Abstract
Background
Hospital costs associated with the treatment of rectal cancer are considerable and the formation of a temporary stoma accounts for additional costs. Results from the EASY trial showed that early closure of a temporary ileostomy was associated with significantly fewer postoperative complications but no difference in health-related quality of life up to 12 months after rectal resection. The aim of the present study was to perform a cost analysis within the framework of the EASY trial.
Methods
Early closure (8–13 days) of a temporary stoma was compared to late closure (> 12 weeks) in the randomized controlled trial EASY (NCT01287637). The study period and follow-up was 12 months after rectal resection. Inclusion of participants was made after index surgery. Exclusion criteria were diabetes mellitus, steroid treatment, signs of postoperative complications or anastomotic leakage. Clinical effectiveness and resource use were derived from the trial and unit costs from Swedish sources. Costs were calculated for the year 2016 and analysed from the perspective of the healthcare sector.
Results
Fifty-five patients underwent early closure, and 57 late closure in eight Swedish and Danish hospitals between 2011 and 2014. The difference in mean cost per patient was 4060 US dollar (95% confidence interval 1121; 6999, p value < 0.01) in favour of early closure. A sensitivity analysis, taking protocol-driven examinations into account, resulted in an overall difference in mean cost per patient of $3608, in favour of early closure (95% confidence interval 668; 6549, p value 0.02). The predominant cost factors were reoperations, readmissions and endoscopic examinations.
Conclusions
The significant cost reduction in this study, together with results of safety and efficacy from the randomized controlled trial, supports the routine use of early closure of a temporary ileostomy after rectal resection for cancer in selected patients without signs of anastomotic leakage.
Clinical trial
Registered at clinicaltrials.gov, clinical trials identifier NCT01287637.
Similar content being viewed by others
Surgical treatment of potentially curable rectal cancer includes low anterior resection (LAR) with total mesorectal excision (TME) [1, 2]. Because of the proximity to the pelvic floor and based on previous results, the routine procedure involves the formation of a temporary defunctioning stoma in order to reduce the risk of symptomatic anastomotic leakage [3] and its clinical consequences [3,4,5,6]. The morbidity associated with a temporary defunctioning stoma is, however, considerable with complications such as dehydration and renal failure [4, 7,8,9] as well as parastomal hernia and skin irritation and ulceration [7]. Defunctioning stomas are usually reversed approximately three months after formation but it is not unusual that the stoma is left in place much longer and for some patients it becomes permanent [10].
Hospital costs associated with the treatment of rectal cancer are considerable, and the formation of a temporary stoma accounts for additional costs, including potential readmissions and a second operation (stoma closure) [11, 12]. Early closure of a temporary stoma has been associated with significantly fewer postoperative complications up to 12 months after rectal resection in a randomized controlled trial [13]. Although the routine use of a temporary stoma in patients operated with low anterior resection increases the hospital costs of surgical treatment for rectal cancer [12], early closure of such may be a cost-effective alternative [14].
The aim of the present study was to perform a cost analysis 12 months after rectal resection for cancer in a multicentre randomized trial comparing early vs. late closure of a temporary ileostomy (EASY trial) [15].
Materials and methods
EASY trial
The EASY trial was designed as a randomized multicentre controlled trial [15] comparing early with late closure of a temporary ileostomy after rectal resection. The primary endpoint was the mean number of complications after rectal resection and a secondary endpoint included health-related quality of life. Both results have been published previously [13, 16]. Inclusion of participants was made after rectal resection (TME for rectal cancer including the creation of a temporary ileostomy). Exclusion criteria were ongoing steroid treatment, diabetes mellitus, signs of postoperative complications and inability to understand Danish or Swedish. Patients with no adverse events were invited to participate. After informed consent, the patients underwent investigation with a contrast computed tomography scan (CT scan) and/or a flexible endoscopy of the rectum to confirm the integrity of the anastomosis. This was performed 6 to 8 days after index operation with stoma creation. Patients were then randomized to either the intervention group with early closure (8–13 days after stoma creation) or to the control group with late closure (> 12 weeks after stoma creation) of the temporary ileostomy. Eight Danish and Swedish hospitals participated in the trial during February 2011 to November 2015. Three centres (with a total number of 8 patients) were excluded due to failure of maintaining a screening log.
The present study comprised a secondary endpoint and aimed at comparing the costs between the two groups within 12 months after the rectal resection (stoma formation).
Health economic methodology
Consenting patients were followed up at stoma closure and at 3, 6 and 12 months after rectal resection regarding postoperative complications and health-related quality of life (primary and secondary endpoints). The resource use analysis was carried out at 12 months. All data were collected through case report forms (CRF). For the analysis, unit costs were derived from Swedish sources and applied for all patients. The analysis included costs accumulated during 12 months after stoma formation (rectal resection).
Resource use
For all surgical procedures, including rectal resection and stoma closure as well as reoperations, unit costs were derived from the Swedish Association of Local Authorities and Regions (SALAR, Sveriges kommuner och landsting, http://www.skl.se), which is based on approximately 85% of all inpatient procedures in Sweden. Readmissions without surgical interventions were calculated based on the actual days of hospital admission in a regular ward. Prior to analysis, since only one patient (control group) required admission to the intensive care unit (ICU), the decision was made not to include this in the cost calculation, as previously suggested [17]. Hence, there would be a risk of adding a rare and costly event that single-handedly could tip the results in one direction. Number of days with a temporary ileostomy (and for a few patients, permanent colostomy) was registered. Because of the fluctuation of stoma function, the resource items needed per day for stoma care were estimated in collaboration with a specialized stoma nurse for a typical functioning stoma.
Only outpatient radiological and endoscopic examinations were registered in the CRFs. Radiological examinations that served as 12 months oncological evaluation after rectal cancer surgery (as part of regular follow-up) were not included in the analysis, as these did not differ between the two groups. The CT scan and/or flexible endoscopy of the rectum that was performed prior to randomization was not included in the cost analysis, as this was a procedure solely for study inclusion and did not differ between the two groups.
All outpatient visits (outpatient clinic nurse, stoma nurse and surgeon) were registered and included in the cost analysis. The cost of chemotherapy was not included in the analysis as the distribution was equal between the two groups and was independent of timing of closure of the temporary ileostomy. Indirect costs such as sick leave were not included, as registry data were not available for the whole study population.
Unit costs
Surgical procedure codes (classified using the Nordic Medico-Statistical Committee ‘NOMESCO’ Classification of Surgical Procedures version 1.16) were retrieved from the national cost per patient database for the year 2016 from SALAR where every surgical procedure has a mean cost representing one hospital admission. These data were used for the calculation of all inpatient surgical procedures, including rectal resection, stoma closure and reoperations. Costs for outpatient procedures (surgical intervention and endoscopy) were derived from the outpatient Diagnosis Related Groups (DRG). Stoma material costs were obtained from pharmacy retail prices in Sweden. All costs were adjusted to the price year 2016 and converted from Swedish crowns (SEK) to United States dollar (USD) according to the purchasing power parities (PPP) for the gross domestic product (Organisation for Economic Co-operation and Development, http://www.oecd.org).
Trial registration
The protocol was registered at http://www.clinicaltrials.gov (NCT01287637) prior to patient inclusion.
Randomization
Consenting patients who fulfilled the inclusion criteria were randomized either to the intervention group with early closure (day 8–13 after stoma creation) or to the control group with late closure (> 12 weeks after stoma creation) of the ileostomy. Randomization was executed in computer-generated blocks of six. The randomization was performed in the surgical ward using sequentially numbered, thick, opaque and sealed envelopes. Blinding of the intervention was not possible.
Statistical analysis
The present study was part of a randomized controlled trial with power calculated for the primary endpoint (postoperative complications up to 12 months). The group size in EASY was set to 72 patients per group [13]. Since the health-related quality of life analysis was unable to detect a difference between the two groups [16], this variable was not included in the health economic analysis. As the intervention resulted in less morbidity [13], and is presumably less costly, the study was considered superior in terms of effectiveness and we did not plan for calculation of quality-adjusted life years (QALYs). Complete data were available for 106 patients (95%). In order to enable total cost calculation, missing values of specific cost components were imputed with the mean for the whole cohort. The six patients with missing data represented both the intervention and control group (n = 3 in each), and there were no differences in postoperative complications (one patients in each group had a grade IIIa complication according to Clavien–Dindo classification of complications). For the analysis and clinical outcomes of interest, descriptive statistics were used. Two-sample t test was used for the comparison of mean costs between the two groups. Due to skewed data and to assess robustness, a non-parametric bootstrap analysis was performed, as recommended [18]. P values smaller than 0.05 were considered statistically significant. A supporting analysis was performed, adjusting for sex, age, BMI, comorbidity and radiation in a regression model (in accordance with previous adjusted analysis for the primary endpoint). The software packages SPSS® 23 software (IBM, Armonk, New York, USA) SAS 9.4 (SAS Institute, Cary NC) and R 3.2.3 software [19] were used for statistical analysis.
Results
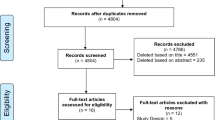
The EASY trial enrolled 112 patients between February 2011 and November 2014. The last follow-up was in November 2015. There were 55 patients in the early closure group (intervention) and 57 patients in the late closure group (control) (Fig. 1). One patient in each group died within 12 months after rectal resection and the costs for these patients were included in the analysis (Fig. 1). There were no violations of the randomization. Baseline demographic characteristics including comorbidity, cancer stage, chemo- and radiotherapy and body mass index (BMI) did not differ between the two groups, but there was a larger female population in the early closure group (Table 1). As reported previously [13], there were significantly fewer complications in the early closure group at 12 months after rectal resection. There was no difference in more severe complications (Clavien–Dindo grade IIIb and higher) (Table 1). The median time with a temporary ileostomy was 11 and 148 days in the early and late closure group, respectively. The total length of hospital stay for the rectal resection and the loop ileostomy closure (either as one or two admissions depending on treatment group) did not differ between the groups, but there were more readmissions in the late closure group (Table 1). The resource variables, unit costs and corresponding sources are listed in Table 2. Mean cost per patient and difference in resource use variables at 12 months are shown in Table 3. All resource use variables were more costly in the late closure group, except for ileostomy closure. This was due to the fact that more patients in the early closure group (25 patients compared to 22 patients in the late closure group) underwent a small bowel resection at closure (not requiring laparotomy), which resulted in a cost difference. The total difference in mean cost per patient was 4060 USD ($) in favour of early closure (95% confidence interval 1121; 6999, p value <0.01). A non-parametric bootstrap based on 2000 iterations showed similar results (Table 4). The adjusted analysis did not alter the results (Table 4). The predominant cost affecting factors were reoperations, readmissions and endoscopic examinations. The number of endoscopic examinations was in a sense protocol driven, to the extent that patients in the late closure group often undergo an additional endoscopic examination in order to confirm the integrity of the anastomosis, prior to stoma closure. A sensitivity analysis was therefore performed where the cost of an additional flexible sigmoidoscopy was added to early closure group and the patients in the late closure group that had not undergone any endoscopic examinations within 12 months after rectal resection. This analysis resulted in an overall difference in mean cost per patient of $3608, in favour of early closure (95% confidence interval 668; 6549, p value 0.02).
Study flow chart. *Excluded after clinical evaluation (n = 91), diabetes (n = 28), permanent or no stoma (n = 29), steroid treatment (n = 3), other (n = 8). **Centre 6 (n = 2), centre 7 (n = 3) and centre 8 (n = 3). †One patient died within 12 months (237 days). ††One patient died within 12 months (294 days). Figure has previously published in Danielsen et al. [12] and Park et al. [16]
Discussion
The results showed that early closure of a temporary ileostomy after rectal resection for cancer was less costly than late closure (standard care) in a randomized study setting. Early closure was associated with less use of outpatient resources (outpatient visits, procedures and diagnostic investigations) as well as fewer readmissions.
Readmission is a known factor affecting total direct healthcare costs [20] and previous studies have identified that the presence of a stoma has been associated with increased readmission rates within 30 to 90 days after colorectal surgery [20, 21]. One study reported an overall 90-day readmission rate of 23% [21]. In the present study, readmissions were twice as common in the late closure group (49%), compared to early closure (24%). This includes all readmissions within 12 months after rectal resection but excludes the readmission required for stoma closure.
A randomized trial of 234 patients found that the use of a defunctioning loop stoma reduced the rate of symptomatic anastomotic leakage after rectal resection for cancer [3]. A recently published five year analysis of the costs in the same study showed that the use of a defunctioning stoma was more expensive due to the need for a second operation (closure) and costs for stoma appliances, despite the cost savings associated with reduced frequency of symptomatic anastomotic leakage [12]. Since previous studies indicated benefits from the use of a defunctioning stoma [3, 5], the standard surgical treatment has included the formation of such. The EASY trial showed that early closure of a temporary ileostomy in selected patients without clinical or radiological signs of anastomotic leakage was associated with significantly fewer postoperative complications up to 12 months after rectal resection. Even though risk factors for anastomotic leakage after rectal resection for cancer are known, we still lack the tools to preoperatively identify which patients truly need a temporary stoma [22, 23]. The clinical postoperative evaluation and inclusion process used in the EASY trial, followed by early closure might therefore be a cost-effective and safe alternative, bearing in mind that early closure is only an option for patients without any signs of postoperative complications. In the trial, evaluation of the anastomosis was performed on postoperative day 6–8, and patients randomized to the intervention group underwent early closure 8–13 days after rectal resection. The total length of hospital stay (for rectal resection and loop ileostomy closure) did not differ between the groups. Patients in the trial may have had an overall longer hospital stay compared to patients undergoing rectal resection for cancer, outside the trial, due to the clinical evaluation and anastomotic investigation. However, given the potential risks of including patients with an anastomotic leak, this was considered necessary from a safety aspect. The present study revealed that the late closure group underwent more endoscopic examinations. This is probably partly due to the protocol, in the sense that several patients in the late closure group underwent an extra examination prior to closure of the stoma, since the previous examination would have been performed between three and eight months earlier. A sensitivity analysis was therefore performed in order to compensate for the extra flexible endoscopy of the rectum that would ‘burden’ the control group in this case. In this analysis, we could see that it had little effect on the overall expense, and the significant cost difference between the two groups remained. One patient in the trial required admission to the intensive care unit. This was a rare and costly event, and based on previous recommendations [17], it was not included in the cost analysis. Since this patient belonged to the late closure group, we may have consequently underestimated the true difference between the groups. However, this did not change the conclusion of the study.
The strength of the present study includes the study design (randomized controlled trial). The robust results with regard to clinical effectiveness, significant differences in resource use and costs, high rate of follow-up and few missing values together with performed sensitivity analyses suggest high internal validity. The inclusion of only direct costs (for example excluding sick leave) and the fact that the study was not powered for the present outcome are identified as limitations.
Conclusion
The significant cost reduction in this study, together with results of safety and efficacy from the randomized controlled trial, supports the routine use of early closure of a temporary ileostomy after rectal resection for cancer in selected patients without signs of anastomotic leakage.
References
O’Leary DP, Fide CJ, Foy C, Lucarotti ME (2001) Quality of life after low anterior resection with total mesorectal excision and temporary loop ileostomy for rectal carcinoma. Br J Surg 88(9):1216–1220
Heald RJ (1995) Total mesorectal excision is optimal surgery for rectal cancer: a Scandinavian consensus. Br J Surg 82(10):1297–1299
Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246(2):207–214
Ihnat P, Gunkova P, Peteja M, Vavra P, Pelikan A, Zonca P (2016) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30(11):4809–4816
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev 12(5):CD006878
Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J et al (2008) Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 248(1):52–60
Gessler B, Haglind E, Angenete E (2012) Loop ileostomies in colorectal cancer patients–morbidity and risk factors for nonreversal. J Surg Res 178(2):708–714
Hallbook O, Matthiessen P, Leinskold T, Nystrom PO, Sjodahl R (2002) Safety of the temporary loop ileostomy. Colorectal Dis 4(5):361–364
Gessler B, Haglind E, Angenete E (2014) A temporary loop ileostomy affects renal function. Int J Colorectal Dis 29(9):1131–1135
den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T et al (2007) A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol 8(4):297–303
Macafee DA, West J, Scholefield JH, Whynes DK (2009) Hospital costs of colorectal cancer care. Clin Med Oncol 3:27–37
Floodeen H, Hallbook O, Hagberg LA, Matthiessen P (2017) Costs and resource use following defunctioning stoma in low anterior resection for cancer - A long-term analysis of a randomized multicenter trial. Eur J Surg Oncol 43(2):330–336
Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A et al (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265(2):284–290
Robertson J, Linkhorn H, Vather R, Jaung R, Bissett IP (2015) Cost analysis of early versus delayed loop ileostomy closure: a case-matched study. Dig Surg 32(3):166–172
Danielsen AK, Correa-Marinez A, Angenete E, Skullmann S, Haglind E, Rosenberg J et al (2011) Early closure of temporary ileostomy–the EASY trial: protocol for a randomised controlled trial. BMJ Open 1(1):e000162
Park J, Danielsen AK, Angenete E, Bock D, Marinez AC, Haglind E et al (2018) Quality of life in a randomized trial of early closure of temporary ileostomy after rectal resection for cancer (EASY trial). Br J Surg 105(3):244–251
Bjoholt I, Janson M, Jonsson B, Haglind E (2006) Principles for the design of the economic evaluation of COLOR II: an international clinical trial in surgery comparing laparoscopic and open surgery in rectal cancer. Int J Technol Assess Health Care 22(1):130–135
Ramsey SD, Willke RJ, Glick H, Reed SD, Augustovski F, Jonsson B et al (2015) Cost-effectiveness analysis alongside clinical trials II-An ISPOR Good Research Practices Task Force report. Value Health 18(2):161–172
Team RC (2016) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Damle RN, Cherng NB, Flahive JM, Davids JS, Maykel JA, Sturrock PR et al (2014) Clinical and financial impact of hospital readmissions after colorectal resection: predictors, outcomes, and costs. Dis Colon Rectum 57(12):1421–1429
Wick EC, Shore AD, Hirose K, Ibrahim AM, Gearhart SL, Efron J et al (2011) Readmission rates and cost following colorectal surgery. Dis Colon Rectum 54(12):1475–1479
Klose J, Tarantino I, von Fournier A, Stowitzki MJ, Kulu Y, Bruckner T et al (2018) A nomogram to predict anastomotic leakage in open rectal surgery-hope or hype? J Gastrointest Surg 22:1619–1630
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary? Langenbecks Arch Surg 400(2):145–152
Acknowledgements
The authors express their gratitude to the doctors, nurses and staff at the participating centres.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jennifer Park has received funding from the Agreement concerning research and education of doctors ALFGBG-682731. Eva Angenete reports funding from the Swedish Research Council 2012-1786, the Swedish Cancer Society 2013/500, Sahlgrenska University Hospital, Agreement concerning research and education of doctors ALFGBG-366481, ALFGBG-526501 and ALFGBG-493341, the Swedish Society of Medicine SLS-247661 and SLS-412151 and the Lions Väst Cancer Foundation. Anne K Danielsen has received funding from the Research Council at Herlev and Gentofte Hospital, Denmark. Eva Haglind reports grants from the Swedish Research Council, Swedish Cancer Society, Sahlgrenska University Hospital, ALG grant, AFA Insurance Research grant outside the submitted work. David Bock, Adiela Correa-Marinez, Jacob Gehrman, Stefan Skullman, Jens E Jansen, Anette Wedin and Jacob Rosenberg have no conflicts of interest or financial ties to disclose.
Ethical approval
The study was approved by the Regional Ethical Approval Committee in Gothenburg, Sweden (Dnr 064-2011), and in Denmark by the Science Ethical Committee for the Capital Region in Denmark (H-1-2010-113).
Informed consent
All patients included in the study returned a signed consent form.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Park, J., Angenete, E., Bock, D. et al. Cost analysis in a randomized trial of early closure of a temporary ileostomy after rectal resection for cancer (EASY trial). Surg Endosc 34, 69–76 (2020). https://doi.org/10.1007/s00464-019-06732-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06732-y