Abstract
Background and study aims
Endoscopic submucosal dissection (ESD) is commonly used in Asia for resection of large non-pedunculated colorectal polyps (LNPCPs) and early (T1) colorectal cancers. It allows for en bloc removal and is often curative. We describe outcomes of colorectal ESD from a United States (US) academic medical center and compare this to international experiences.
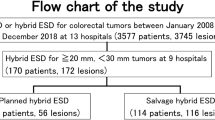
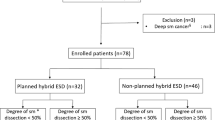
Methods
Retrospective review was performed of colonic lesions referred to the University of Chicago Medical Center for ESD from 2012 to 2020. Clinical and procedural data were collected.
Results
The study included 78 lesions with mean size of 29.7 mm (range 10–100 mm). The overall en bloc resection rate was 73.1% (n = 57). Between the first and second half of the study, it improved from 61.5 to 84.6% (p = 0.02). Histology showed adenocarcinoma in fifteen lesions (19.2%). Of all neoplastic lesions (n = 68), resection with negative margins (R0) was achieved in 54 cases (79.4%). Adverse events occurred in 9 cases (11.5%), but most (n = 6, 66.7%) were successfully treated endoscopically. Follow-up endoscopy was performed in 46 patients (59.0%) at a mean interval of 6.8 months (SD ± 5.0 months) with two case of recurrent lesion (4.3%).
Conclusions
This study shows successful colorectal ESD outcomes at a US tertiary center. The en bloc resection rate was lower than other cohorts, but a learning curve was demonstrated. The R0 resection, lesion recurrence, and adverse event rates were similar to other non-Asian experiences, but not as favorable as in Asia [Fuccio et al. in Gastrointest Endosc 86:74–86.e17, 2017]. Increased ESD training in the US can help optimize utilization and outcomes.

Similar content being viewed by others
References
Fuccio L, Hassan C, Ponchon T et al (2017) Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc 86(1):74-86.e17
Mannath J, Subramanian V, Singh R et al (2011) Polyp recurrence after endoscopic mucosal resection of sessile and flat colonic adenomas. Dig Dis Sci 56(8):2389–2395
Heitman SJ, Bourke MJ (2017) Endoscopic submucosal dissection and EMR for large colorectal polyps: “the perfect is the enemy of good.” Gastrointest Endosc 86:87–89
Rex DK, Hassan C, Dewitt JM (2017) Colorectal endoscopic submucosal dissection in the United States: why do we hear so much about it and do so little of it? Gastrointest Endosc 85:554–558
Fujishiro M (2018) Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J Gastroenterol 21:4289–4295
Russo P, Barbeiro S, Awadie H, Libânio D, Dinis-Ribeiro M, Bourke M (2019) Management of colorectal laterally spreading tumors: a systematic review and meta-analysis. Endosc Int Open 7(2):E239–E259
Hassan C, Repici A, Sharma P et al (2016) Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut 65(5):806–820
Fujiya M, Tanaka K, Dokoshi T et al (2015) Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 81(3):583–595
De Ceglie A, Hassan C, Mangiavillano B et al (2016) Endoscopic mucosal resection and endoscopic submucosal dissection for colorectal lesions: a systematic review. Crit Rev Oncol Hematol 104:138–155
Arezzo A, Passera R, Marchese N, Galloro G, Manta R, Cirocchi R (2016) Systematic review and meta-analysis of endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal lesions. United Eur Gastroenterol J 4(1):18–29
Saito Y (2015) Indication for colorectal ESD. In: Fukami N (ed) Endoscopic submucosal dissection. Springer, New York, pp 19–24
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T et al (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47(9):829–854
Tanaka S, Kashida H, Saito Y et al (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27(4):417–434
Lang GD, Konda VJ, Siddiqui UD et al (2015) A single-center experience of endoscopic submucosal dissection performed in a Western setting. Dig Dis Sci 60(2):531–536
Kikuchi R, Takano M, Takagi K et al (1995) Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum 38:1286–1295
Ge PS, Jirapinyo P, Ohaya TR et al (2019) Predicting outcomes in colorectal endoscopic submucosal dissection: a United States experience. Surg Endosc 33:4016–4025
Yang D, Alhara H, Perbtani Y et al (2019) Safety and efficacy of endoscopic submucosal dissection for rectal neoplasia: a multicenter North American experience. Endosc Int Open 07:E1714–E1722
Saito Y, Uraoka T, Yamaguchi Y et al (2010) A multi-center retrospective study of 1,111 colorectal endoscopic submucosal dissections (ESD). Gastrointest Endosc 72(6):1217–1225
Lee E, Lee JB, Lee SH et al (2013) Endoscopy submucosal dissection for colorectal tumors-1,000 colorectal ESD cases: one specialized institute’s experiences. Surg Endosc 27(1):31–39
Oka S, Tanka S, Saito Y et al (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707
Emmanuel A, Gulati S, Burt M, Hayee B, Haji A (2019) Outcomes of endoscopic resection of large colorectal lesions subjected to prior failed resection or substantial manipulation. Int J Colorectal Dis 34(6):1033–1041
Pimentel-Nunes P, Pioche M, Albeniz E et al (2019) Curriculum for endoscopic submucosal dissection training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 51:980–992
Saito Y, Fukuzawa M, Matsuda T et al (2010) Clinical outcomes of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24:343–352
Lee EJ, Lee JB, Lee SH et al (2012) Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg Endosc 26:2220–2230
Fuccio L, Ponchon T (2017) Colorectal endoscopic submucosal dissection (ESD). Best Pract Res Clin Gastroenterol 31(4):473–480
Probst A, Ebigbo A, Markle B et al (2017) Endoscopic submucosal dissection for early rectal neoplasia: experience from a European Center. Endoscopy 49:222–232
Stier MW, Chapman CG, Krietman A et al (2018) Dissection-Enabled SCaffold Assisted Resection – DeSCAR – A novel technique for resection of residual or non-lifting gastrointestinal neoplasia. Gastrointest Endosc 87:843–851
Funding
None.
Author information
Authors and Affiliations
Contributions
NG: study concept and design, acquisition of data, analysis and interpretation of data, statistical analysis, drafting of the manuscript; GRR: study concept and design, acquisition of data, drafting of the manuscript; UDS: acquisition of data, review of the manuscript; CGC: acquisition of data, review of the manuscript; KD: acquisition of data; JH: provided pathology data; SYX: provided pathology data; IW: study concept and design, acquisition of data, analysis and interpretation of data, statistical analysis, revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Dr. Uzma Siddiqui is a consultant for ConMed, Boston Scientific, Medtronic and Olympus. Dr. Irving Waxman is a consultant for Boston Scientific, Medtronic, Olympus, and Cook Medical. Dr. Nina Gupta, Dr. Gabriela Rodriquez-Ruiz, Dr. Chapman, Dr. Kianoush Donboli, Dr. John Hart, and Dr. Shu-Yuan Xiao have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guarantor of the article: Irving Waxman, MD.
Rights and permissions
About this article
Cite this article
Gupta, N., Rodríguez-Ruiz, G., Siddiqui, U.D. et al. Endoscopic submucosal dissection for colorectal lesions: outcomes from a United States experience. Surg Endosc 36, 236–243 (2022). https://doi.org/10.1007/s00464-020-08262-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08262-4