Abstract
Background
Anastomotic leakage (AL) and major complications after colorectal resection for deep infiltrating endometriosis (DIE) have a remarkable impact on patient outcomes. The aim of this study is to assess the predictive value of C-reactive protein (CRP), procalcitonin (PCT), white blood cell count (WBCs) and the Dutch Leakage Score (DLS) as reliable markers in the early diagnosis of AL and major complications after laparoscopic colorectal resection for DIE.
Methods
262 consecutive women undergoing laparoscopic colorectal resection for DIE between September 2017 and September 2018 were prospectively enrolled. WBCs, CRP, PCT and DLS were recorded at baseline and on postoperative day (POD) 2, 3 and 6 then statistically analyzed as predictors of AL and severe postoperative complications.
Results
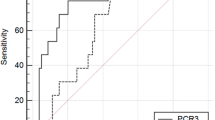
The AL rate was 3.2%. The major morbidity rate was 11.2%. No postoperative mortality was recorded. The postoperative trend of DLS and serum levels of CRP and PCT, but not WBCs, were significantly higher in women developing AL and severe complications. DLS had better sensitivity and specificity than biomarkers on all postoperative days as a predictor of AL and major complications. CRP and PCT have a low positive predictive value (PPV) and a high negative predictive value (NPV) for AL and major complications on POD3 and POD6. The risk of malnutrition was significantly related to AL.
Conclusions
The combination of DLS as a standardized postoperative clinical monitoring system and CRP and PCT as serum biomarkers, allows the exclusion of AL and major complications in the early postoperative period after laparoscopic colorectal resection for DIE, thus ensuring a safe patient discharge.

Similar content being viewed by others
References
Turco LC, Scaldaferri F, Chiantera V et al (2020) Long-term evaluation of quality of life and gastrointestinal well-being after segmental colo-rectal resection for deep infiltrating endometriosis (ENDO-RESECT QoL). Arch Gynecol Obstet 301:217–228
Ek M, Roth B, Ekström P, Valentin L, Bengtsson M, Ohlsson B (2015) Gastrointestinal symptoms among endometriosis patients—a case-cohort study. BMC Womens Health 15:59
Nezhat C, Li A, Falik R et al (2018) Bowel endometriosis: diagnosis and management. Am J Obstet Gynecol 218:549–562
Habib N, Centini G, Lazzeri L et al (2020) Bowel endometriosis: current perspectives on diagnosis and treatment. Int J Womens Health 12:35–47
Ip JCY, Chua TC, Wong SW, Krishnan S (2020) Rectal disc resection improves stool frequency in patients with deep infiltrating endometriosis: a prospective study. Aust N Z J Obstet Gynaecol 60:454–458
Ceccaroni M, Clarizia R, Roviglione G (2020) Nerve-sparing surgery for deep infiltrating endometriosis: laparoscopic eradication of deep infiltrating endometriosis with rectal and parametrial resection according to the Negrar method. J Minim Invasive Gynecol 27:263–264
Duffy JM, Arambage K, Correa FJ et al (2014) Laparoscopic surgery for endometriosis. Cochrane Database Syst Rev 3(4):CD011031
Abo C, Bendifallah S, Jayot A et al (2019) Discoid resection for colorectal endometriosis: results from a prospective cohort from two French tertiary referral centres. Colorectal Dis 21:1312–1320
Kingham TP, Pachter HL (2009) Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am Coll Surg 208:269–278
Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA (2007) Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg 245:254–258
Platell C, Barwood N, Dorfmann G, Makin G (2007) The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis 9:71–79
Scattarelli A, Carriou M, Boulet L et al (2019) C-reactive protein assessment to predict early septic complications after laparoscopic bowel resection for endometriosis: a diagnostic study. BJOG 126:1176–1182
Riiskjær M, Forman A, Kesmodel US, Andersen LM, Ljungmann K, Seyer-Hansen M (2017) Diagnostic value of serial measurement of C-reactive protein in the detection of a surgical complication after laparoscopic bowel resection for endometriosis. Gynecol Obstet Investig 824:410–416
van Rooijen SJ, Jongen AC, Wu ZQ et al (2017) Definition of colorectal anastomotic leakage: a consensus survey among Dutch and Chinese colorectal surgeons. World J Gastroenterol 23:6172–6180
Vallance A, Wexner S, Berho M et al (2017) A collaborative review of the current concepts and challenges of anastomotic leaks in colorectal surgery. Colorectal Dis 19:O1–O12
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102:462–479
Italian ColoRectal Anastomotic Leakage (iCral) Study Group (2020) Anastomotic leakage after elective colorectal surgery: a prospective multicentre observational study on use of the Dutch leakage score, serum procalcitonin and serum C-reactive protein for diagnosis. BJS Open 4:499–507
Muñoz JL, Alvarez MO, Cuquerella V et al (2018) Procalcitonin and C-reactive protein as early markers of anastomotic leak after laparoscopic colorectal surgery within an enhanced recovery after surgery (ERAS) program. Surg Endosc 32:4003–4010
Warschkow R, Beutner U, Steffen T et al (2012) Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg 256:245–250
Giaccaglia V, Salvi PF, Antonelli MS et al (2016) Procalcitonin reveals early dehiscence in colorectal surgery: the PREDICS Study. Ann Surg 263:967–972
Facy O, Paquette B, Orry D et al (2016) Diagnostic accuracy of inflammatory markers as early predictors of infection after elective colorectal surgery: results from the IMACORS Study. Ann Surg 263:961–966
Cousin F, Ortega-Deballon P et al (2016) Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery: a meta-analysis. Ann Surg 264:252–256
American Society for Reproductive Medicine (1996) Revised American Society for Reproductive Medicine classification of endometriosis. Fertil Steril 67:817–821
Kaiser MJ, Bauer JM, Ramsch C et al (2009) Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 13:782–788
den Dulk M, Noter SL, Hendriks ER et al (2009) Improved diagnosis and treatment of anastomotic leakage after colorectal surgery. Eur J Surg Oncol 35:420–426
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Garcia-Granero A, Frasson M, Flor-Lorente B et al (2013) Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum 56:475–483
Correia MI, Waitzberg DL (2003) The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr 22:235–239
Norman K, Pichard C, Lochs H, Pirlich M (2008) Prognostic impact of disease-related malnutrition. Clin Nutr 27:5–15
Gustafsson UO, Scott MJ, Hubner M et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg 43:659–695
Nelson G, Bakkum-Gamez J, Kalogera E et al (2019) Guidelines for perioperative care in gynecologic/oncology: enhanced recovery after surgery (ERAS) society recommendations-2019 update. Int J Gynecol Cancer 29:651–668
Jie B, Jiang ZM, Nolan MT, Zhu SN, Yu K, Kondrup J (2012) Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 28:1022–1027
Waitzberg DL, Saito H, Plank LD et al (2006) Postsurgical infections are reduced with specialized nutrition support. World J Surg 30:1592–1604
Acknowledgements
The authors thank Nicoletta De Santis, data manager, Unità per la Ricerca Clinica, IRCCS Sacro Cuore Don Calabria Hospital, Via Don A. Sempreboni 5, 37024, Negrar di Valpolicella, Verona, Italy. The authors thank Elinor Julie Rae Anderson, medical writer freelance, for her linguistic revision of the manuscript.
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Elisa Bertocchi, Giuliano Barugola, Marcello Ceccaroni, Massimo Guerriero, Roberto Rossini, Irene Gentile and Giacomo Ruffo declare that they have no conflict of interest and nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bertocchi, E., Barugola, G., Ceccaroni, M. et al. Laparoscopic colorectal resection for deep infiltrating endometriosis: can we reliably predict anastomotic leakage and major postoperative complications in the early postoperative period?. Surg Endosc 36, 422–429 (2022). https://doi.org/10.1007/s00464-021-08301-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08301-8