Abstract
Background
The comparative evidence regarding the outcomes of closure versus non-closure of mesenteric defects in laparoscopic Roux-en-Y gastric bypass (LRYGB) is poorly understood. We aimed to compare the outcomes of closure versus non-closure of mesenteric defects in LRYGB for morbid obesity.
Methods
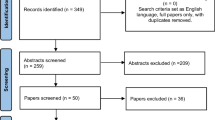
We conducted a search of electronic information sources to identify all comparative studies investigating the outcomes of closure versus non-closure of mesenteric defects in patients undergoing LRYGB for morbid obesity. We used the Cochrane risk of bias tool and the ROBINS-I tool to assess the risk of bias of RCTs and observational studies, respectively. Random or fixed effects modelling was applied as appropriate.
Results
We included 10,031 patients from six observational studies and 2609 patients from two RCTs. Analysis of observational studies showed closure defects resulted in lower risks of internal hernia (OR 0.28, 95% CI 0.15, 0.54) and reoperation for small bowel obstruction (SBO) (OR 0.30, 95% CI 0.10, 0.83); no difference was found between the two groups in terms of SBO not related to internal hernia (OR 1.19, 95% CI 0.47, 2.99), early SBO (OR 0.74, 95% CI 0.04, 14.38), anastomotic leak (OR 0.84, 95% CI 0.45, 1.57), bleeding (OR 1.08, 95% CI 0.62, 1.89), and anastomotic ulcer (OR 2.08, 95% CI 0.62, 6.94). Analysis of RCTs showed closure of defects resulted in lower risks of internal hernia (OR 0.29, 95% CI 0.19,0.45) and reoperation for SBO (OR 0.51, 95% CI 0.38, 0.69) but higher risks of SBO not related to internal hernia (OR 1.90, 95% CI 1.09, 3.34) and early SBO (OR 2.63, 95% CI 1.16, 5.96); no difference was found between the two groups in terms of anastomotic leak (OR 1.95, 95% CI 0.80, 4.72), bleeding (OR 0.67, 95% CI 0.38, 1.17), and anastomotic ulcer (OR 2.08, 95% CI 0.62, 6.94).
Conclusions
Our results suggest that closure of mesenteric defects in LRYGB may be associated with lower risks of internal herniation and reoperation for SBO compared with non-closure of the defects (moderate certainty). The available evidence is inconclusive regarding the risks of SBO not related to internal hernia and early SBO (low certainty). More RCTs are needed to improve the robustness of the available evidence.






Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H et al (2017) Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg 27(9):2279–2289
Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ et al (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234:279–289
Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux en-Y gastric bypass: incidence, treatment and prevention. Obes Surg 13:350–354
Ahmed AR, Rickards G, Husain S et al (2007) Trends in internal hernia incidence after laparoscopic Roux-en-Y gastric bypass. Obes Surg 17(12):1563–1566
Iannelli A, Facchiano E, Gugenheim J (2006) Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 16(10):1265–1271
Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO (1999) Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 13:10–13
Schneider C, Cobb W, Scott J, Carbonell A, Myers K, Bour E (2011) Rapid excess weight loss following laparoscopic gastric bypass leads to increased risk of internal hernia. Surg Endosc 25:1594–1598
Bauman RW, Pirrello JR (2009) Internal hernia at Petersen’s space after laparoscopic Roux-en-Y gastric bypass: 62% incidence without closure—a single surgeon series of 1047 cases. Surg Obes Relat Dis 5:565–570
de la Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R (2011) Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis 7:176–180
Rodriguez A, Mosti M, Sierra M et al (2010) Small bowel obstruction after antecolic and antegastric laparoscopic Roux-en-Y gastric bypass: could the incidence be reduced? Obes Surg 20:1380–1384
Geubbels N, Lijftogt N, Fiocco M, van Leersum NJ, Wouters MW, de Brauw LM (2015) Meta-analysis of internal herniation after gastric bypass surgery. Br J Surg 102(5):451–460
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Nuytens F, D'Hondt M, Van Rooy F, Vansteenkiste F, Pottel H, Abasbassi M et al (2019) Closure of mesenteric defects is associated with a higher incidence of small bowel obstruction due to adhesions after laparoscopic antecolic Roux-en-y gastric bypass: a retrospective cohort study. Int J Surg 71:149–155
Amor IB, Kassir R, Debs T, Aldeghaither S, Petrucciani N, Nunziante M et al (2019) Impact of mesenteric defect closure during laparoscopic roux-en-y gastric bypass (LRYGB): a retrospective study for a total of 2093 LRYGB. Obes Surg 29(10):3342–3347
Aghajani E, Nergaard BJ, Leifson BG, Hedenbro J, Gislason H (2017) The mesenteric defects in laparoscopic Roux-en-Y gastric bypass: 5 years follow-up of non-closure versus closure using the stapler technique. Surg Endosc 31(9):3743–3748
Chowbey P, Baijal M, Kantharia NS, Khullar R, Sharma A, Soni V (2016) Mesenteric defect closure decreases the incidence of internal hernias following laparoscopic roux-En-Y gastric bypass: a retrospective cohort study. Obes Surg 26(9):2029–2034
Stenberg E, Szabo E, Ågren G, Ottosson J, Marsk R, Lönroth H et al (2016) Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet 387(10026):1397–1404
Rosas U, Ahmed S, Leva N, Garg T, Rivas H, Lau J et al (2015) Mesenteric defect closure in laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial. Surg Endosc 29(9):2486–2490
Ribeiro-Parenti L, Arapis K, Chosidow D, Dumont JL, Demetriou M, Marmuse JP (2015) Gastrojejunostomy stricture rate: comparison between antecolic and retrocolic laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 11(5):1076–1084
Obeid A, McNeal S, Breland M, Stahl R, Clements RH, Grams J (2014) Internal hernia after laparoscopic Roux-en-Y gastric bypass. J Gastrointest Surg 18(2):250–255 (discussion 255–256)
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RM and SH contributed to conception and design. MA, AS, KAK, MMM, and SH helped with data collection. SH and SH contributed to analysis and interpretation. SH, SH, and RM involved in writing the article. All authors contributed to critical revision of the article and final approval of the article. SH and SH helped with statistical analysis.
Corresponding author
Ethics declarations
Disclosure
Shahab Hajibandeh, Shahin Hajibandeh, Mostafa Abdelkarim, Ahmad Shehadeh, Muhammad Mahid Mohsin, Khursheed Ahmed Khan and Richard Morgan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Search no. | Search strategy† |
|---|---|
#1 | MeSH descriptor: [bypass, roux en y gastric] explode all trees |
#2 | MeSH descriptor: [ anastomosis, roux en y] explode all trees |
#3 | Roux en y near2 bypass: TI,AB,KW |
#4 | Roux-en-y near2 bypass: TI,AB,KW |
#5 | #1 OR #2 OR #3 OR #4 |
#6 | Mesenteric defect: TI,AB,KW |
#7 | Petersen's defect: TI,AB,KW |
#8 | Jejunojejunal defect: TI,AB,KW |
#9 | #6 OR #7 OR #8 |
#10 | #5 AND #9 |
Combination of key words to be used in databases:
((("gastric bypass"[MeSH Terms] OR "anastomosis, roux-en-y"[MeSH Terms]) OR ("anastomosis, roux-en-y"[MeSH Terms] OR ("anastomosis"[All Fields] AND "roux-en-y"[All Fields]) OR "roux-en-y anastomosis"[All Fields] OR "roux en y bypass"[All Fields])) OR ("anastomosis, roux-en-y"[MeSH Terms] OR ("anastomosis"[All Fields] AND "roux-en-y"[All Fields]) OR "roux-en-y anastomosis"[All Fields] OR "roux en y bypass"[All Fields])) AND ((((("mesentery"[MeSH Terms] OR "mesentery"[All Fields] OR "mesenteric"[All Fields]) AND defect[All Fields]) OR (petersen's[All Fields] AND defect[All Fields])) OR (jejunojejunal[All Fields] AND defect[All Fields])) OR defect[All Fields]).
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Abdelkarim, M. et al. Closure versus non-closure of mesenteric defects in laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis. Surg Endosc 34, 3306–3320 (2020). https://doi.org/10.1007/s00464-020-07544-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07544-1