Abstract
Background
Third-space endoscopy requires a delicate and accurate insufflation technique to secure the endoscopic visualization and maintain the working space. However, optimal third-space insufflation parameters have yet to be determined. The aim of this study was to assess: (1) the diversity of endoluminal third-space pressure by manual insufflation, and (2) the performance of the insufflation settings for third-space endoscopy.
Methods
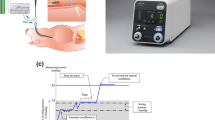
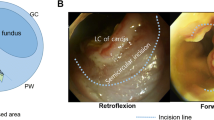
A submucosal tunnel was created in the upper posterior wall of the porcine stomach. Using two-channel esophagogastroduodenoscopy, one channel was used for insufflation and the other was used for pressure measurement. Experiment 1 Endoluminal submucosal tunnel pressure was measured in a 10-cm submucosal tunnel of a single porcine. Six board-certified endoscopists in turn maintained what they considered sufficient exposure under manual insufflation. Experiment 2 Endoluminal submucosal tunnel pressure and number of insufflations were measured using the pressure-regulated insufflation device; the differences in the submucosal tunnel length (long: 10-cm, short: 4-cm) and the insufflation route diameter (large: 3.8-mm, small: 2.2-mm) were compared.
Results
Experiment 1 The endoluminal submucosal tunnel pressure profiles during third-space endoscopy varied between endoscopists. Experiment 2 Longer submucosal tunnels and larger insufflation route diameters lead to stable endoluminal submucosal tunnel pressure. The gap with the preset pressure of the insufflator and endoluminal pressure narrowed, and the required number of insufflations decreased with longer tunnel length and larger route diameter.
Conclusions
The pressure dynamics in third-space endoscopy differed among endoscopists. Longer submucosal tunnels and larger insufflation route diameters lead to stable endoluminal submucosal tunnel pressure.







Similar content being viewed by others
References
Khashab MA, Pasricha PJ (2013) Conquering the third space: challenges and opportunities for diagnostic and therapeutic endoscopy. Gastrointest Endosc 77:146–148
Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV (2004) Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 60:114–117
Bowman DE (2006) ASGE/SAGES working group on natural orifice translumenal endoscopic surgery white paper October 2005. Gastrointest Endosc 63:199–203
Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA, Marler RJ (2007) Submucosal endoscopy with mucosal flap safety valve. Gastrointest Endosc 65:688–694
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Kawai M, Peretta S, Burckhardt O, Dallemagne B, Marescaux J, Tanigawa N (2012) Endoscopic pyloromyotomy: a new concept of minimally invasive surgery for pyloric stenosis. Endoscopy 44:169–173
Khashab MA, Stein E, Clarke JO, Saxena P, Kumbhari V, Chander Roland B, Kalloo AN, Stavropoulos S, Pasricha P, Inoue H (2013) Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc 78:764–768
Li QL, Chen WF, Zhang XC, Cai MY, Zhang YQ, Hu JW, He MJ, Yao LQ, Zhou PH, Xu MD (2016) Submucosal tunneling endoscopic septum division: a novel technique for treating Zenker’s diverticulum. Gastroenterology 151:1071–1074
Bapaye A, Wagholikar G, Jog S, Kothurkar A, Purandare S, Dubale N, Pujari R, Mahadik M, Vyas V, Bapaye J (2016) Per rectal endoscopic myotomy for the treatment of adult Hirschsprung’s disease: First human case (with video). Dig Endosc 28:680–684
Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ, Yao LQ (2012) Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc 75:195–199
Werner YB, von Renteln D, Noder T, Schachschal G, Denzer UW, Groth S, Nast JF, Kersten JF, Petzoldt M, Adam G, Mann O, Repici A, Hassan C, Rosch T (2017) Early adverse events of per-oral endoscopic myotomy. Gastrointest Endosc 85:708-718.e702
Song S, Wang X, Zhang S, Li Y, Zhang X, Chu X (2018) Efficacy and complications of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors and exploration for influencing factors. Z Gastroenterol 56:365–373
Nabi Z, Reddy DN, Ramchandani M (2018) Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc 87:4–17
Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L (2012) Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 26:3267–3272
Zhang XC, Li QL, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ, Hu JW, Cai MY, Yao LQ, Zhou PH (2016) Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy 48:967–978
Hirota M, Miyazaki Y, Takahashi T, Yamasaki M, Takiguchi S, Mori M, Doki Y, Nakajima K (2014) Dynamic article: steady pressure CO2 colonoscopy; its feasibility and underlying mechanism. Dis Colon Rectum 57:1120–1128
Imaeda H, Nakajima K, Hosoe N, Nakahara M, Zushi S, Kato M, Kashiwagi K, Matsumoto Y, Kimura K, Nakamura R, Wada N, Tsujii M, Yahagi N, Hibi T, Kanai T, Takehara T, Ogata H (2016) Percutaneous endoscopic gastrostomy under steady pressure automatically controlled endoscopy: first clinical series. World J Gastrointest Endosc 8:186–191
Kato M, Nakajima K, Yamada T, Hirota M, Miyazaki Y, Yamasaki M, Nishida T, Mori M, Doki Y, Tsujii M, Takehara T (2014) Esophageal submucosal dissection under steady pressure automatically controlled endoscopy (SPACE): a clinical feasibility study. Endoscopy 46:680–684
Nakajima K, Moon JH, Tsutsui S, Miyazaki Y, Yamasaki M, Yamada T, Kato M, Yasuda K, Sumiyama K, Yahagi N, Saida Y, Kondo H, Nishida T, Mori M, Doki Y (2012) Esophageal submucosal dissection under steady pressure automatically controlled endoscopy (SPACE): a randomized preclinical trial. Endoscopy 44:1139–1148
Yamada T, Hirota M, Tsutsui S, Kato M, Takahashi T, Yasuda K, Sumiyama K, Tsujii M, Takehara T, Mori M, Doki Y, Nakajima K (2015) Gastric endoscopic submucosal dissection under steady pressure automatically controlled endoscopy (SPACE); a multicenter randomized preclinical trial. Surg Endosc 29:2748–2755
Kamba S, Kobayashi M, Koizumi A, Ono S, Hara Y, Shimamoto N, Matsui H, Furuhashi H, Ohya TR, Tamai N, Nishikawa M, Nakajima K, Sumiyama K (2019) Intra-abdominal pressure during endoscopic full-thickness resection comparing manual and automatic control insufflation: a block-randomized porcine study. Surg Endosc 34:1625–1633
Maydeo A, Dhir V (2017) Third-space endoscopy: stretching the limits. Gastrointest Endosc 85:728–729
Sumiyama K, Tajiri H, Gostout CJ (2008) Submucosal endoscopy with mucosal flap safety valve (SEMF) technique: a safe access method into the peritoneal cavity and mediastinum. Minim Invasive Ther Allied Technol 17:365–369
Nabi Z, Nageshwar Reddy D, Ramchandani M (2018) Recent advances in third-space endoscopy. Gastroenterol Hepatol (N Y) 14:224–232
Youn YH, Minami H, Chiu PW, Park H (2016) Peroral endoscopic myotomy for treating achalasia and esophageal motility disorders. J Neurogastroenterol Motil 22:14–24
Saxena P, Khashab MA (2016) New NOTES clinical training and program development. Gastrointest Endosc Clin N Am 26:385–400
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77:719–725
Patel KS, Calixte R, Modayil RJ, Friedel D, Brathwaite CE, Stavropoulos SN (2015) The light at the end of the tunnel: a single-operator learning curve analysis for per oral endoscopic myotomy. Gastrointest Endosc 81:1181–1187
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES (2014) Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 18:92–98; discussion 98–99
Funding
This research was partly funded by Research Grant from Japan Consortium for Advanced Surgical Endoscopy (J-CASE 2018).
Author information
Authors and Affiliations
Contributions
NU designed the study and U wrote the initial draft of the manuscript. NU also contributed to the interpretation of the data and to the critical revision of the manuscript for important intellectual content. All the other authors (M, YY, T, Y, S, T, M, T, K, MY, E, D) contributed to data collection and interpretation and critical review of the manuscript. All the authors have read and approved the final version of the manuscript and have agreed to the accountability of all aspects of the study, ensuring that any queries related to the accuracy or integrity of any part of the work are answerable.
Corresponding author
Ethics declarations
Disclosures
Drs. Yuki Ushimaru, Noriko Matsuura, Yasushi Yamasaki, Yoji Takeuchi, Kotaro Yamashita, Takuro Saito, Koji Tanaka, Tomoki Makino, Tsuyoshi Takahashi, Yukinori Kurokawa, Makoto Yamasaki, Hidetoshi Eguchi, Yuichiro Doki, and Kiyokazu Nakajima have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures in this study were performed in accordance with the ethical standards of the responsible committee on institutional animal experimentation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ushimaru, Y., Matsuura, N., Yamasaki, Y. et al. Optimization of insufflation and pressure control in third-space endoscopy. Surg Endosc 36, 817–825 (2022). https://doi.org/10.1007/s00464-021-08319-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08319-y