Abstract
Background
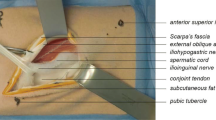
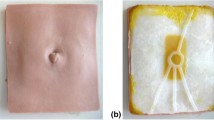
Paediatric laparoscopic procedures are now becoming routine practice. Therefore, there is a need for simulated laparoscopic models to acquire part-procedural competency prior to direct patient contact in a safe learning environment. For this reason, we chose two paediatric conditions; inguinal hernia (IH) and congenital diaphragmatic hernia (CDH), which were combined to create the laparoscopic inguinal and diaphragmatic defect (LIDD) model. Our aim was to assess this novel surgical simulation model by determining its construct and content validity.
Methods
A total of 107 participants completed the validation study: volunteer medical students (novices), surgical trainees (intermediate) and consultant surgeons (experts). Basic demographic data were collected. Subjects were shown a pre-recorded video of both exercises. The assessment exercise involved closing both the simulated inguinal or diaphragmatic hernial orifice. The task was assessed using a novel scoring system with a maximum score of 21 for IH model and 15 for the CDH. The content validity was assessed by a 6-point Likert scale of the expert group.
Results
105/107 participants successfully completed the two exercises. Both aspects of the LIDD model revealed a statistical significance between the scores obtained by the three groups of subjects. Experts scored 20.3/21 for the IH and 14.8/15 for the CDH models which significantly higher than medical students (6.3/21 and 5.3/15; p < 0.05 for both) and trainees (11.2/21 and 9.3/15; p < 0.05 for both). Similarly, trainees performed significantly better than medical students in both models (p < 0.05). Therefore, the LIDD model was found to have a good construct validity. It was, however, unable to differentiate between the various levels of trainees in the intermediate group. Content validity from the experts revealed that there was a high score for the potential of both aspects of LIDD (4.8 and 4.8). There was also a high level of functional fidelity for task completion (4.0 and 4.0).
Conclusions
We have demonstrated both the construct and content validity of the LIDD model for both laparoscopic IH and CDH repair. It was able to successfully differentiate between the expert, trainees and inexperienced laparoscopic surgeons.



Similar content being viewed by others
References
Gupta R, Singh S (2009) Challenges in paediatric laparoscopic surgeries. Indian J Anaesth 53(5):560–566
Stefanidis D, Sevdalis N, Paige J, Zevin B, Aggarwal R, Grantcharov T et al (2015) Simulation in surgery: what’s needed next? Ann Surg 261(5):846–853
Diesen DL, Erhunmwunsee L, Bennett KM, Ben-David K, Yurcisin B, Ceppa EP et al (2011) Effectiveness of laparoscopic computer simulator versus usage of box trainer for endoscopic surgery training of novices. J Surg Educ 68(4):282–289
Carlin AM, Gasevic E, Shepard AD (2007) Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg 193(3):326–330
Scott DJ (2006) Patient safety, competency, and the future of surgical simulation. Simul Healthc J Soc Simul Healthc 1(3):164–170
Schout BMA, Hendrikx AJM, Scheele F, Bemelmans BLH, Scherpbier AJJA (2010) Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc 24(3):536–546
Hennessey IAM, Hewett P (2013) Construct, concurrent, and content validity of the eoSim laparoscopic simulator. J Laparoendosc Adv Surg Tech 23(10):855–860
Zendejas B, Brydges R, Hamstra SJ, Cook DA (2013) State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg 257(4):586–593
Cho A, Basson S, Tsang T (2013) Outcomes of a structured training programme for paediatric laparoscopic inguinal hernia repair. J Pediatr Surg 48(2):404–407
Mokadam NA, Lee R, Vaporciyan AA, Walker JD, Cerfolio RJ, Hermsen JL et al (2015) Gamification in thoracic surgical education: using competition to fuel performance. J Thorac Cardiovasc Surg 150(5):1052–1058
Chummun K, Burke JP, O’Sullivan R, Prendiville W (2012) The influence of a ‘take home’ box trainer on laparoscopic performance for gynaecological surgeons. Gynecol Surg 9(3):303–308
Kobayashi SA, Jamshidi R, O’Sullivan P, Palmer B, Hirose S, Stewart L et al (2011) Bringing the skills laboratory home: an affordable webcam-based personal trainer for developing laparoscopic skills. J Surg Educ 68(2):105–109
Thinggaard E, Konge L, Bjerrum F, Strandbygaard J, Gögenur I, Spanager L (2017) Take-home training in a simulation-based laparoscopy course. Surg Endosc 31(4):1738–1745
Choy I, Kitto S, Adu-Aryee N, Okrainec A (2013) Barriers to the uptake of laparoscopic surgery in a lower-middle-income country. Surg Endosc 27(11):4009–4015
Singh P, Aggarwal R, Pucher PH, Hashimoto DA, Beyer-Berjot L, Bharathan R et al (2015) An immersive “simulation week” enhances clinical performance of incoming surgical interns improved performance persists at 6 months follow-up. Surgery 157(3):432–443
Stefanidis D, Arora S, Parrack DM, Hamad GG, Capella J, Grantcharov T et al (2012) Research priorities in surgical simulation for the 21st century. Am J Surg 203(1):49–53
Våpenstad C, Hofstad EF, Bø LE, Kuhry E, Johnsen G, Mårvik R et al (2017) Lack of transfer of skills after virtual reality simulator training with haptic feedback. Minim Invasive Ther Allied Technol 26(6):346–354
See KWM, Chui KH, Chan WH, Wong KC, Chan YC (2016) Evidence for endovascular simulation training: a systematic review. Eur J Vasc Endovasc Surg 51(3):441–451
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Damir Ljuhar, Samuel Alexander, Sarah Martin and Ramesh Nataraja have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ljuhar, D., Alexander, S., Martin, S. et al. The laparoscopic inguinal and diaphragmatic defect (LIDD) model: a validation study of a novel box trainer model. Surg Endosc 32, 4813–4819 (2018). https://doi.org/10.1007/s00464-018-6232-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6232-y