Abstract
Background
While the ACOSOG and ALaCaRT trials found that laparoscopic resections for rectal cancer failed to demonstrate non-inferiority of pathologic outcomes when compared with open resections, the COLOR II and COREAN studies demonstrated non-inferiority of clinical outcomes, leading to uncertainty regarding the value of minimally invasive (MIS) techniques in rectal cancer surgery. We analyzed differences in pathologic and clinical outcomes between open versus MIS resections for rectal cancer.
Methods
We identified patients who underwent resection for stage II or III rectal adenocarcinoma from the National Cancer Database (2010–2015). Surgical approach was categorized as open or MIS (laparoscopic or robotic). Logistic regression and Cox proportional hazard analysis were used to assess differences in outcomes and survival. Analysis was performed in an intention-to-treat fashion.
Results
A total of 31,190 patients who underwent rectal adenocarcinoma resection were identified, of whom 52.8% underwent open resection and 47.2% underwent MIS resection (31.0% laparoscopic, 16.2% robotic). After adjustment for patient, tumor, and institutional characteristics, MIS approaches were associated with significantly decreased risk of positive circumferential resection margins (OR 0.82, 95% CI 0.72–0.94), increased likelihood of harvesting ≥ 12 lymph nodes (OR 1.12, 95% CI 1.04–1.21), shorter length of stay (OR 0.57, 95% CI 0.53–0.62), and improved overall survival (HR 0.90, 95% CI 0.83–0.98).
Conclusions
MIS approaches to rectal cancer resection were associated with improved pathologic and clinical outcomes when compared to the open approach. In this nationwide, facility-based sample of cancer cases in the United States, our data suggest superiority of MIS techniques for rectal cancer treatment.
Similar content being viewed by others
Minimally invasive (MIS) techniques for colorectal cancer resection have been steadily increasing in popularity since they were first introduced in 1990 [1, 2]. For colon adenocarcinoma, multiple randomized controlled trials (RCTs) have demonstrated equivalent local recurrence rates and survival between patients who undergo laparoscopic or open colon resections, and improved short-term outcomes after laparoscopic procedures [1, 3, 4]. However, RCTs comparing laparoscopic to open approaches for rectal adenocarcinoma resection have produced contradictory results. The ACOSOG and ALaCaRT trials determined that laparoscopic resections for rectal cancer failed to meet non-inferiority criteria when compared with open resections, based on pathologic outcomes [5, 6]. In contrast, the COLOR II and COREAN studies confirmed non-inferiority of long-term clinical outcomes [7, 8], leading to uncertainty regarding the value of MIS techniques in rectal cancer surgery.
Despite equivocal data, MIS techniques have become widely incorporated into clinical practice, and have become an important component of fellowship training in colorectal surgery. Proponents of laparoscopic and robotic approaches to rectal surgery argue that smaller incisions enable faster postoperative recovery, advanced optics offer improved visualization, and wristed instruments enable easier and more meticulous dissection in the deep pelvis [2]. As MIS rectal resections are becoming more commonplace, there is a distinct need to determine ‘real-world’ results from these cases.
We analyzed patients who underwent open versus MIS resections for stage II or III rectal adenocarcinoma, using the National Cancer Database (NCDB). The primary objective of the study was to compare pathologic and clinical outcomes in patients who underwent open versus MIS rectal resections.
Methods
Study design
We conducted a retrospective analysis of patients with clinical stage II and III rectal adenocarcinoma diagnosed from January 2010 through December 2015 in the NCDB. The NCDB is a nationwide, facility-based dataset that captures 70% of all newly diagnosed malignancies in the United States (US). It is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigator.
Only patients who underwent rectal resection (low anterior resection (LAR) or abdominoperineal resection (APR)) were included in the analysis. The study period was limited to patients diagnosed between 2010 and 2015, as the NCDB did not record surgical approach until 2010. This study was exempt from Institutional Review Board review due to the de-identified nature of the database.
Variable definitions
The NCDB includes basic demographic and clinical characteristics, including age, sex, race, and Charlson/Deyo comorbidity score (CDCC) [9]. It also collects socioeconomic data, including insurance status (patient’s primary insurance carrier at the time of initial diagnosis and/or treatment), income level (median household income for each patient’s zip code between 2008 and 2012), education level (percent of adults in the patient’s zip code who did not graduate from high school between 2008 and 2012), and degree of urbanization (metropolitan, urban, or rural, based on population, as designated by the US Department of Agriculture Economic Research Service).
The NCDB additionally captures facility-level characteristics, including facility type (category classification by the CoC accreditation program, which includes community cancer programs, comprehensive community cancer programs, academic/research programs, and integrated network cancer programs) and facility region (New England, Mid Atlantic, South Atlantic, East North Central, East South Central, West North Central, West South Central, Mountain, and Pacific). CoC facility type definitions and US states contained in each facility region are defined in Appendix 1.
Facility rectal resection volume was calculated using de-identified facility identification codes assigned by the NCDB. Only facilities that submitted at least one case to the NCDB every year of the study were included, to ensure a consistent population of hospitals and to ensure that hospital volume did not appear falsely low due to lack of membership in the CoC in certain years. Only patients who underwent proctectomy for rectal adenocarcinoma were included in the volume calculations. Facilities were categorized as low (< 4.1 resections/year), middle (4.1–8.5 resections/year), or high (> 8.5 resections/year) volume, based on tertiles.
Surgical approach was classified as open, laparoscopic, laparoscopic converted to open, robotic, or robotic converted to open. Patients who underwent laparoscopic, laparoscopic converted to open, robotic, or robotic converted to open procedures were placed in the ‘MIS’ group, on an intent-to-treat basis. Patients who underwent open operations were placed in the ‘open’ group.
Clinical stage was designated based on American Joint Commission on Cancer (AJCC) 7th edition. Tumor size was defined as the largest dimension of the diameter of the primary tumor in centimeters. Circumferential margin (CRM) status (negative or positive) was obtained from final surgical pathologic analysis. Number of lymph nodes examined, node status (negative, positive, or nodes not examined), and pathologic stage were also obtained from surgical pathology. Length of hospital stay after the operation (LOS) was investigated as a continuous variable, and also categorized into < 7 days and ≥ 7 days, using the mean LOS in the ACOSOG trial as a threshold [5]. Neoadjuvant radiation was defined as receipt of radiation before primary site surgery as part of the first course of treatment. Adjuvant chemotherapy was defined as receipt of chemotherapy after primary site surgery as part of the first course of treatment. Overall survival (OS) was defined as months from diagnosis to death.
Statistical analysis
Variables were summarized as median with interquartile range (IQR) or count with percentage. Categorical variables were compared with the Pearson’s Chi squared test, and continuous variables were compared with the 2-sample t test. For each categorical outcome, multivariable logistic regression was used to adjust for surgical approach, type of resection, age, sex, race, CDCC score, clinical stage, tumor size, tumor grade, receipt of neoadjuvant radiation, insurance type, regional income quartile, regional education level, urban designation of region, facility type, facility rectal resection volume, and facility region. The regression models were clustered based on facility identification codes, to account for intra-class correlation associated within specific facilities.
Kaplan–Meier curves and Cox proportional hazard analysis were used to analyze OS. The Cox model was also clustered based on facility identification codes. Results of the logistic regressions and Cox analysis were reported as odds ratios (OR) and hazard ratios (HR), respectively, with corresponding 95% confidence intervals (CI) and p values.
All statistical analyses were performed using Stata software, version SE 14.0 (StataCorp, College Station, TX, USA). All tests were 2-sided and statistical significance was accepted at the p < 0.05 level.
Results
We identified 31,190 patients diagnosed with stage II or III rectal adenocarcinoma between 2010 and 2015, who underwent rectal resection. Of those, 16,455 (52.8%) patients underwent an open approach and 14,735 (47.2%) underwent an MIS approach. In the MIS group, 8176 (26.2% of the overall cohort) patients underwent a laparoscopic approach, 1506 (4.8%) had laparoscopic converted to open surgery, 4678 (15.0%) underwent a robotic approach, and 375 (1.2%) had robotic converted to open surgery. The conversion rate was 15.6% for laparoscopic operations and 7.4% for robotic procedures. Conversion rates decreased over the study period, from 18.6% in 2010 to 15.2% in 2015 for laparoscopic cases, and 9.7% in 2010 to 6.7% in 2015 for robotic cases. Median (IQR) follow-up time was 37.0 (24.5–53.4) months.
Independent predictors of undergoing minimally invasive approach
Univariate analysis demonstrated baseline differences between patients who underwent open versus MIS approaches (Table 1). Patients who underwent MIS operations were < 65 years old (p < 0.001), white or Asian (p < 0.001), CDCC 0 (p = 0.003), had private insurance (p < 0.001), and lived in regions with the highest income quartile (p < 0.001) and highest education level (p < 0.001). The MIS approach was associated with treatment at comprehensive community cancer programs and academic programs (p < 0.001), high-volume centers (p < 0.001), and treatment in the New England/Mid-Atlantic and Mountain/Pacific regions (p < 0.001). In terms of disease characteristics, patients with stage III disease (p < 0.001), tumors < 6 cm in size (p = 0.002), and moderately differentiated tumor grade (p < 0.001) were more likely to undergo MIS resections. The MIS approach was also associated with receipt of neoadjuvant radiation (p < 0.001) and LAR (p < 0.001).
On multivariable analysis, many of these characteristics remained significantly associated with surgical approach (Table 2). Independent predictors of the MIS approach included male sex (p = 0.04), higher regional education level (p = 0.04), treatment at comprehensive community cancer programs (p = 0.01) or academic programs (p = 0.02) compared to community cancer programs, and treatment at high-volume centers (p = 0.01). Moderately differentiated tumor grade (p = 0.03) and stage III disease (p = 0.004) were also significantly associated with MIS resection. Independent predictors of the open approach included CDCC ≥ 3 (p = 0.04), treatment in a rural region (p = 0.02), and APR (p < 0.001). Compared to patients with private insurance, patients with Medicare (p = 0.01), Medicaid (p = 0.002), and no insurance (p < 0.001) were more likely to undergo open operations. Compared to patients treated in New England/Mid-Atlantic, patients in the South Atlantic (p = 0.02), North Central (p = 0.03), and South Central (p < 0.001) regions of the US were less likely to have MIS operations.
Pathologic and clinical outcomes, based on surgical approach
Univariate analysis demonstrated differences in pathologic and clinical outcomes associated with surgical approach (Table 3). The MIS approach was associated with decreased rates of positive CRM (6.1% vs. 8.4%, p < 0.001) and increased likelihood of examining ≥ 12 lymph nodes (71.5% vs. 67.8%, p < 0.001). Patients who underwent an MIS resection had shorter LOS (median 5 (IQR 4–7) days vs. median 6 (IQR 5–9) days, p < 0.001), and lower rates of LOS ≥ 7 days (35.6% vs. 50.7%, p < 0.001), 30-day mortality (1.0% vs. 1.3%, p = 0.01), and 90-day mortality (1.9% vs. 2.6%, p < 0.001). There was no significant difference in rate of unplanned 30-day readmissions (7.7% vs. 7.1%, p = 0.052).
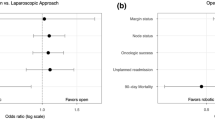
On multivariable analysis, surgical approach remained significantly associated with many of these outcomes (Table 3). The MIS approach was an independent predictor of fewer positive CRM (OR 0.82, 95% CI 0.72–0.94, p = 0.003) and increased likelihood of examining ≥ 12 nodes (OR 1.12, 95% CI 1.04–1.21, p = 0.004). The MIS approach was also significantly associated with decreased likelihood of LOS ≥ 7 days (p < 0.001), and increased rates of unplanned readmission (p = 0.04). When adjusting for pathologic stage instead of clinical stage, the MIS approach continued to be independently associated with fewer positive CRM (OR 0.84, 95% CI 0.73–0.96, p = 0.01), increased likelihood of examining ≥ 12 nodes (OR 1.16, 95% CI 1.07–1.26, p < 0.001), shorter LOS (OR 0.58, 95% CI 0.54–0.63, p < 0.001), and increased rates of unplanned readmission (OR 1.16, 95% CI 1.02–1.32, p = 0.03).
On subset analysis of only patients who underwent LAR, the same associations remained significant on multivariable analysis. Additionally, in the LAR subset, the MIS approach was associated with decreased 30-day mortality (OR 0.72, 95% CI 0.52–0.99, p = 0.04). On subset analysis of patients who underwent an MIS converted to an open approach (compared to operations that began with an open approach), there was no significant difference in rates of positive CRM (p = 0.88), LOS ≥ 7 days (p = 0.46), 30-day mortality (p = 0.88), or 90-day mortality (p = 0.69). The MIS-converted-to-open patients tended to have ≥ 12 nodes examined (OR 1.31, 95% CI 1.14–1.52, p < 0.001), and had higher rates of readmission (OR 1.35, 95% CI 1.08–1.68, p = 0.008).
Analysis of overall survival
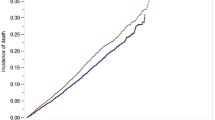
On unadjusted analysis, Kaplan–Meier curves of OS in patients with stage II and stage III rectal adenocarcinoma demonstrated improved OS in patients who underwent MIS resections (both p < 0.001) (Fig. 1A and B). Rates of 1-year and 5-year OS were 95.0% and 69.8% in patients who underwent an open approach, compared to 96.2% and 75.6% in patients who underwent an MIS approach (p < 0.05 for both 1-year and 5-year OS).
Cox proportional hazards analysis demonstrated that the MIS approach was independently associated with decreased risk of mortality (HR 0.90, 95% CI 0.83–0.98, p = 0.01) compared to the open approach (Table 4). Independent predictors of worse OS included positive CRM (p < 0.001), APR (p = 0.003), age ≥ 65 years old (p < 0.001), male sex (p < 0.001), greater comorbidities (p < 0.001), larger tumor size (p = 0.01), poorly differentiated tumor grade (p < 0.001), and advanced pathologic stage (p < 0.001). Predictors of improved OS included receipt of neoadjuvant radiation (p < 0.001), adjuvant chemotherapy (p < 0.001), and private insurance (p < 0.001).
Subset analysis of only patients who underwent LAR demonstrated the same OS advantage associated with the MIS approach (HR 0.90, 95% CI 0.82–0.99, p = 0.04). Subset analysis of patients who began with an MIS approach and were converted to open, compared to those who began with an open approach, demonstrated no significant difference in OS between the two groups (HR 1.03, 95% CI 0.88–1.22, p = 0.69).
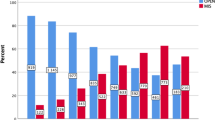
Patterns in utilization of minimally invasive approaches
Our data demonstrate a steady decline in the use of the open approach from 2010 (69.1% of cases) to 2015 (39.4% of cases) (Fig. 2A and B). During the same time-period, the use of laparoscopic and robotic approaches steadily increased (25.1% in 2010 up to 33.6% in 2015 for laparoscopic cases, and 5.8% in 2010 up to 27.1% in 2015 for robotic cases). Before 2013, most cases were performed with an open approach. However, after 2013, the majority of cases were performed, or attempted, minimally invasively.
Our data also demonstrate dramatic variations in use of laparoscopic and robotic approaches for rectal cancer resection across the US (Fig. 3A and B). For example, in the East South Central region, 63.2% of cases were performed open, 24.6% were performed laparoscopically, and 12.2% were performed robotically. On the other hand, in the Mid-Atlantic region, less than half of operations were performed open (45.8%), while 34.4% were performed laparoscopically, and nearly one in five were performed with a robotic approach (19.8%).
A and B Utilization of open versus minimally invasive approaches for rectal adenocarcinoma resection across regions of the United States. *United States regions are defined as follows: New England (CT, MA, ME, NH, RI, VT), Middle Atlantic (NJ, NY, PA), South Atlantic (DC, DE, FL, GA, MD, NC, SC, VA, WV), East North Central (IL, IN, MI, OH, WI), East South Central (AL, KY, MS, TN), West North Central (IA, KS, MN, MO, ND, NE, SD), West South Central (AR, LA, OK, TX), Mountain (AZ, CO, ID, MT, NM, NV, UT, WY), Pacific (AK, CA, HI, OR, WA)
Discussion
This study of the NCDB demonstrates that the MIS approach to rectal adenocarcinoma resection was associated with improved pathologic and clinical outcomes when compared to the open approach, even after adjusting for patient, tumor, and facility characteristics. Patients who underwent laparoscopic or robotic rectal resections were less likely to have positive circumferential resection margins and more likely to have at least 12 lymph nodes examined. MIS approaches were significantly associated with decreased LOS (though increased readmission rate), and improved overall survival. Our data show that, despite wide variations in rectal cancer treatment across the US, the MIS approach to rectal resection is a modifiable factor in the hands of surgeons proficient in both techniques, associated with improved pathologic and clinical outcomes.
These data provide useful information regarding the safety and utility of MIS techniques for rectal cancer resection, as well-known RCTs comparing laparoscopic to open approaches have produced conflicting results. The COLOR II RCT, which accrued 1044 patients from 30 European centers between 2004 and 2010, found that 3-year locoregional recurrence rates were 5.0% in both the laparoscopic and open groups, and met non-inferiority criteria [7]. The COREAN study included 340 patients with rectal cancer who received neoadjuvant chemoradiation, recruited from 3 Korean centers between 2006 and 2009 [8]. The authors found that 3-year disease-free survival (DFS) was 72.5% for the open group and 79.2% for the laparoscopic group, and also met non-inferiority criteria. Thus, both study groups concluded that laparoscopic techniques were oncologically safe for rectal adenocarcinoma resection, based on long-term clinical outcomes.
In contrast, the ACOSOG and ALaCaRT trials determined that laparoscopic resections for rectal cancer failed to meet non-inferiority criteria when compared with open operations, based on pathologic outcomes. In the ACOSOG RCT, 486 patients with stage II or III rectal cancer who received neoadjuvant therapy were recruited from 35 centers in the US and Canada between 2008 and 2013 [5]. The study authors found that ‘successful’ resection [CRM > 1 mm, negative distal margin, and completeness of total mesorectal excision (TME)] occurred in 81.7% of laparoscopic cases and 86.9% of open cases, thereby failing to meet their non-inferiority criteria. However, the recently published analysis of secondary endpoints demonstrated no significant difference in 2-year DFS or locoregional recurrence between the two groups [10]. The ALaCaRT trial, which also used pathologic measures as its primary outcome, recruited 475 patients with T1–T3 rectal adenocarcinoma from 24 sites in Australia and New Zealand between 2010 and 2014 [6]. ‘Successful’ resection (complete TME, CRM ≥ 1 mm, and distal resection margin ≥ 1 mm) was achieved in 82% of laparoscopic cases and 89% of open cases, which also failed to meet non-inferiority criteria. The authors’ analysis of secondary endpoints also found no significant difference in locoregional recurrence, 2-year DFS, or OS between the two groups [11].
A meta-analysis of 14 RCTs published between 2003 and 2015, and including the four aforementioned trials, found no difference in CRM positivity between the laparoscopic and open groups, but did find an increased risk of non-complete TME in the laparoscopic group (13.2% vs. 10.4%, p = 0.02). Comparisons of robotic to laparoscopic rectal resections are now emerging, including a retrospective study from China that demonstrated shorter LOS and earlier return of bowel function following robotic procedures and another retrospective study from France that demonstrated decreased conversion rates associated with robotic techniques [12, 13]. Interestingly, the largest RCT comparing robotic to laparoscopic rectal cancer resections, the ROLARR trial, included 471 patients from 29 sites across 10 countries, and found no significant difference in conversion rates or CRM positivity [14].
Despite these mixed results from well-regarded RCTs, our data demonstrate that MIS techniques are gaining in popularity across the US, with the majority of rectal cancer resections now being performed laparoscopically or robotically. The discrepancy between RCT results and our retrospective data illustrates the key difference between efficacy and effectiveness studies. While efficacy studies, such as the RCTs, are performed under ‘ideal and controlled circumstances’ (on carefully selected patients at specific institutions by highly trained surgeons), effectiveness studies, such as our retrospective, nationwide analysis, examine interventions under ‘real-world, usual’ circumstances (heterogeneous patient populations, variety of clinical settings, and less-monitored interventions), thereby providing more generalizable data than efficacy studies, despite the retrospective nature of the analysis [15].
When comparing efficacy and effectiveness studies of the same intervention, a larger effect of the intervention is often seen in efficacy studies, with their controlled conditions, carefully selected patients, and expert providers [15]. In fact, one study found that participants in the CLASICC trial tended to be younger and of better socioeconomic status than other patients in the national cancer registry [16]. However, we found the opposite; our retrospective data demonstrate stronger benefits associated with MIS techniques than the prospective efficacy studies. This may indicate that surgeons are attuned to predicting those patients who might benefit most from an MIS approach, thus explaining why MIS techniques were associated with improved outcomes in our retrospective study, while some randomized trials failed to meet non-inferiority criteria. It is possible that selection bias could have affected which patients in the NCDB underwent laparoscopic or open resection, though we controlled for all available patient, tumor, and facility characteristics.
Our data also provide an interesting snapshot of rates of specific outcomes in the ‘real-world.’ We found that the rate of CRM positivity was 6.1% in the MIS group, similar to the ROLARR trial (6.3% laparoscopic, 5.1% robotic) [14] and within the range of those reported by the other RCTs (3% to 12.1%) [5,6,7,8]. In our open cohort, 8.4% of patients had a positive CRM, also comparable to the RCTs, which ranged from 3% to 10%. Our data demonstrated a 12.8% conversion rate in the MIS group (15.6% laparoscopic, 7.4% robotic), similar to that reported by ROLARR (12.2% laparoscopic, 8.1% robotic) and by the other RCTs (9% to 16%, all laparoscopic). The only outlier was the COREAN trial, which reported a 1% conversion rate from laparoscopic to open [8]. In terms of survival, the 3-year OS in our MIS group (86.7%) was similar to that reported by the RCTs above (83.6% to 90.4% laparoscopic). However, the 3-year OS in our open group (81.9%) was worse than the RCTs (86.7% to 91.7% open) [7, 8]. It is reassuring that our reported rates of CRM positivity, conversion, and survival are somewhat similar to those from the RCTs, though it is important to note that our patients were cared for at CoC-accredited centers by virtue of their inclusion in the NCDB.
Interestingly, our data highlight dramatic incidental disparities and regional variations in utilization of MIS techniques in the US. The increased use of the MIS approach in men and in patients with lower CDCC scores makes sense, given the noted benefit of MIS tools in the narrow male pelvis and increased risk of morbidity associated with peritoneal insufflation in patients with severe comorbidities [5]. However, our data reveal stark disparities, as patients with private insurance were more likely to undergo MIS operations, while patients from regions with lower education levels were less likely to have MIS procedures. These findings highlight the need for continued public policy work to ensure that patients have equal access to specialized, high-quality, care, including minimally invasive resections where appropriate.
The main limitation of this study is the potential for selection bias inherent to retrospective analysis, including factors that may have affected surgeons’ choice of surgical approach that we were unable to identify or control for. Though we adjusted for all available patient, tumor, and facility characteristics, there may have been other unmeasured factors that confounded our results, such as body mass index or receipt of surgery at a ‘rectal cancer center of excellence.’ Other limitations include the fact that the NCDB does not record local or distant recurrence, disease-specific survival, TME specimen quality, or tumor distance from the anal verge. Importantly, the database also lacks information related to the specialty of the provider who performed the operation (i.e., general surgeon, colorectal surgeon, surgical oncologist, MIS surgeon). Additionally, the NCDB only includes patients who were treated at CoC centers, many of whom underwent operations at academic or comprehensive cancer centers, which may limit the generalizability of our results, though 70% of cancer diagnoses are captured in the database.
Conclusions
In this large, ‘real-world,’ facility-based sample of 70% of all newly diagnosed cancer cases in the US, our data suggest superiority of MIS techniques for rectal adenocarcinoma resection, compared to the open approach. Even after adjusting for patient, institutional, and tumor characteristics, the MIS approach was associated with improved pathologic and clinical outcomes, including lower rates of positive CRM, increased likelihood of harvesting ≥ 12 lymph nodes, LOS < 7 days, and improved OS. Since 2013, MIS techniques have been used in most rectal cancer resections across the US. However, there were marked disparities and regional variations in the utilization of MIS techniques, as patients with Medicaid or no insurance and patients from regions with lower education levels were less likely to undergo MIS procedures. Continued exploration of these disparities is urgently warranted. Our data show that, despite wide variations in rectal cancer treatment across the US, the MIS approach to rectal resection is a modifiable factor that is associated with improved pathologic and clinical outcomes.
References
Clinical Outcomes of Surgical Therapy Study G, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Moghadamyeghaneh Z, Phelan M, Smith BR, Stamos MJ (2015) Outcomes of open, laparoscopic, and robotic abdominoperineal resections in patients with rectal cancer. Dis Colon Rectum 58:1123–1129
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, Group UMCT (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, Investigators AL (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, Peters WR Jr, Maun DC, Chang GJ, Herline A, Fichera A, Mutch MG, Wexner SD, Whiteford MH, Marks J, Birnbaum E, Margolin DA, Larson DW, Marcello PW, Posner MC, Read TE, Monson JRT, Wren SM, Pisters PWT, Nelson H (2018) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269:589–595
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Wilson K, Hague W, Simes J, Australasian Gastro-Intestinal Trials Group Ai (2018) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269:596–602
Zhu XL, Yan PJ, Yao L, Liu R, Wu DW, Du BB, Yang KH, Guo TK, Yang XF (2018) Comparison of short-term outcomes between robotic-assisted and laparoscopic surgery in colorectal cancer. Surg Innov. https://doi.org/10.1177/1553350618797822
Rouanet P, Bertrand MM, Jarlier M, Mourregot A, Traore D, Taoum C, de Forges H, Colombo PE (2018) Robotic versus laparoscopic total mesorectal excision for sphincter-saving surgery: results of a single-center series of 400 consecutive patients and perspectives. Ann Surg Oncol 25:3572–3579
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Singal AG, Higgins PD, Waljee AK (2014) A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 5:e45
Morris EJ, Jordan C, Thomas JD, Cooper M, Brown JM, Thorpe H, Cameron D, Forman D, Jayne D, Quirke P, Trialists C (2011) Comparison of treatment and outcome information between a clinical trial and the National Cancer Data Repository. Br J Surg 98:299–307
Funding
GCL was supported by the National Institutes of Health T32 Research Training in Alimentary Tract Surgery Grant DK007754-13.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Grace C. Lee was supported by the NIH T32 Research Training in Alimentary Tract Surgery grant DK007754-13. Liliana G. Bordeianou is a consultant for Ethicon and legal consultant for CRICO, receives royalty fees from Up-to-Date, and receives research support from 11 Health, all outside the submitted work. Todd D. Francone is a consultant for Intuitive, outside the submitted work. Lawrence S. Blaszkowsky, Robert N. Goldstone, Rocco Ricciardi, and Hiroko Kunitake have no conflicts of interest or financial ties to disclose. Motaz Qadan is a consultant for Olympus, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hiroko Kunitake and Motaz Qadan are co-senior authors.
Appendix 1: Definitions of commission on cancer facility types and facility regions
Appendix 1: Definitions of commission on cancer facility types and facility regions
Definitions of Commission on Cancer facility types | |
Community Cancer Program | Facility accessions 100–500 newly diagnosed cancer cases each year. Training resident physicians is optional |
Comprehensive Community Cancer Program | Facility accessions > 500 newly diagnosed cancer cases each year. Training resident physicians is optional |
Academic/Research Program | Facility accessions > 500 newly diagnosed cancer cases each year. Facility participates in training resident physicians in at least four program areas, including internal medicine and general surgery |
Integrated Network Cancer Program | Multiple facilities providing integrated cancer care. At least one facility is a hospital. Training resident physicians is optional, and there is no minimum caseload requirement |
States contained in each United States facility region | |
New England | CT, MA, ME, NH, RI, VT |
Middle Atlantic | NJ, NY, PA |
South Atlantic | DC, DE, FL, GA, MD, NC, SC, VA, WV |
East North Central | IL, IN, MI, OH, WI |
East South Central | AL, KY, MS, TN |
West North Central | IA, KS, MN, MO, ND, NE, SD |
West South Central | AR, LA, OK, TX |
Mountain | AZ, CO, ID, MT, NM, NV, UT, WY |
Pacific | AK, CA, HI, OR, WA |
Rights and permissions
About this article
Cite this article
Lee, G.C., Bordeianou, L.G., Francone, T.D. et al. Superior pathologic and clinical outcomes after minimally invasive rectal cancer resection, compared to open resection. Surg Endosc 34, 3435–3448 (2020). https://doi.org/10.1007/s00464-019-07120-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07120-2