Abstract
Background
The current status of colorectal endoscopic submucosal dissection (ESD) performed by endoscopists without colorectal ESD experience is unknown. This study evaluated the quality of colorectal ESD performed by endoscopists without colorectal ESD experience.
Methods
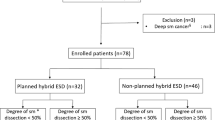
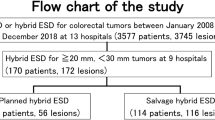
We retrospectively examined the outcomes of 420 consecutive patients with 427 superficial colorectal tumors (male/female, 251/169; mean age, 69 years) who underwent ESD. The procedures were performed by 31 endoscopists without colorectal ESD experience using needle knife-type devices at 13 hospitals from October 2008 to June 2017. Cases were divided into the first and second phases according to the experience of the endoscopist: the first phase included the first 20 cases and the second phase included case 21 and beyond. We also identified factors associated with en bloc resection failure.
Results
Rates of colonic tumors, laterally spreading tumors of the non-granular type, poor scope operability, and severe submucosal fibrosis for the first phase were significantly lower than those for the second phase. The en bloc resection rates for the first and second phases were 93% and 96%, respectively. The factors associated with en bloc resection failure were poor scope operability (odds ratio [OR] 2.6; 95% confidence interval [CI] 1.0–6.5), severe submucosal fibrosis (OR 6.5; 95% CI 2.6–15.9), and the first 20 cases (OR 3.4; 95% CI 1.2–10.1).
Conclusion
Inexperienced endoscopists should initially perform colorectal ESD for tumors without severe submucosal fibrosis under good scope operability for at least 20 cases.


Similar content being viewed by others
References
Cao Y, Liao C, Tan A, Gao Y, Mo Z, Gao F (2009) Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 41:751–757
Terasaki M, Tanaka S, Oka S, Nakadoi K, Takata S, Kanao H, Yoshidas S, Chayama K (2012) Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol 27:734–740
Oka S, Tanaka S, Saito Y, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisabe T, Tsuruta O, Sano Y, Yamano H, Shimizu S, Yahagi N, Watanabe T, Nakamura H, Fujii T, Ishikawa H, Sugihara K (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707
Tamaru Y, Oka S, Tanaka S, Hiraga Y, Kunihiro M, Nagata S, Furudoi A, Ninomiya Y, Asayama N, Shigita K, Nishiyama S, Hayashi N, Chayama K (2016) Endoscopic submucosal dissection for anorectal tumor with hemorrhoids close to the dentate line: a multicenter study of Hiroshima GI Endoscopy Study Group. Surg Endosc 30:4425–4431
Boda K, Oka S, Tanaka S, Tanaka H, Matsumoto K, Yamashita K, Sumimoto K, Hirano D, Tamaru Y, Ninomiya Y, Hayashi N, Chayama K (2018) Short-term outcomes of endoscopic submucosal dissection for superficial cecal tumors: a comparison between extension and nonextension into the appendiceal orifice. Ther Adv Gastroenterol 11:1756284818772794
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishihara S, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Boku N, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20:207–239
Oka S, Tanaka S, Kanao H, Ishikawa H, Watanabe T, Igarashi M, Saito Y, Ikematsu H, Kobayashi K, Inoue Y, Yahagi N, Tsuda S, Simizu S, Iishi H, Yamano H, Kudo SE, Tsuruta O, Tamura S, Saito Y, Cho E, Fujii T, Sano Y, Nakamura H, Sugihara K, Muto T (2010) Current status in the occurrence of postoperative bleeding, perforation and residual/local recurrence during colonoscopic treatment in Japan. Dig Endosc 22:376–380
Niikura R, Yasunaga H, Yamada A, Matsui H, Fushimi K, Hirata Y, Koike K (2016) Factors predicting adverse events associated with therapeutic colonoscopy for colorectal neoplasia: a retrospective nationwide study in Japan. Gastrointest Endosc 84:971.e6–982.e6
Kuwai T, Yamaguchi T, Imagawa H, Sumida Y, Takasago T, Miyasako Y, Nishimura T, Iio S, Yamaguchi A, Kouno H, Kohno H, Ishaq S (2017) Endoscopic submucosal dissection of early colorectal neoplasms with a monopolar scissor-type knife: short- to long-term outcomes. Endoscopy 49:913–918
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara K, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27:417–434
Tanaka S, Saitoh Y, Matsuda T, Igarashi M, Matsumoto T, Iwao Y, Suzuki Y, Nishida H, Watanabe T, Sugai T, Sugihara K, Tsuruta O, Hirata I, Hiwatashi N, Saito H, Watanabe M, Sugano K, Shimosegawa T (2015) Evidence-based clinical practice guidelines for management of colorectal polyps. J Gastroenterol 50:252–260
Hayashi N, Tanaka S, Nishiyama S, Terasaki M, Nakadoi K, Oka S, Yoshihara M, Chayama K (2014) Predictors of incomplete resection and perforation associated with endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc 79:427–435
Matsumoto A, Tanaka S, Oba S, Kanao H, Oka S, Yoshihara M, Chayama K (2010) Outcome of endoscopic submucosal dissection for colorectal tumors accompanied by fibrosis. Scand J Gastroenterol 45:1329–1337
Tajiri H, Kitano S (2004) Complications associated with endoscopic mucosal resection: definition of bleeding that can be viewed as accidental. Dig Endosc 16:S134–S136
Boda K, Oka S, Tanaka S, Nagata S, Kunihiro M, Kuwai T, Hiraga Y, Furudoi A, Terasaki M, Nakadoi K, Higashiyama M, Okanobu H, Akagi M, Chayama K (2018) Clinical outcome of endoscopic submucosal dissection for colorectal tumors: a large multicenter retrospective study from the Hiroshima GI Endoscopy Research Group. Gastrointest Endosc 87:714–722
Hotta K, Oyama T, Shinohara T, Miyata Y, Takahashi A, Kitamura Y, Tomori A (2010) Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc 22:302–306
Jeon HH, Lee HS, Youn YH, Park JJ, Park H (2016) Learning curve analysis of colorectal endoscopic submucosal dissection (ESD) for laterally spreading tumors by endoscopists experienced in gastric ESD. Surg Endosc 30:2422–2430
Yang DH, Jeong GH, Song Y, Park SH, Park SK, Kim JW, Jung KW, Kim KJ, Ye BD, Myung SJ, Yang SK, Kim JH, Park YS, Byeon JS (2015) The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci 60:3431–3441
Shiga H, Ohba R, Matsuhashi T, Jin M, Kuroha M, Endo K, Moroi R, Kayaba S, Iijima K (2017) Feasibility of colorectal endoscopic submucosal dissection (ESD) carried out by endoscopists with no or little experience in gastric ESD. Dig Endosc 29:58–65
Sakamoto T, Saito Y, Nakamura F, Abe S, Takamaru H, Sekiguchi M, Yamada M, Nakajima T, Matsuda T, Yamagishi H, Kato H (2018) Short-term outcomes following endoscopic submucosal dissection of large protruding colorectal neoplasms. Endoscopy 50:606–612
Niimi K, Fujishiro M, Goto O, Kodashima S, Koike K (2012) Safety and efficacy of colorectal endoscopic submucosal dissection by the trainee endoscopists. Dig Endosc 24:154–158
Sakamoto T, Saito Y, Fukunaga S, Nakajima T, Matsudas T (2011) Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum 54:1307–1312
Ohata K, Nonaka K, Misumi Y, Tsunashima H, Takita M, Minato Y, Tashima T, Sakai E, Muramoto T, Matsuyama Y, Hiejima Y, Matsuhashi N (2016) Usefulness of training using animal models for colorectal endoscopic submucosal dissection: is experience performing gastric ESD really needed? Endosc Int Open 4:E333–E339
Imai K, Hotta K, Yamaguchi Y, Kakushima N, Tanaka M, Takizawa K, Kawata N, Matsubayashi H, Shimoda T, Mori K, Ono H (2016) Preoperative indicators of failure of en bloc resection or perforation in colorectal endoscopic submucosal dissection: implications for lesion stratification by technical difficulties during stepwise training. Gastrointest Endosc 83:954–962
Takeuchi Y, Iishi H, Tanaka S, Saito Y, Ikematsu H, Kudo SE, Sano Y, Hisabe T, Yahagi N, Saitoh Y, Igarashi M, Kobayashi K, Yamano H, Shimizu S, Tsuruta O, Inoue Y, Watanabe T, Nakamura H, Fujii T, Uedo N, Shimokawa T, Ishikawa H, Sugihara K (2014) Factors associated with technical difficulties and adverse events of colorectal endoscopic submucosal dissection: retrospective exploratory factor analysis of a multicenter prospective cohort. Int J Colorectal Dis 29:1275–1284
Lee SP, Kim JH, Sung IK, Lee SY, Park HS, Shim CS, Han HS (2015) Effect of submucosal fibrosis on endoscopic submucosal dissection of colorectal tumors: pathologic review of 173 cases. J Gastroenterol Hepatol 30:872–878
Sakamoto H, Hayashi Y, Miura Y, Shinozaki S, Takahashi H, Fukuda H, Okada M, Ino Y, Takezawa T, Sunada K, Lefor AK, Yamamoto H (2017) Pocket-creation method facilitates endoscopic submucosal dissection of colorectal laterally spreading tumors, non-granular type. Endosc Int Open 5:E123–E129
Fu K, Sano Y, Kato S, Fujii T, Iwasaki J, Sugito M, Ono M, Saito N, Yoshida S, Fujimori T (2005) Hazards of endoscopic biopsy for flat adenoma before endoscopic mucosal resection. Dig Dis Sci 50:1324–1327
Fukunaga S, Nagami Y, Shiba M, Sakai T, Maruyama H, Ominami M, Otani K, Hosomi S, Tanaka F, Taira K, Tanigawa T, Yamagami H, Watanabe T, Fujiwara Y (2019) Impact of preoperative biopsy sampling on severe submucosal fibrosis on endoscopic submucosal dissection for colorectal laterally spreading tumors: a propensity score analysis. Gastrointest Endosc 89:470–478
Fock KM (2014) Review article: the epidemiology and prevention of gastric cancer. Aliment Pharmacol Ther 40:250–260
Iacopini F, Bella A, Costamagna G, Gotoda T, Saito Y, Elisei W, Grossi C, Rigato P, Scozzarro A (2012) Stepwise training in rectal and colonic endoscopic submucosal dissection with differentiated learning curves. Gastrointest Endosc 76:1188–1196
Pioche M, Rivory J, Nishizawa T, Uraoka T, Touzet S, O’Brien M, Saurin JC, Ponchon T, Denis A, Yahagi N (2016) Randomized comparative evaluation of endoscopic submucosal dissection self-learning software in France and Japan. Endoscopy 48:1076–1083
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Kazuki Boda, Shiro Oka, Shinji Tanaka, Shinji Nagata, Masaki Kunihiro, Toshio Kuwai, Yuko Hiraga, Akira Furudoi, Koichi Nakadoi, Hideharu Okanobu, Tomohiro Miwata, Shiro Okamoto, and Kazuaki Chayama have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boda, K., Oka, S., Tanaka, S. et al. Real-world learning curve analysis of colorectal endoscopic submucosal dissection: a large multicenter study. Surg Endosc 34, 3344–3351 (2020). https://doi.org/10.1007/s00464-019-07104-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07104-2