Abstract
Background
Postoperative pulmonary complications (PPCs) are the most common causes of serious morbidity after esophagectomy, which involves both thoracic and abdominal incisions. Although the thoracoscopic approach decreases PPC frequency after esophagectomy, it remains unclear whether the frequency is further decreased by combining it with laparoscopic gastric mobilization. This study aimed to determine the impact of laparoscopy on the prevention of PPCs after thoracoscopic esophagectomy using data from the Japan Clinical Oncology Group Study 0502 (JCOG0502).
Methods
JCOG0502 is a four-arm prospective study comparing esophagectomy with definitive chemo-radiotherapy. The use of thoracoscopy and/or laparoscopy was decided at the surgeon’s discretion. PPCs were defined as one or more of the following postoperative morbidities grade ≥2 (as per Common Terminology Criteria for Adverse Events v3.0): pneumonia, atelectasis, and acute respiratory distress syndrome.
Results
A total of 379 patients were enrolled in JCOG0502. Of these, 210 patients underwent esophagectomy via thoracotomy with laparotomy (n = 102), thoracotomy with laparoscopy (n = 7), thoracoscopy with laparotomy (n = 43), and thoracoscopy with laparoscopy (n = 58). PPC frequency was reduced to a greater extent by thoracoscopy than by thoracotomy (thoracoscopy 15.8%, thoracotomy 30.3%; p = 0.015). However, following thoracoscopic esophagectomy, laparoscopy failed to further decrease the PPC frequency compared with laparotomy (laparoscopy 15.5%, laparotomy 16.3%; p = 1.00). Univariable analysis showed that thoracoscopy (shown above) and less blood loss (<350 mL 16.3%, ≥350 mL 30.2%; p = 0.022) were associated with PPC prevention, whereas laparoscopy showed a borderline significant association (laparoscopy 15.4%, laparotomy 26.9%; p = 0.079). Multivariable analysis also showed that thoracoscopy and less blood loss were associated with PPC prevention.
Conclusion
Thoracoscopic approach to esophagectomy significantly reduced PPC frequency with minimal additional effect from laparoscopic gastric mobilization.
Similar content being viewed by others
Esophageal cancer is one of the most aggressive cancers affecting the gastrointestinal tract and is known to have a poor outcome. Approximately 482,300 new cases and 406,800 deaths from esophageal cancer occurred worldwide in 2008 [1]. In Japan, these numbers were 20,556 and 11,592, respectively [2].
Esophagectomy is the standard treatment for potentially resectable thoracic esophageal cancer [3]. It typically consists of transthoracic esophageal resection and transabdominal gastric mobilization for esophageal replacement. However, because it includes a wide surgical excision, esophagectomy is associated with a higher risk of postoperative morbidity and mortality than those in other cancer surgeries [4, 5]. Postoperative pulmonary complications (PPCs) are the most common causes of serious morbidity after esophagectomy and can result in a poor prognosis in esophagectomized patients [6,7,8]. Therefore, PPC prevention is crucial to improve the survival of patients with esophageal cancer.
Thoracoscopic esophagectomy was first introduced in 1992 [9] and has been extensively performed in recent years [10]. This approach minimizes the extent of chest trauma. Several studies, including those from our group, have reported that it decreases PPC frequency [11,12,13,14]. However, it remains unclear whether PPC frequency is further decreased by combining this thoracoscopic esophagectomy with laparoscopic gastric mobilization because previous prospective studies have only evaluated the combined impact of the two approaches [13, 14]. The present study uses data from our prospective multicenter trial, the Japan Clinical Oncology Group Study 0502 (JCOG0502), to determine the effect of laparoscopy on the prevention of PPCs after thoracoscopic esophagectomy and the factors playing a role in this prevention.
Materials and methods
Study design and patient selection
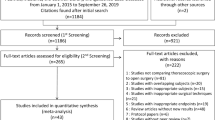
JCOG0502 is a four-arm prospective study comparing esophagectomy with definitive chemo-radiotherapy for T1bN0 cancers and includes randomized and patient preference arms. Patients were assigned for randomization if they had no strong preference and were then randomly allocated to one of the two treatments (Fig. 1). However, if patients had a strong preference and refused randomization, they were allocated to the arm with their preferred treatment. Written informed consent was obtained from all enrolled patients. The study protocol was approved by the Clinical Trial Review Committee of the JCOG and by the review boards of all the participating institutions. The trial was registered with UMIN-CTR (www.umin.ac.jp/ctr/) (registration number: UMIN000000551). Patient accrual for this study has been completed. The primary endpoint is overall survival in the randomized arm, which will be analyzed in 2018. The key eligibility criteria for JCOG0502 were as follows: age between 20 and 75 years, diagnosis of histologically proven clinical stage IA (T1bN0) squamous cell carcinoma, adenosquamous cell carcinoma, or basaloid cell carcinoma in the thoracic esophagus according to the American Joint Committee on Cancer Staging Manual (7th edition), and performance status 0–1 according to the Eastern Cooperative Oncology Group. The major exclusion criteria were as follows: double primary cancer, uncontrolled diabetes, recent myocardial infarction (≤3 months), unstable angina, chronic obstructive pulmonary disease, pulmonary fibrosis, and heart failure.
Operative methods
After the patients were allocated to the surgery arms, subtotal esophagectomy with lymphadenectomy was performed without preoperative chemotherapy and/or radiotherapy. The use of thoracoscopy and/or laparoscopy was decided at the surgeon’s discretion without any intention to compare these approaches, regardless of randomization or patient preference. Thoracoscopic esophagectomy was performed in the prone or lateral decubitus position according to the standards of each participating institution. In case of laparoscopic surgery, a minilaparotomy was made through which gastric conduits were created extracorporeally and specimens were removed. It could also be used as a hand-access port. Patients with upper thoracic disease underwent three-field lymphadenectomy, whereas those with mid- or lower thoracic disease underwent either two- or three-field lymphadenectomy at the surgeon’s discretion.
Definitions and statistical methods
PPCs were defined as one or more of the following postoperative morbidities grade ≥2 as per Common Terminology Criteria for Adverse Events (CTCAE) v3.0: pneumonia, atelectasis, and acute respiratory distress syndrome. Other postoperative complications were defined as adverse events of grade ≥2 as per CTCAE v3.0. Postoperative mortality was defined as postoperative death within 30 days due to any cause, or death during the same hospital admission. Preoperative laboratory data were divided into two categories based on the median values. To compare open and thoracoscopic/laparoscopic surgery groups, the Wilcoxon rank-sum test and Fisher’s exact test were used for continuous data and categorical data, respectively. Multivariable analysis included logistic regression without variable selection as well as stepwise variable selection (with α = 0.2 for including and/or retaining a variable in the model). Baseline characteristics, preoperative laboratory data, and operative factors were included as explanatory variables in the multivariable analyses. The level of significance was set at a two-sided p value of <0.05. All analyses were performed using SAS software, v9.2 (SAS Institute Inc., Cary, NC) at the JCOG Data Center. The data presented in this article include those up to June 2015.
Results
A total of 379 patients with clinical stage IA (T1bN0) thoracic esophageal cancer from 37 institutions were enrolled in JCOG0502 between December 2006 and February 2013. Excluding one patient who withdrew consent postoperatively, 210 of 379 patients underwent transthoracic esophagectomy (Fig. 1). These patients were enrolled from 30 institutions, and the median number of patients from each institution was 5 (range, 1–28). Gastric pull-up reconstruction was performed in the majority of patients (n = 206) with the colon being used as a conduit in the remaining patients (n = 4). Cervical anastomosis was performed in 198 patients, whereas intrathoracic anastomosis was performed in 12 patients. Of the 210 patients, 102 underwent thoracotomic esophagectomy with laparotomy, 7 underwent thoracotomy with laparoscopy, 43 underwent thoracoscopy with laparotomy, and 58 underwent thoracoscopy with laparoscopy (Fig. 1).
Impact of thoracoscopy on PPC prevention
First, we compared thoracotomy (n = 109) and thoracoscopy (n = 101) to confirm the effect of thoracoscopic approach on PPC prevention. As shown in Table 1, there were no significant differences in the baseline characteristics of patients between the two approaches. Operative data showed that the thoracoscopic approach reduced blood loss but prolonged the operating time. Postoperatively, patients undergoing thoracoscopy had a lower PPC frequency than those undergoing thoracotomy [thoracoscopy 16 (15.8%), thoracotomy 33 (30.3%); p = 0.015], particularly atelectasis [thoracoscopy 11 (10.9%), thoracotomy 24 (22.0%); p = 0.041] (Table 2). There were no significant differences in the incidences of other complications and postoperative stay duration between the two approaches.
Impact of laparoscopy on PPC prevention
Next, we determined whether PPC frequency was further decreased when combined with laparoscopy. Among the 101 patients who underwent thoracoscopic esophagectomy, 43 underwent laparotomy and 58 underwent laparoscopy (Fig. 1). As shown in Table 1, there were no significant differences in the baseline characteristics of the patients between the two approaches. Operative data showed that laparoscopy prolonged the operating time. Postoperatively, there were no significant differences in PPC frequency [laparoscopy 9 (15.5%), laparotomy 7 (16.3%); p = 1.00] and other postoperative complications/outcomes between the two approaches (Table 2).
Among the 109 patients who underwent thoracotomic esophagectomy, PPCs occurred in 32 patients (31.4%) in the laparotomy group and in 1 patient (14.3%) in the laparoscopy group. There was no significant difference between the two groups (p = 0.673).
Preventive factors for PPCs
Finally, we comprehensively analyzed the data from all 210 patients to determine if laparoscopy could aid in the prevention of PPCs. In univariable analysis, both thoracoscopy (shown above) and less blood loss (< 350 mL 16.3%, ≥350 mL 30.2%; p = 0.022) were associated with PPC prevention (Table 3), whereas laparoscopy showed a borderline significant reduction in PPC frequency (laparoscopy 15.4%, laparotomy 26.9%; p = 0.079). Multivariable analysis identified both thoracoscopy (Odds ratio, 0.40; 95% confidence interval, 0.16–1.04; p = 0.059) and preoperative partial pressure of O2 (PaO2) in arterial blood (Odds ratio, 0.50; 95% confidence interval, 0.24–1.02; p = 0.057) as preventive factors with borderline significance. Stepwise regression analysis showed that both thoracoscopy (Odds ratio, 0.46; 95% confidence interval, 0.23–0.92; p = 0.028) and less blood loss (Odds ratio, 0.50; 95% confidence interval, 0.25–0.99; p = 0.048) were associated with PPC prevention.
Discussion
The present study demonstrated that the laparoscopic approach had limited effect on PPC prevention after thoracoscopic esophagectomy. To the best of our knowledge, this is only the second study using data from a prospective multicenter trial that evaluated the effect of laparoscopy on PPC prevention after esophagectomy. The first phase III multicenter trial (MIRO trial) was conducted by Mariette et al. [15]. They reported that laparoscopy decreased PPC frequency to a greater extent than that by laparotomy under the condition of thoracotomy (laparoscopy 17.7%, laparotomy 30.1%; p = 0.037) [16]. This result is similar to that of the present study comparing laparoscopy with laparotomy following thoracotomic esophagectomy (laparoscopy 14.3%, laparotomy 31.4%), although the difference was not significant (p = 0.673) due to the lack of power. Therefore, our results are consistent with those of the MIRO trial, and laparoscopy is recommended to prevent PPCs under the condition of thoracotomy.
Another prospective randomized trial (TIME trial) reported that a combination of thoracoscopic and laparoscopic approaches decreased the frequency of pneumonia to a great extent compared with thoracotomy with laparotomy (thoracoscopy–laparoscopy: 9%, thoracotomy–laparotomy: 29%; p = 0.005) [13]. However, the extent to which each minimally invasive approach contributes to this reduction is still unclear. The present study demonstrated that laparoscopy showed a borderline significant reduction in PPC frequency, whereas thoracoscopy showed an independent and significant reduction in PPC frequency. Therefore, it is likely that the impact of thoracoscopy on the prevention of pneumonia in the TIME trial was more than that of laparoscopy.
It is well known that laparoscopic surgery maintains better postoperative respiratory function than open abdominal surgery [17, 18], thus potentially affecting PPC prevention after thoracoscopic esophagectomy. However, whether laparoscopy contributes to better postoperative respiratory function [19, 20] and reduction of PPC frequency [8, 19, 20] remains controversial. In the present study, laparoscopy failed to show any substantial effect on PPC prevention under this condition. We speculated that this is because the preventive effect of thoracoscopy was so dominant that it masked that of laparoscopy. Under the condition of thoracotomy, a laparoscopic approach could potentially have a substantial effect on PPC prevention.
Another possible explanation for laparoscopy failing to show a substantial preventive impact after thoracoscopic esophagectomy is the presence of a minilaparotomy. In the MIRO trial, surgeons created a gastric conduit intracorporeally using a pure laparoscopic approach without any minilaparotomy, and specimens were removed via the thoracotomic incision [15]. In contrast, gastric conduits in the laparoscopic group of the present study were created extracorporeally through a minilaparotomy, and specimens were removed via this incision. We speculate that the pain and discomfort caused by the minilaparotomy diminished the preventive effect of laparoscopy on PPCs. A laparoscopic approach without minilaparotomy may be required to further decrease PPC frequency after thoracoscopic esophagectomy.
The prone position with artificial pneumothorax is reported to have an advantage over the lateral decubitus position by avoiding total lung collapse, thereby decreasing the incidence of PPCs [21]. In the present study, the body positions were equally distributed between the laparotomy and laparoscopy groups as shown in Table 1. Therefore, it is not likely that the body position during thoracoscopic esophagectomy affected the results in the present study.
Multivariable analysis in the present study indicated that thoracoscopy and less blood loss were significant PPC preventive factors. It has previously been reported that less blood loss is associated with PPC prevention after esophagectomy [7, 22, 23]. Total blood loss during surgery is one of the parameters to estimate surgical stress in surgical risk scoring systems [24, 25], and the calculated risk score is well correlated with the postoperative morbidity and mortality rates after gastrointestinal surgery [26]. Therefore, it is likely that less blood loss is one of the PPC preventive factors after esophagectomy.
The median body mass index (BMI) in the present study (22.5) was lower than that in trials conducted in Western countries (24.0–25.0) [13, 16]. It has been reported that patients with a high BMI do not have increased risk of PPCs after esophagectomy compared with those with a normal BMI [27, 28]. Likewise, the present study showed no significant increase in PPC frequency in the BMI ≥25 group (Table 3). The pneumonia and PPC frequencies in the thoracotomy–laparotomy (control) group were reported to be 29 and 30.1% in the TIME and MIRO trials, respectively [13, 16], which are comparable with that of the present study (31.4%). Thus, it is not likely that the lower BMI affected the results in the present study.
The present study had some limitations. First, because it was designed as a non-randomized comparison with a limited number of patients, the results may have been affected by patient selection bias and low statistical power. Second, there are omitted preoperative patient variables of pulmonary function tests, smoking history, and comorbidities, which may influence PPC frequency. Third, esophagectomy was only performed for patients with stage IA esophageal cancers. Therefore, the results may not be generalized to advanced esophageal cancers, which require preoperative therapy and more invasive surgical manipulation. Finally, the results may have been influenced by different surgical techniques and perioperative patient care styles because they were carried out depending on the standards of each participating institution.
Our new randomized phase III trial, JCOG1409 (MONET trial), is currently underway to compare the efficacy and safety of thoracoscopic esophagectomy and thoracotomic esophagectomy. In the MONET trial, patients are further stratified based on whether they undergo laparotomy or laparoscopy for gastric mobilization, performed according to the standard of each participating institution [29]. We expect that the data from JCOG1409 will strengthen the conclusions of the present study.
In conclusion, the present study demonstrated that the thoracoscopic approach and less blood loss were significant factors in the prevention of PPCs after esophagectomy, whereas the laparoscopic approach had minimal effect on the prevention of PPCs after thoracoscopic esophagectomy.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Tachimori v, Ozawa S, Numasaki H, Fujishiro M, Matsubara H, Oyama T, Shinoda M, Toh Y, Udagawa H, Uno T, Registration Committee for Esophageal Cancer of the Japan Esophageal S (2015) Comprehensive registry of esophageal cancer in Japan, 2008. Esophagus 12:130–157
Kuwano H, Nishimura Y, Oyama T, Kato H, Kitagawa Y, Kusano M, Shimada H, Takiuchi H, Toh Y, Doki Y, Naomoto Y, Matsubara H, Miyazaki T, Muto M, Yanagisawa A (2015) Guidelines for diagnosis and Treatment of carcinoma of the esophagus, April 2012 edited by the Japan Esophageal Society. Esophagus 12:1–30
Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S, Sugihara K, Mori M, Satomi S, Kokudo N, Iwanaka T (2016) National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today 46:38–47
Yang CK, Teng A, Lee DY, Rose K (2015) Pulmonary complications after major abdominal surgery: National Surgical Quality Improvement Program analysis. J Surg Res 198:441–449
Kataoka K, Takeuchi H, Mizusawa J, Igaki H, Ozawa S, Abe T, Nakamura K, Kato K, Ando N, Kitagawa Y (2017) Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg 265:1152–1157
Baba Y, Yoshida N, Shigaki H, Iwatsuki M, Miyamoto Y, Sakamoto Y, Watanabe M, Baba H (2016) Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single institution study. Ann Surg 264:305–311
Ichikawa H, Miyata G, Miyazaki S, Onodera K, Kamei T, Hoshida T, Kikuchi H, Kanba R, Nakano T, Akaishi T, Satomi S (2013) Esophagectomy using a thoracoscopic approach with an open laparotomic or hand-assisted laparoscopic abdominal stage for esophageal cancer: analysis of survival and prognostic factors in 315 patients. Ann Surg 257:873–885
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37:7–11
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Sugihara K, Mori M (2014) A risk model for esophagectomy using data of 5354 Patients included in a Japanese Nationwide Web-Based Database. Ann Surg 260:259–266
Nozaki I, Kato K, Igaki H, Ito Y, Daiko H, Yano M, Udagawa H, Mizusawa J, Katayama H, Nakamura K, Kitagawa Y (2015) Evaluation of safety profile of thoracoscopic esophagectomy for T1bN0M0 cancer using data from JCOG0502: a prospective multicenter study. Surg Endosc 29:3519–3526
Nozaki I, Kato K, Igaki H, Ito Y, Daiko H, Yano M, Udagawa H, Mizusawa J, Katayama H, Nakamura K, Kitagawa Y (2015) Erratum to: evaluation of safety profile of thoracoscopic esophagectomy for T1bN0M0 cancer using data from JCOG0502: a prospective multicenter study. Surg Endosc 29:3527
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Luketich JD, Pennathur A, Franchetti Y, Catalano PJ, Swanson S, Sugarbaker DJ, De Hoyos A, Maddaus MA, Nguyen NT, Benson AB, Fernando HC (2015) Minimally invasive esophagectomy: results of a prospective phase II multicenter trial-the eastern cooperative oncology group (E2202) study. Ann Surg 261:702–707
Briez N, Piessen G, Bonnetain F, Brigand C, Carrere N, Collet D, Doddoli C, Flamein R, Mabrut JY, Meunier B, Msika S, Perniceni T, Peschaud F, Prudhomme M, Triboulet JP, Mariette C (2011) Open versus laparoscopically-assisted oesophagectomy for cancer: a multicentre randomised controlled phase III trial—the MIRO trial. BMC Cancer 11:310
Mariette C, Meunier B, Pezet D, Dalban C, Collet D, Thomas P, Brigand C, Perniceni T, Carrere N, Bonnetain F, Piessen G (2015) Hybrid minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicenter, open-label, randomized phase III controlled trial, the MIRO trial. J Clin Oncol 33, 2015 (suppl 3; abstr 5)
Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y (2002) A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery 131:S306–S311
Frazee RC, Roberts JW, Okeson GC, Symmonds RE, Snyder SK, Hendricks JC, Smith RW (1991) Open versus laparoscopic cholecystectomy. A comparison of postoperative pulmonary function. Ann Surg 213:651–653 (discussion 653–654)
Oshikiri T, Yasuda T, Kawasaki K, Harada H, Oyama M, Hasegawa H, Ohara T, Sendo H, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2016) Hand-assisted laparoscopic surgery (HALS) is associated with less-restrictive ventilatory impairment and less risk for pulmonary complication than open laparotomy in thoracoscopic esophagectomy. Surgery 159:459–466
Daiko H, Fujita T (2015) Laparoscopic assisted versus open gastric pull-up following thoracoscopic esophagectomy: a cohort study. Int J Surg 19:61–66
Markar SR, Wiggins T, Antonowicz S, Zacharakis E, Hanna GB (2015) Minimally invasive esophagectomy: lateral decubitus vs. prone positioning; systematic review and pooled analysis. Surg Oncol 24:212–219
Yoshida N, Watanabe M, Baba Y, Iwagami S, Ishimoto T, Iwatsuki M, Sakamoto Y, Miyamoto Y, Ozaki N, Baba H (2014) Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today 44:526–532
Nakamura M, Iwahashi M, Nakamori M, Ishida K, Naka T, Iida T, Katsuda M, Tsuji T, Nakatani Y, Yamaue H (2008) An analysis of the factors contributing to a reduction in the incidence of pulmonary complications following an esophagectomy for esophageal cancer. Langenbecks Arch Surg 393:127–133
Haga Y, Ikei S, Ogawa M (1999) Estimation of physiologic ability and Surgical Stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today 29:219–225
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Haga Y, Wada Y, Takeuchi H, Kimura O, Furuya T, Sameshima H, Ishikawa M (2004) Estimation of physiologic ability and surgical stress (E-PASS) for a surgical audit in elective digestive surgery. Surgery 135:586–594
Melis M, Meredith KL, Weber J, Siegel EM, McLoughlin JM, Dean EM, Shah N, Karl RC (2015) Body Mass Index and perioperative complications after esophagectomy for Cancer. Ann Surg. doi:10.1097/SLA.0000000000000242
Wightman SC, Posner MC, Patti MG, Ganai S, Watson S, Prachand V, Ferguson MK (2017) Extremes of body mass index and postoperative complications after esophagectomy. Dis Esophagus 30:1–6
Kataoka K, Takeuchi H, Mizusawa J, Ando M, Tsubosa Y, Koyanagi K, Daiko H, Matsuda S, Nakamura K, Kato K, Kitagawa Y, Japan Esophageal Oncology Group/Japan Clinical Oncology G (2016) A randomized phase III trial of thoracoscopic versus open esophagectomy for thoracic esophageal cancer: Japan Clinical Oncology Group Study JCOG1409. Jpn J Clin Oncol 46:174–177
Acknowledgements
We thank Dr. Hiroya Takeuchi who conceived the original idea for the present study and the members of the JCOG Data Center/JCOG Operations Office for their support in preparing the report, managing the data (Ms. Hiromi Katsuki), and overseeing the study (Dr. Haruhiko Fukuda).
Funding
This study was supported in part by the National Cancer Center Research and Development Fund (23-A-19, 23-A-16, 26-A-4, 29-A-3) from the Ministry of Health, Labour and Welfare of Japan. The JCOG0502 study was supported by Grants-in-Aid for Cancer Research (20S-3, 18-1) from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Isao Nozaki, Junki Mizusawa, Ken Kato, Hiroyasu Igaki, Yoshinori Ito, Hiroyuki Daiko, Masahiko Yano, Harushi Udagawa, Satoru Nakagawa, Masakazu Takagi, and Yuko Kitagawa have no conflicts of interest or financial ties to disclose.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nozaki, I., Mizusawa, J., Kato, K. et al. Impact of laparoscopy on the prevention of pulmonary complications after thoracoscopic esophagectomy using data from JCOG0502: a prospective multicenter study. Surg Endosc 32, 651–659 (2018). https://doi.org/10.1007/s00464-017-5716-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5716-5