Abstract
Background
Since 2010, comparative studies on transanal and laparoscopic total mesorectal excision (TME) have been published and it remains unclear about the oncological benefit from transanal total mesorectal excision (taTME).
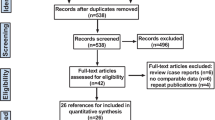
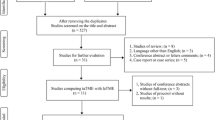
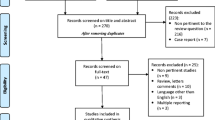
Methods
We have searched English databases to identify all taTME studies published between January 2010 and August 2017. Pathological outcomes included circumferential resection margin (CRM), positive CRM (< 1 M), length of distal resection margin (DRM), positive DRM, quality of mesorectum (complete mesorectum), harvested lymph node, and length of the specimen. Odds ratios (ORs) were calculated for dichotomous outcomes and weighted mean differences (WMDs) for continuous outcomes.
Results
We have included ten studies comprising of 762 patients. Compared with laparoscopic TME, taTME had a longer CRM (WMD, 0.833; 95% CI 0.366–1.299; P < 0.001), a lower positive rate of CRM (OR, 0.505; 95% CI 0.258–0.991; P = 0.047), and a longer DRM (WMD, 6.261; 95% CI 1.049–11.472; P = 0.019). There were no significant differences in other pathological outcomes. Both cumulative meta-analysis and sensitivity analysis were unable to detect potential sources of the heterogeneity in DRM. There was no evidence of publication bias.
Conclusions
This meta-analysis revealed that taTME had more advantages on positive CRM, CRM, and DRM compared with laparoscopic TME. Compared with laparoscopic TME, more benefits of taTME on pathological outcomes remained undetected. The current findings are all based on observational studies, RCTs with adequate power are required.








Similar content being viewed by others
References
Heald RJ, Husband EM, Ryall RDH (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Sylla P, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery. Surg Endosc 24:1205
Bulman AS, Lindley RP, Parsons P, Ellis H (1988) Pathological features of invasive breast cancer associated with a high risk of local recurrence after tumour excision and radical radiotherapy. Ann R Coll Surg Engl 70:289–292
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Higgins J, Green SE (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. Wiley, New York
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Wells GA, Shea BJ, O’Connell D, Peterson J, Welch V, Losos M et al (2005) The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Ottawa. Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327:557–560
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634
Velthuis S, Nieuwenhuis DH, Ruijter TE, Cuesta MA, Bonjer HJ, Sietses C (2014) Transanal versus traditional laparoscopic total mesorectal excision for rectal carcinoma. Surg Endosc 28:3494–3499
Rasulov AO, Mamedli ZZ, Gordeyev SS, Kozlov NA, Dzhumabaev HE (2016) Short-term outcomes after transanal and laparoscopic total mesorectal excision for rectal cancer. Tech Coloproctol 20:227–234
Perdawood SK, Thinggaard BS, Bjoern MX (2017) Effect of transanal total mesorectal excision for rectal cancer: comparison of short-term outcomes with laparoscopic and open surgeries. Surg Endosc. https://doi.org/10.1007/s00464-017-5926-x
Perdawood SK, Al Khefagie GA (2016) Transanal vs laparoscopic total mesorectal excision for rectal cancer: initial experience from Denmark. Colorectal Dis 18:51–58
Marks JH, Montenegro GA, Salem JF, Shields MV, Marks GJ (2016) Transanal TATA/TME: a case-matched study of taTME versus laparoscopic TME surgery for rectal cancer. Tech Coloproctol 20:467
Lelong B, Meillat H, Zemmour C, Poizat F, Ewald J, Mege D et al (2017) Short- and mid-term outcomes after endoscopic transanal or laparoscopic transabdominal total mesorectal excision for low rectal cancer: a single institutional case-control study. J Am Coll Surg 224:917–925
Fernandez-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, Diaz del Gobbo G et al (2015) Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg 261:221–227
de’Angelis N, Portigliotti L, Azoulay D, Brunetti F (2015) Transanal total mesorectal excision for rectal cancer: a single center experience and systematic review of the literature. Langenbecks Arch Surg 400:945–959
Chouillard EK, Chahine E, Quarisima S, Bonnet BV, Regnier A, Bors S (2016) Stanadardization of the approach to transanal notes total mesorectal excision (TME) in patients with rectal cancer: is anatomy better preserved? Surg Endosc 20:537–544
Chen CC, Lai YL, Jiang JK, Chu CH, Huang IP, Chen WS et al (2016) Transanal total mesorectal excision versus laparoscopic surgery for rectal cancer receiving neoadjuvant chemoradiation: a matched case-control study. Ann Surg Oncol 23:1169–1176
Zhang H, Zhang YS, Jin XW, Li MZ, Fan JS, Yang ZH (2013) Transanal single-port laparoscopic total mesorectal excision in the treatment of rectal cancer. Tech Coloproctol 17:117
Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, Lacy BD et al (2015) Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 221:415–423
Kneist W, Aigner F (2015) Total mesorectal excision via transanal minimally invasive surgery. An alternative technique. Coloproctology 37:253–261
Acknowledegement
Thanks to Prof. Choon Seng Chong, National University Hospital of Singapore, for his contribution in proofreading in English and other comments.
Funding
This work was supported by the National Natural Science Foundation of China (81572383).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Hong-Peng Jiang, Yan-Sen Li, Bo Wang, Fan Liu, Chang Wang, Zhan-Long Shen, Ying-Jiang Ye, and Shan Wang have no conflicts of interest or financial ties to disclose.
Additional information
Hong-Peng Jiang and Yan-Sen Li have equal first authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jiang, HP., Li, YS., Wang, B. et al. Pathological outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a systematic review with meta-analysis. Surg Endosc 32, 2632–2642 (2018). https://doi.org/10.1007/s00464-018-6103-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6103-6