.org/10.1016/j.ijantimicag.2018.08.001
Downes KJ, Cowden C, Laskin BL, Huang YS, Gong W, Bryan M, Fisher BT, Goldstein SL, Zaoutis TE (2017) Association of acute kidney injury with concomitant vancomycin and piperacillin/tazobactam treatment among hospitalized children. JAMA Pediatr 171:e173219. https://doi.org/10.1001/jamapediatrics.2017.3219
Maldonado NA, Cano LE, De Bedout C, Arbelaez CA, Roncancio G, Tabares AM, Robledo CG, Robledo J (2014) Association of clinical and demographic factors in invasive candidiasis caused by fluconazole-resistant Candida species: a study in 15 hospitals, Medellin, Colombia 2010-2011. Diagn Microbiol Infect Dis 79:280–286. https://doi.org/10.1016/j.diagmicrobio.2014.02.003
Butler KM, Rench MA, Baker CJ (1990) Amphotericin B as a single agent in the treatment of systemic candidiasis in neonates. Pediatr Infect Dis J 9:51–56. https://doi.org/10.1097/00006454-199001000-00012
Autmizguine J, Tan S, Cohen-Wolkowiez M, Cotten CM, Wiederhold N, Goldberg RN, Adams-Chapman I, Stoll BJ, Smith PB, Benjamin DK Jr (2018) Antifungal susceptibility and clinical outcome in neonatal candidiasis. Pediatr Infect Dis J 37:923–929. https://doi.org/10.1097/inf.0000000000001913
Horwitz E, Shavit O, Shouval R, Hoffman A, Shapiro M, Moses AE (2012) Evaluating real-life clinical and economical burden of amphotericin-B deoxycholate adverse reactions. Int J Clin Pharm 34:611–617. https://doi.org/10.1007/s11096-012-9654-y
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD (2016) Executive summary: clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:409–417. https://doi.org/10.1093/cid/civ1194
Ascher SB, Smith PB, Watt K, Benjamin DK, Cohen-Wolkowiez M, Clark RH, Benjamin DK Jr, Moran C (2012) Antifungal therapy and outcomes in infants with invasive Candida infections. Pediatr Infect Dis J 31:439–443. https://doi.org/10.1097/INF.0b013e3182467a72
Manzoni P, Galletto P, Rizzollo S, Franco C, Gallo E, Antonucci R, Fanos V, Farina D (2012) Liposomal amphotericin B does not induce nephrotoxicity or renal function impairment in premature neonates. Early Hum Dev 88(Suppl 2):S86–S91. https://doi.org/10.1016/s0378-3782(12)70024-5
Karadag-Oncel E, Ozsurekci Y, Yurdakok M, Kara A (2013) Is liposomal amphotericin B really safety in neonates? Early Hum Dev 89:35–36. https://doi.org/10.1016/j.earlhumdev.2012.07.015
Scarcella A, Pasquariello MB, Giugliano B, Vendemmia M, de Lucia A (1998) Liposomal amphotericin B treatment for neonatal fungal infections. Pediatr Infect Dis J 17:146–148
Silver C, Rostas S (2018) Comprehensive drug utilization review in neonates: liposomal amphotericin B. J Pharm Pharmacol 70:328–334. https://doi.org/10.1111/jphp.12878
Goldman RD, Koren G (2004) Amphotericin B nephrotoxicity in children. J Pediatr Hematol Oncol 26:421–426
Carmody JB, Harer MW, Denotti AR, Swanson JR, Charlton JR (2016) Caffeine exposure and risk of acute kidney injury in a retrospective cohort of very low birth weight neonates. J Pediatr 172:63–68.e61. https://doi.org/10.1016/j.jpeds.2016.01.051
Harer MW, Askenazi DJ, Boohaker LJ, Carmody JB, Griffin RL, Guillet R, Selewski DT, Swanson JR, Charlton JR (2018) Association between early caffeine citrate administration and risk of acute kidney injury in preterm neonates: results from the AWAKEN study. JAMA Pediatr 172:e180322. https://doi.org/10.1001/jamapediatrics.2018.0322
Bhat MA, Shah ZA, Makhdoomi MS, Mufti MH (2006) Theophylline for renal function in term neonates with perinatal asphyxia: a randomized, placebo-controlled trial. J Pediatr 149:180–184. https://doi.org/10.1016/j.jpeds.2006.03.053
Al-Wassia H, Alshaikh B, Sauve R (2013) Prophylactic theophylline for the prevention of severe renal dysfunction in term and post-term neonates with perinatal asphyxia: a systematic review and meta-analysis of randomized controlled trials. J Perinatol 33:271–277. https://doi.org/10.1038/jp.2012.97
KDIGO (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Bellos I, Iliopoulos DC, Perrea DN (2019) Pharmacological interventions for the prevention of acute kidney injury after pediatric cardiac surgery: a network meta-analysis. Clin Exp Nephrol 23:782–791. https://doi.org/10.1007/s10157-019-01706-9
Kent AL, Charlton JR, Guillet R, Gist KM, Hanna M, El Samra A, Fletcher J, Selewski DT, Mammen C (2018) Neonatal acute kidney injury: a survey of neonatologists’ and nephrologists’ perceptions and practice management. Am J Perinatol 35:1–9. https://doi.org/10.1055/s-0037-1604260
Goldstein SL, Kirkendall E, Nguyen H, Schaffzin JK, Bucuvalas J, Bracke T, Seid M, Ashby M, Foertmeyer N, Brunner L, Lesko A, Barclay C, Lannon C, Muething S (2013) Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132:e756–e767. https://doi.org/10.1542/peds.2013-0794
Kashani K, Rosner MH, Haase M, Lewington AJP, O’Donoghue DJ, Wilson FP, Nadim MK, Silver SA, Zarbock A, Ostermann M, Mehta RL, Kane-Gill SL, Ding X, Pickkers P, Bihorac A, Siew ED, Barreto EF, Macedo E, Kellum JA, Palevsky PM, Tolwani AJ, Ronco C, Juncos LA, Rewa OG, Bagshaw SM, Mottes TA, Koyner JL, Liu KD, Forni LG, Heung M, Wu VC (2019) Quality improvement goals for acute kidney injury. Clin J Am Soc Nephrol 14:941–953. https://doi.org/10.2215/cjn.01250119
Acknowledgments
The authors thank Liza Kramer, PharmD Candidate, Class of 2019, University of Iowa College of Pharmacy; and Whitni Patterson, Pharm D Candidate, Class of 2019, University of Iowa College of Pharmacy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Study questions’ answers
1. b; 2. a; 3. a, c, d; 4. a; 5. b
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murphy, H.J., Thomas, B., Van Wyk, B. et al. Nephrotoxic medications and acute kidney injury risk factors in the neonatal intensive care unit: clinical challenges for neonatologists and nephrologists. Pediatr Nephrol 35, 2077–2088 (2020). https://doi.org/10.1007/s00467-019-04350-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04350-3