Abstract
Background
Mastering right hemicolectomy techniques using laparoscopy in colorectal cancer surgery is very difficult. Although the long-term prognosis of laparoscopic right hemicolectomy (LRH) and complete mesocolic excision is unquestionable, different surgeons have their own opinions on routes of conducting LRH.
Objectives
LRH surgery is very complex due to the upper abdominal anatomical structure and vascular variation. Therefore, it has been considered the most difficult of all colorectal cancer surgeries. Our innovative middle cranial approach (MCA) was developed to avoid unnecessary injuries and minimize the operative time, thereby reducing the patient’s hospital stay and improving their short-term prognosis.
Methods
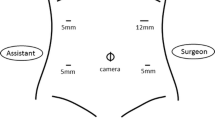
We compared 90 colon cancer patients who underwent the MCA between January 2016 and January 2017 with 82 patients who underwent the conventional central approach conducted by the same group of physicians (with Dr Cui as the surgeon) from 2011 to 2015. A short-term statistical analysis was performed.
Results
A total of 90 patients were included: 43 men and 47 women. Twenty-three patients underwent abdominal surgery (including stomach, rectum, and sigmoid colon surgery; appendectomy; and uterine attachment surgery). The median age of these patients was 62.6 (28–85) years; the median BMI was 22.9 (14.7–33.3) kg/m2; the mean bleeding volume was 53.9 (10–100) ml; the mean tumour diameter was 5.7 (0.8–9) cm, and the average number of lymph nodes detected was 19.2 (7–49).
Conclusions
Our study showed that radical resection of right-sided colon cancer using the MCA was safe and feasible for the treatment of colorectal cancer patients.



Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Heald RJ (1988) The ‘Holy Plane’ of rectal surgery. J R Soc Med 81(9):503–508
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation–technical notes and outcome. Colorectal Dis 11(4):354–364. https://doi.org/10.1111/j.1463-1318.2008.01735.x (discussion 364–355).
Sjovall A, Granath F, Cedermark B, Glimelius B, Holm T (2007) Loco-regional recurrence from colon cancer: a population-based study. Ann Surg Oncol 14(2):432–440. https://doi.org/10.1245/s10434-006-9243-1
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38(7):705–711
Hasegawa S, Kawamura J, Nagayama S, Nomura A, Kondo K, Sakai Y (2007) Medially approached radical lymph node dissection along the surgical trunk for advanced right-sided colon cancers. Surg Endosc 21(9):1657. https://doi.org/10.1007/s00464-007-9305-x
Ignjatovic D, Sund S, Stimec B, Bergamaschi R (2007) Vascular relationships in right colectomy for cancer: clinical implications. Tech coloproctol 11(3):247–250. https://doi.org/10.1007/s10151-007-0359-5
Jamieson JK, Dobson JF (1909) VII. Lymphatics of the colon: with special reference to the operative treatment of cancer of the colon. Ann Surg 50(6):1077–1090
Gillot C, Hureau J, Aaron C, Martini R, Thaler G, Michels NA (1964) The superior mesenteric vein, an anatomic and surgical study of eighty-one subjects. J Int Coll Surg 41:339–369
Baek SJ, Kim SH, Kwak JM, Kim J (2013) Incidence and risk factors of chylous ascites after colorectal cancer surgery. Am J Surg 206(4):555–559. https://doi.org/10.1016/j.amjsurg.2013.01.033
Alsabilah JF, Razvi SA, Albandar MH, Kim NK (2017) Intraoperative archive of right colonic vascular variability aids central vascular ligation and redefines gastrocolic trunk of henle variants. Dis Colon Rectum 60(1):22–29. https://doi.org/10.1097/dcr.0000000000000720
Culligan K, Walsh S, Dunne C, Walsh M, Ryan S, Quondamatteo F, Dockery P, Coffey JC (2014) The mesocolon: a histological and electron microscopic characterization of the mesenteric attachment of the colon prior to and after surgical mobilization. Ann Surg 260(6):1048–1056. https://doi.org/10.1097/sla.0000000000000323
Zhang C, Ding ZH, Yu HT, Yu J, Wang YN, Hu YF, Li GX (2011) Retrocolic spaces: anatomy of the surgical planes in laparoscopic right hemicolectomy for cancer. Am Surg 77(11):1546–1552
Treves F (1885) Lectures on the anatomy of the intestinal canal and peritoneum in man. Br Med J 1(1264):580–583
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30(15):1763–1769. https://doi.org/10.1200/jco.2011.38.3992
Galizia G, Lieto E, De Vita F, Ferraraccio F, Zamboli A, Mabilia A, Auricchio A, Castellano P, Napolitano V, Orditura M (2014) Is complete mesocolic excision with central vascular ligation safe and effective in the surgical treatment of right-sided colon cancers? A prospective study. Int J Colorectal Dis 29(1):89–97. https://doi.org/10.1007/s00384-013-1766-x
Storli KE, Sondenaa K, Furnes B, Eide GE (2013) Outcome after introduction of complete mesocolic excision for colon cancer is similar for open and laparoscopic surgical treatments. Dig Surg 30(4–6):317–327. https://doi.org/10.1159/000354580
Bertelsen CA, Bols B, Ingeholm P, Jansen JE, Neuenschwander AU, Vilandt J (2011) Can the quality of colonic surgery be improved by standardization of surgical technique with complete mesocolic excision? Colorectal Dis 13(10):1123–1129. https://doi.org/10.1111/j.1463-1318.2010.02474.x
Mike M, Kano N (2015) Laparoscopic surgery for colon cancer: a review of the fascial composition of the abdominal cavity. Surg Today 45(2):129–139. https://doi.org/10.1007/s00595-014-0857-9
Barussaud ML, Danion J, Castagnet M, Richer JP, Faure JP (2015) From anatomy to laparoscopic surgery, or how to reconcile surgeons to embryology. Surg Radiol Anat 37(4):393–398. https://doi.org/10.1007/s00276-014-1373-8
Matsuda T, Iwasaki T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2017) Laparoscopic complete mesocolic excision for right-sided colon cancer using a cranial approach: anatomical and embryological consideration. Int J Colorectal Disease 32(1):139–141. https://doi.org/10.1007/s00384-016-2673-8
Moore KL, Persaud TVN, Torchia MG Keith L, Moore, TVNPersaud, MG (2016) The developing human. clinically oriented embryology, 10th edn. Elsevier, Torchia
Benz S, Tam Y, Tannapfel A, Stricker I (2016) The uncinate process first approach: a novel technique for laparoscopic right hemicolectomy with complete mesocolic excision. Surg Endosc 30(5):1930–1937. https://doi.org/10.1007/s00464-015-4417-1
Matsuda T, Iwasaki T, Mitsutsuji M, Hirata K, Maekawa Y, Tsugawa D, Sugita Y, Sumi Y, Shimada E, Kakeji Y (2015) Cranially approached radical lymph node dissection around the middle colic vessels in laparoscopic colon cancer surgery. Langenbeck’s Arch Surg 400(1):113–117. https://doi.org/10.1007/s00423-014-1250-2
Kuzu MA, Ismail E, Celik S, Sahin MF, Guner MA, Hohenberger W, Acar HI (2017) Variations in the vascular anatomy of the right colon and implications for right-sided colon surgery. Dis Colon Rectum 60(3):290–298. https://doi.org/10.1097/dcr.0000000000000777
Adamina M, Manwaring ML, Park KJ, Delaney CP (2012) Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc 26(10):2976–2980. https://doi.org/10.1007/s00464-012-2294-4
Voiglio EJ, Boutillier du Retail C, Neidhardt JP, Caillot JL, Barale F, Mertens P (1998) Gastrocolic vein. Definition and report of two cases of avulsion. Surg Radiol Anat 20(3):197–201
Ignjatovic D, Spasojevic M, Stimec B (2010) Can the gastrocolic trunk of Henle serve as an anatomical landmark in laparoscopic right colectomy? A postmortem anatomical study. Am J Surg 199(2):249–254. https://doi.org/10.1016/j.amjsurg.2009.03.010
Acknowledgements
This work was supported by the Science & Technology Bureau (Grant Number 2015RAXYJ063) and the Science & Technology Bureau (Grant Number 2014RFQGJNSFC) and Hospital elite fund (Grant Number ZY2015-06) and Heilongjiang Scientific Research Program Assignmet Heilongjiang Medical Science Institute & Harbin Medical University Cancer Hospital (Regist No. 201705).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Songtao Du, Bomiao Zhang, Yanlong liu, Peng Han, Chengxin Song, Fangjie Hu, Tianyi Xia, Xiangxin Wu, Binbin Cui have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Du, S., Zhang, B., Liu, Y. et al. A novel and safe approach: middle cranial approach for laparoscopic right hemicolon cancer surgery with complete mesocolic excision. Surg Endosc 32, 2567–2574 (2018). https://doi.org/10.1007/s00464-017-5982-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5982-2