Abstract
Background
To evaluate the clinical and oncological outcomes of single-incision laparoscopic surgery (SILS) vs. conventional laparoscopic surgery (CLS) for patients with rectal cancer (RC) who underwent total mesorectal excision (TME) surgery.
Methods
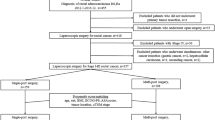
This was a retrospective case–control study of patients with RC operated between 12/2013 and 12/2017 in Ruijin Hospital North, Shanghai Jiaotong University School of Medicine. In total, 177 patients who underwent CLS and 51 who underwent SILS met the inclusion and exclusion criteria and were matched 1:1 using propensity score matching method (PSM).
Results
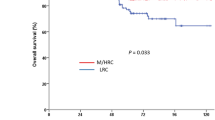
Compared with the CLS group, the SILS group showed shorter operation time [105 (40) vs. 125 (55) min, P = 0.045], shorter total incision length [4 (1) vs. 6.5 (1.5) cm, P < 0.001], lower VAS score on POD2 [1 (1) vs. 2 (1), P < 0.001], shorter time to soft diet [7 (1) vs. 8 (2) days, P = 0.048], and shorter length of hospital stay [9 (2) vs. 11 (3) days, P < 0.001]. The postoperative complications were similar between two groups [1(2%) vs. 5 (9.8%), P = 0.205]. No readmissions or mortality in either group occurred within 30 days of surgery. All 102 specimens met the requirements of TME. No significant differences were observed in the pathologic outcomes between the two groups. The median follow-up period was 32.6 months in the SILS group and 36.8 months in the CLS group (P = 0.053). The 3-year disease-free survival rates and overall survival rates of the SILS and CLS groups were 89.8% vs. 96.0% (P = 0.224) and 90.9% vs. 96.9% (P = 0.146), respectively.
Conclusions
Compared with CLS, TME surgery for rectal cancer can be performed safely and effectively using the SILS technique with better cosmetic results, less postoperative pain, faster postoperative recovery, and acceptable clinical and oncological outcomes.




Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386
Moon SY, Kim S, Lee SY, Han EC, Kang SB, Jeong SY, Park KJ, Oh JH, SEoul COlorectal Group (SECOG) (2016) Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer Med 5:1047–1054
Julien M, Dove J, Quindlen K, Halm K, Shabahang M, Wild J, Blansfield J (2016) Evolution of laparoscopic surgery for colorectal cancer: the impact of the clinical outcomes of surgical therapy group trial. Am Surg 82:685–691
Askari A, Nachiappan S, Currie A, Bottle A, Athanasiou T, Faiz O (2016) Selection for laparoscopic resection confers a survival benefit in colorectal cancer surgery in England. Surg Endosc 30:3839–3847
Cuccurullo D, Pirozzi F, Sciuto A, Bracale U, La Barbera C, Galante F, Corcione F (2015) Relaparoscopy for management of postoperative complications following colorectal surgery: ten years experience in a single center. Surg Endosc 29:1795–1803
Azin A, Saleh F, Cleghorn M, Yuen A, Jackson T, Okrainec A, Quereshy FA (2017) A comparison of endoscopic localization error rate between operating surgeons and referring endoscopists in colorectal cancer. Surg Endosc 31:1318–1326
Govaert JA, Fiocco M, van Dijk WA, Kolfschoten NE, Prins HA, Dekker JWT, Tollenaar R, Tanis PJ, Wouters M, Dutch Value Based Healthcare Study (2017) Multicenter stratified comparison of hospital costs between laparoscopic and open colorectal cancer resections: influence of tumor location and operative risk. Ann Surg 266:1021–1028
Gietelink L, Wouters MW, Bemelman WA, Dekker JW, Tollenaar RA, Tanis PJ (2016) Reduced 30-day mortality after laparoscopic colorectal cancer surgery. Ann Surg 264:135–140
Hoyuela C, Juvany M, Carvajal F (2017) Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: a systematic review and meta-analysis. Am J Surg 214:127–140
Pascual M, Salvans S, Pera M (2016) Laparoscopic colorectal surgery: current status and implementation of the latest technological innovations. World J Gastroenterol 22:704–717
Steinemann DC, Muller PC, Probst P, Schwarz AC, Buchler MW, Muller-Stich BP, Linke GR (2017) Meta-analysis of hybrid natural-orifice transluminal endoscopic surgery versus laparoscopic surgery. Br J Surg 104:977–989
Rubinkiewicz M, Nowakowski M, Wierdak M, Mizera M, Dembinski M, Pisarska M, Major P, Malczak P, Budzynski A, Pedziwiatr M (2018) Transanal total mesorectal excision for low rectal cancer: a case-matched study comparing TaTME versus standard laparoscopic TME. Cancer Manag Res 10:5239–5245
Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L, Liu H, Wang Z (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 16:380
Spanheimer PM, Armstrong JG, Fu S, Liao J, Regenbogen SE, Byrn JC (2017) Robotic proctectomy for rectal cancer: analysis of 71 patients from a single institution. Int J Med Robot Comput Assist Surg 13:e1841
Chouillard E, Alsabah S, Daher R, Younan A, Greco VJ, Chahine E, Abdullah B, Biagini J (2016) Single-incision laparoscopy could be better than standard laparoscopy in right colectomy for cancer. J Laparoendosc Adv Surg Tech A 26:371–378
Keller DS, Flores-Gonzalez JR, Ibarra S, Haas EM (2016) Review of 500 single incision laparoscopic colorectal surgery cases—lessons learned. World J Gastroenterol 22:659–667
Cianchi F, Staderini F, Badii B (2014) Single-incision laparoscopic colorectal surgery for cancer: state of art. World J Gastroenterol 20:6073–6080
Gash K, Bicsak M, Dixon A (2015) Single-incision laparoscopic surgery for rectal cancer: early results and medium-term oncological outcome. Colorectal Dis 17:1071–1078
Bucher P, Pugin F, Morel P (2008) Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis 23:1013–1016
Kim SJ, Choi BJ, Lee SC (2014) Successful total shift from multiport to single-port laparoscopic surgery in low anterior resection of colorectal cancer. Surg Endosc 28:2920–2930
Ragupathi M, Ramos-Valadez DI, Yaakovian MD, Haas EM (2011) Single-incision laparoscopic colectomy: a novel approach through a Pfannenstiel incision. Tech Coloproctol 15:61–65
Madhoun N, Keller DS, Haas EM (2015) Review of single incision laparoscopic surgery in colorectal surgery. World J Gastroenterol 21:10824–10829
Rao PP, Rao PP, Bhagwat S (2011) Single-incision laparoscopic surgery-current status and controversies. J Minim Access Surg 7:6–16
Trakarnsanga A, Akaraviputh T, Wathanaoran P, Phalanusitthepha C, Methasate A, Chinswangwattanakul V (2011) Single-incision laparoscopic colectomy without using special articulating instruments: an initial experience. World J Surg Oncol 9:162
Bulut O, Aslak KK, Levic K, Nielsen CB, Romer E, Sorensen S, Christensen IJ, Nielsen HJ (2015) A randomized pilot study on single-port versus conventional laparoscopic rectal surgery: effects on postoperative pain and the stress response to surgery. Tech Coloproctol 19:11–22
Tei M, Otsuka M, Suzuki Y, Kishi K, Tanemura M, Akamatsu H (2018) Safety and feasibility of single-port laparoscopic low anterior resection for upper rectal cancer. Am J Surg 216:1101–1106
Bush AJ, Morris SN, Millham FH, Isaacson KB (2011) Women’s preferences for minimally invasive incisions. J Minim Invasive Gynecol 18:640–643
Osborne AJ, Lim J, Gash KJ, Chaudhary B, Dixon AR (2013) Comparison of single-incision laparoscopic high anterior resection with standard laparoscopic high anterior resection. Colorectal Dis 15:329–333
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Katsuno G, Fukunaga M, Nagakari K, Yoshikawa S, Azuma D, Kohama S (2016) Short-term and long-term outcomes of singleincision versus multi-incision laparoscopic resection for colorectal cancer: a propensity-score-matched analysis of 214 cases. Surg Endosc 30:1317–1325
Miyo M, Takemasa I, Ishihara H, Hata T, Mizushima T, Ohno Y, Doki Y, Mori M (2017) Long-term outcomes of single-site laparoscopic colectomy with complete mesocolic excision for colon cancer: comparison with conventional multiport laparoscopic colectomy using propensity score matching. Dis Colon Rectum 60:664–673
Yun JA, Yun SH, Park YA, Huh JW, Cho YB, Kim HC, Lee WY (2016) Oncologic outcomes of single-incision laparoscopic surgery compared with conventional laparoscopy for colon cancer. Ann Surg 263:973–978
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047
Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE, Bonham G (2016) Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20:1–10
Alptekin H, Yilmaz H, Acar F, Kafali ME, Sahin M (2012) Incisional hernia rate may increase after single-port cholecystectomy. J Laparoendosc Adv Surg Tech A 22:731–737
Song Z, Li Y, Liu K, Jiang Y, Shi Y, Ji X, Zhang T, Wu H, Shi Y, Zhao R (2019) Clinical and oncologic outcomes of single-incision laparoscopic surgery for right colon cancer: a propensity score matching analysis. Surg Endosc 33:1117–1123
Funding
This study was supported by Advanced and Appropriate Technology Promotion Projects of Shanghai Municipal Health Commission (2019SY058). It had no involvement in study design, collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Yimei Jiang, Zijia Song, Xi Cheng, Kun Liu, Yiqin Shi, Changgang Wang, You Li, Xiaopin Ji, and Ren Zhao have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, Y., Song, Z., Cheng, X. et al. Clinical and oncological outcomes of single-incision vs. conventional laparoscopic surgery for rectal cancer. Surg Endosc 34, 5294–5303 (2020). https://doi.org/10.1007/s00464-019-07317-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07317-5