Abstract
Background
Laparoscopic pancreaticoduodenectomy (LPD) is technically demanding and there is much controversy about its safety. We evaluated the learning curve for pure LPD based on the clinical outcomes of consecutive patients treated by a single surgeon.
Methods
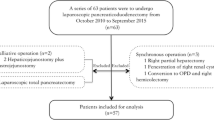
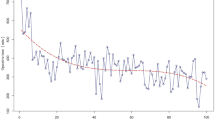
We reviewed the medical records of 119 consecutive patients who underwent LPD by a single surgeon between June 2013 and August 2018. The learning curve was evaluated using the cumulative summation (CUSUM) and risk-adjusted CUSUM (RA-CUSUM) methods. Perioperative outcomes were compared among the learning curve phases.
Results
CUSUM analysis of the operation time showed that the operation time improved after the 47th case. RA-CUSUM analysis showed the learning curve for surgical failure, defined as severe complications (Clavien–Dindo grade ≥ 3) or open conversion, comprised three phases (phase 1: cases 1–60; phase 2: cases 61–83; phase 3: cases 84–119). There were no significant differences in operation time among the three phases. Intraoperative blood loss decreased significantly over the three phases (P = 0.032). There were no postoperative deaths. The rates of postoperative complications, pancreatic fistula (grade B/C), and post-pancreatic hemorrhage were significantly lower in phase 3 than in phase 2 (2.8% vs. 21.7%, P = 0.019; 2.8% vs. 17.4%, P = 0.049; 0% vs. 13.0%, P = 0.026), but not between phases 1 and 2. Postoperative hospital stay decreased progressively, and was significantly shorter in phase 3 than in phase 1 (9.1 vs. 16.7 days, P = 0.001).
Conclusions
The LPD failure rate decreased after the first 60 cases and stabilized after 84 cases. For safe dissemination of LPD, it is important to shorten the long learning curve and decrease the unfavorable outcomes in the early phase of the learning curve.


Similar content being viewed by others
References
Cuschieri A (1994) Laparoscopic surgery of the pancreas. J R Coll Surg Edinb 39:178–184
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8:408–410. https://doi.org/10.1007/bf00642443
Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Schmidt MC, Merchant NB, Parikh AA, Martin RC, Scoggins CR, Ahmad S, Kim H, Park J, Johnston F, Strouch MJ, Menze A, Rymer J, McClaine R, Strasberg S, Talamonti MS, Staley CA, McMasters KM, Lowy AM, Byrd-Sellers J, Wood WC, Hawkins WG (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248:438–446. https://doi.org/10.1097/sla.0b013e318185a990
Yoon Y-S, Lee K, Han H-S, Cho J, Jang J, Kim S-W, Lee W, Kang C, Park S-J, Han S-S, Ahn Y, Yu H, Choi I (2014) Effects of laparoscopic versus open surgery on splenic vessel patency after spleen and splenic vessel-preserving distal pancreatectomy: a retrospective multicenter study. Surg Endosc 29:583–588. https://doi.org/10.1007/s00464-014-3701-9
EAES Consensus Conference Study Group, Edwin B, Sahakyan MA, Hilal M, Besselink MG, Braga M, Fabre J-M, Fernández-Cruz L, Gayet B, Kim S, Khatkov IE (2017) Laparoscopic surgery for pancreatic neoplasms: the European Association for Endoscopic Surgery clinical consensus conference. Surg Endosc 31:2023–2041. https://doi.org/10.1007/s00464-017-5414-3
Dokmak S, Ftériche F, Aussilhou B, Bensafta Y, Lévy P, Ruszniewski P, Belghiti J, Sauvanet A (2015) Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 220:831–838. https://doi.org/10.1016/j.jamcollsurg.2014.12.052
van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Group D, Hilst J, Rooij T, Bosscha K, Brinkman DJ, Dieren S, Dijkgraaf MG, Gerhards MF, Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Marsman HA, Gulik TM, Wicherts DA, Eshuis WJ, Stibbe LA, van Dijkum EJ, Hooft JE, Fockens P, Laarhoven HW, Wilmink JW, de Vijver MJ, Bijlsma MF, Verheij J, Nio YC, Lienden KP, Tienhoven G, Schoorlemmer A, Creemers G-J, Eijck CH, Koerkamp B, Bruno MJ, Eskens F, Nuyttens JJ, Pek C, der Schelling GP, Seerden TC, Patijn GA, Nieuwenhuijs VB, Groot JW, Bonsing BA, Vahrmeijer A, Swijnenburg RJ, Mieog SJ, der Harst E, Dulk M, Damink S, Dejong CH, Dam R, Vos J, Liem MS, Laarhoven C, Goor H, den Boezem PB, der Kolk MB, Stommel MW, Hermans JJ, Geenen EJ, Radema SA, Brosens LA, Scheepers JJ, Roos D, Boerma D, Riele W, Santvoort HC, Bollen TL, Wit F, Molenaar QI, Mohammad N, Leeuwen MS, Roele A, Jong KP, Meijer VE, Klaase JM, Kazemier G, Zonderhuis B, Daams F, Meijerink MR, Latenstein A, Rijssen BL, Nota C, Halsema E, Veldhuisen E, Vogel J, Janssen K, Scholten L, Daamen L, Walma M, Strijker M, Prins M, Zwart M, Suker M, Rombouts S, Mungroop T, Vissers F, Korrel M (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4:199–207. https://doi.org/10.1016/s2468-1253(19)30004-4
Adam M, Choudhury K, Dinan MA, Reed SD, Scheri RP, Blazer DG, Roman SA, Sosa JA (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262:372–377. https://doi.org/10.1097/sla.0000000000001055
Klompmaker S, van Hilst J, Wellner UF, Busch OR, Coratti A, D’Hondt M, Dokmak S, Festen S, Kerem M, Khatkov I, Lips DJ, Lombardo C, Luyer M, Manzoni A, Molenaar IQ, Rosso E, Saint-Marc O, Vansteenkiste F, Wittel UA, Bonsing B, Koerkamp B, Hilal M, Fuks D, Poves I, Keck T, Boggi U, Besselink MG, Consortium on (E-MIPS) E (2018) Outcomes after minimally-invasive versus open pancreatoduodenectomy: a Pan-European Propensity Score Matched Study. Ann Surg (publish ahead of print: NA). https://doi.org/10.1097/sla.0000000000002850
Sharpe S, Talamonti MS, Wang CE, Prinz RA, Roggin KK, Bentrem DJ, Winchester DJ, Marsh RD, Stocker SJ, Baker MS (2015) Early national experience with laparoscopic pancreaticoduodenectomy for ductal adenocarcinoma: a comparison of laparoscopic pancreaticoduodenectomy and open pancreaticoduodenectomy from the National Cancer Data Base. J Am Coll Surg 221:175–184. https://doi.org/10.1016/j.jamcollsurg.2015.04.021
Croome KP, Farnell MB, Que FG, Reid-Lombardo MK, Truty MJ, Nagorney DM, Kendrick ML (2014) Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 260:633–638; discussion 638–640. https://doi.org/10.1097/sla.0000000000000937
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 215:810–819. https://doi.org/10.1016/j.jamcollsurg.2012.08.006
Kendrick ML, Cusati D (2010) Total laparoscopic pancreaticoduodenectomy. Arch Surg Chic 145:19–23. https://doi.org/10.1001/archsurg.2009.243
Correa-Gallego C, Dinkelspiel HE, Sulimanoff I, Fisher S, Viñuela EF, Kingham PT, Fong Y, DeMatteo RP, D’Angelica MI, Jarnagin WR, Allen PJ (2014) Minimally-invasive vs open pancreaticoduodenectomy: systematic review and meta-analysis. J Am Coll Surg 218:129–139. https://doi.org/10.1016/j.jamcollsurg.2013.09.005
Gumbs AA, Rivera AM, Milone L, Hoffman JP (2011) Laparoscopic pancreatoduodenectomy: a review of 285 published cases. Ann Surg Oncol 18:1335–1341. https://doi.org/10.1245/s10434-010-1503-4
Chopinet S, Fuks D, Rinaudo M, Massol J, Gregoire E, Lamer C, Belgaumkar A, Hardwigsen J, Treut Y-P, Gayet B (2017) Postoperative bleeding after laparoscopic pancreaticoduodenectomy: the Achilles’ Heel? World J Surg 42:1138–1146. https://doi.org/10.1007/s00268-017-4269-z
van Hilst J, de Rooij T, Hilal M, Asbun HJ, Barkun J, Boggi U, Busch OR, Conlon KC, Dijkgraaf MG, Han H-S, Hansen PD, Kendrick ML, Montagnini AL, Palanivelu C, Røsok BI, Shrikhande SV, Wakabayashi G, Zeh HJ, Vollmer CM, Kooby DA, Besselink MG (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB 19:190–204. https://doi.org/10.1016/j.hpb.2017.01.011
Chen K, Pan Y, Liu X, Jiang G, Wu D, Maher H, Cai X (2017) Minimally invasive pancreaticoduodenectomy for periampullary disease: a comprehensive review of literature and meta-analysis of outcomes compared with open surgery. BMC Gastroenterol 17:120. https://doi.org/10.1186/s12876-017-0691-9
Lu C, Jin W, Mou Y-P, Zhou J, Xu X, Xia T, Zhang R, Zhou Y, Yan J, Huang C, Zhang B, Wang J (2016) Analysis of learning curve for laparoscopic pancreaticoduodenectomy. J Vis Surg 2:145. https://doi.org/10.21037/jovs.2016.07.25
Speicher PJ, Nussbaum DP, White RR, Zani S, Mosca PJ, Blazer DG, Clary BM, Pappas TN, Tyler DS, Perez A (2014) Defining the learning curve for team-based laparoscopic pancreaticoduodenectomy. Ann Surg Oncol 21:4014–4019. https://doi.org/10.1245/s10434-014-3839-7
Wang M, Meng L, Cai Y, Li Y, Wang X, Zhang Z, Peng B (2016) Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg Off J Soc Surg Aliment Tract 20:924–935. https://doi.org/10.1007/s11605-016-3105-3
Kim SC, Song KB, Jung YS, Kim YH, Park DH, Lee SS, Seo DW, Lee SK, Kim MH, Park KM, Lee YJ (2012) Short-term clinical outcomes for 100 consecutive cases of laparoscopic pylorus-preserving pancreatoduodenectomy: improvement with surgical experience. Surg Endosc 27:95–103. https://doi.org/10.1007/s00464-012-2427-9
Kuroki T, Kitasato A, Adachi T, Tanaka T, Hirabaru M, Matsushima H, Soyama A, Hidaka M, Takatsuki M, Eguchi S (2014) Learning curve for laparoscopic pancreaticoduodenectomy: a single surgeon’s experience with consecutive patients. Hepatogastroenterology 61:838–841
Nagakawa Y, Nakamura Y, Honda G, Gotoh Y, Ohtsuka T, Ban D, Nakata K, Sahara Y, Velasquez V, Takaori K, Misawa T, Kuroki T, Kawai M, Morikawa T, Yamaue H, Tanabe M, Mou Y, Lee W-J, Shrikhande SV, Conrad C, Han H-S, Tang C, Palanivelu C, Kooby DA, Asbun HJ, Wakabayashi G, Tsuchida A, Takada T, Yamamoto M, Nakamura M (2018) Learning curve and surgical factors influencing the surgical outcomes during the initial experience with laparoscopic pancreaticoduodenectomy. J Hepato-biliary-pancreat Sci 25:498–507. https://doi.org/10.1002/jhbp.586
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Bassi C, Marchegiani G, Dervenis C, Sarr M, Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Chiaro M, Falconi M, Fernandez-Cruz L, Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M, International Study Group on Pancreatic Surgery (ISGPS) (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH)—an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25. https://doi.org/10.1016/j.surg.2007.02.001
Steiner SH, Cook RJ, Farewell VT, Treasure T (2000) Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostatistics 1:441–452. https://doi.org/10.1093/biostatistics/1.4.441
Song K, Kim S, Lee W, Hwang D, Lee J, Kwon J, Park Y, Lee S, Park G (2019) Laparoscopic pancreaticoduodenectomy for periampullary tumors: lessons learned from 500 consecutive patients in a single center. Surg Endosc. https://doi.org/10.1007/s00464-019-06913-9
Chedid AD, Chedid MF, Winkelmann LV, Filho TJ, Kruel CD (2015) Achieving good perioperative outcomes after pancreaticoduodenectomy in a low-volume setting: a 25-year experience. Int Surg 100:705–711. https://doi.org/10.9738/intsurg-d-14-00176.1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sungho Kim, Yoo-Seok Yoon, Ho-Seong Han, Jai Young Cho, YoungRok Choi, and Boram Lee have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S., Yoon, YS., Han, HS. et al. Evaluation of a single surgeon’s learning curve of laparoscopic pancreaticoduodenectomy: risk-adjusted cumulative summation analysis. Surg Endosc 35, 2870–2878 (2021). https://doi.org/10.1007/s00464-020-07724-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07724-z