Abstract
Introduction
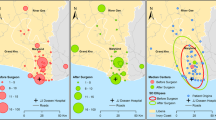
With the regionalization of surgical care, reduction in the rural workforce, rising healthcare costs, and increasing focus on surgical outcomes, appropriate transfer of surgical patients is an increasingly important aspect of health care. This study examines patients transferred for surgical intervention through a national sample.
Methods
The American College of Surgeons National Surgical Quality Improvement Program database was queried from 2005 to 2012 for surgery patients who were transferred from an outside hospital or emergency department (ED) and compared patients undergoing surgery without transfer. Patients were divided into two time periods (TP): 2005–2008 (TP1) and 2008–2012 (TP2) for analysis; patient characteristics and top CPT codes for each TP were collected. Univariate analysis and matched cohorts were used to compare the groups.
Results
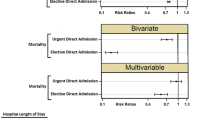
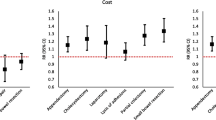
Overall, 61,204 patients were transferred and underwent surgery. The rate of transferred surgery patients increased from 3.2 % in TP1 to 4.5 % in TP2 (p < 0.0001). Compared to non-transferred patients, transferred patients had higher rates of diabetes (23.4 vs. 17.6 %, p < 0.0001), tobacco use (27.9 vs. 20.3 %, p < 0.0001), Charlson comorbidity index (mean score 1.5 vs. 0.8, p < 0.0001), preoperative sepsis (32.0 vs. 9.4 %, p < 0.0001), and need for emergent surgery (41.3 vs. 14.4 %, p < 0.0001). From TP1 to TP2, there was an increase in transferred patients who were obese (33.9–36.4 %, p < 0.0001) and had emergent transfers (39.6–41.8 %, p < 0.0001), with a decrease in diabetic patients (24.7–23.1 %, p < 0.0001). From TP1 to TP2, transferred patients had more minor complications (17.7–31.0 %, p < 0.0001), but fewer major complications (32.1–23.9 %, p < 0.0001) and lower 30-day mortality (11.8–8.1 %, p < 0.0001).
Conclusions
Patients transferred for surgery represent a higher acuity population than non-transferred patients, and the number of transfers continues to rise. Even when matched by comorbidities, transferred patients have worse outcomes. Surgical sub-specialization and physician tiering may complicate future transfer practices. Efficient transfers, effective physician communication, and ready availability of medical records are critical in improving patient transfers.
Similar content being viewed by others
References
Melgarejo Urendez A, Bernat Adell MD, Lorente Garcia P (2014) Analysis of adverse events associated with interhospital transfer of critically ill patients. Safety checklist. Enfermeria intensiva/Sociedad Espanola de Enfermeria Intensiva y Unidades Coronarias 25(2):58–64. doi:10.1016/j.enfi.2014.03.004
Arthur KR, Kelz RR, Mills AM, Reinke CE, Robertson MP, Sims CA, Pascual JL, Reilly PM, Holena DN (2013) Interhospital transfer: an independent risk factor for mortality in the surgical intensive care unit. Am Surg 79(9):909–913
Crippen CJ, Hughes SJ, Chen S, Behrns KE (2014) The impact of interhospital transfers on surgical quality metrics for academic medical centers. Am Surg 80(7):690–695
Golestanian E, Scruggs JE, Gangnon RE, Mak RP, Wood KE (2007) Effect of interhospital transfer on resource utilization and outcomes at a tertiary care referral center. Crit Care Med 35(6):1470–1476. doi:10.1097/01.ccm.0000265741.16192.d9
Gordon HS, Rosenthal GE (1996) Impact of interhospital transfers on outcomes in an academic medical center. Implications for profiling hospital quality. Med Care 34(4):295–309
Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA (2003) Accepting critically ill transfer patients: adverse effect on a referral center’s outcome and benchmark measures. Ann Intern Med 138(11):882–890
Combes A, Luyt CE, Trouillet JL, Chastre J, Gibert C (2005) Adverse effect on a referral intensive care unit’s performance of accepting patients transferred from another intensive care unit. Crit Care Med 33(4):705–710
Hernandez-Boussard T, Davies S, McDonald K, Wang NE (2014) Interhospital facility transfers in the United States: a nationwide outcomes study. J Patient Saf. doi:10.1097/pts.0000000000000148
Lucas DJ, Ejaz A, Haut ER, Spolverato G, Haider AH, Pawlik TM (2014) Interhospital transfer and adverse outcomes after general surgery: implications for pay for performance. J Am Coll Surg 218(3):393–400. doi:10.1016/j.jamcollsurg.2013.11.024
BlueCross BlueShield of North Carolina Tiered Network Product (2015). https://www.bcbsnc.com/content/providers/quality-based-networks/tiered-network.htm. Accessed Jan 2015
Unicare (2012) Physician Tiering FAQ. https://www.unicarestateplan.com/pdf/physicianTieringFAQ.pdf. Nov 2014
Wadgaonkar AD, Schneider EC, Bhattacharyya T (2010) Physician tiering by health plans in Massachusetts. J Bone Joint Surg Am 92(12):2204–2209. doi:10.2106/jbjs.i.01080
Hong CS, Atlas SJ, Chang Y, Subramanian SV, Ashburner JM, Barry MJ, Grant RW (2010) Relationship between patient panel characteristics and primary care physician clinical performance rankings. JAMA 304(10):1107–1113. doi:10.1001/jama.2010.1287
Services TCfMaM (2014) Roadmap for implementing value driven healthcare in the traditional medicare fee-for-service program. Department of Health and Human Services, Washington, DC
The Board of Trustees FHIaFSMITF (2012) Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. Centers for Medicare and Medicaid Services
Schneider EL, Guralnik JM (1990) The aging of America. Impact on health care costs. Jama 263(17):2335–2340
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
D’Hoore W, Bouckaert A, Tilquin C (1996) Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol 49(12):1429–1433
Bergman S, Martelli V, Monette M, Sourial N, Deban M, Hamadani F, Teasdale D, Holcroft C, Zakrzewski H, Fraser S (2013) Identification of quality of care deficiencies in elderly surgical patients by measuring adherence to process-based quality indicators. J Am Coll Surg 217(5):858–866. doi:10.1016/j.jamcollsurg.2013.07.387
Ehlert BA, Durham CA, Parker FM, Bogey WM, Powell CS, Stoner MC (2011) Impact of operative indication and surgical complexity on outcomes after thoracic endovascular aortic repair at National Surgical Quality Improvement Program Centers. J Vasc Surg 54(6):1629–1636. doi:10.1016/j.jvs.2011.05.116
Ross SW, Oommen B, Kim M, Walters AL, Green JM, Heniford BT, Augenstein VA (2014) A little slower, but just as good: postgraduate year resident versus attending outcomes in laparoscopic ventral hernia repair. Surg Endosc 28(11):3092–3100. doi:10.1007/s00464-014-3586-7
Menchine MD, Baraff LJ (2008) On-call specialists and higher level of care transfers in California emergency departments. Acad Emerg Med 15(4):329–336. doi:10.1111/j.1553-2712.2008.00071.x
Spain DA, Bellino M, Kopelman A, Chang J, Park J, Gregg DL, Brundage SI (2007) Requests for 692 transfers to an academic level I trauma center: implications of the emergency medical treatment and active labor act. J Trauma 62(1):63–67. doi:10.1097/TA.0b013e31802d9716 (discussion 67–68)
Lynge DC, Larson EH, Thompson MJ, Rosenblatt RA, Hart LG (2008) A longitudinal analysis of the general surgery workforce in the United States, 1981–2005. Arch Surg (Chicago, Ill: 1960) 143(4):345–350. doi:10.1001/archsurg.143.4.345 (discussion 351)
Rossi A, Rossi D, Rossi M, Rossi P (2011) Continuity of care in a rural critical access hospital: surgeons as primary care providers. Am J Surg 201(3):359–362. doi:10.1016/j.amjsurg.2010.08.026 (discussion 362)
Iwashyna TJ (2012) The incomplete infrastructure for interhospital patient transfer. Crit Care Med 40(8):2470–2478. doi:10.1097/CCM.0b013e318254516f
Bosk EA, Veinot T, Iwashyna TJ (2011) Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care 49(6):592–598. doi:10.1097/MLR.0b013e31820fb71b
Iwashyna TJ, Courey AJ (2011) Guided transfer of critically ill patients: where patients are transferred can be an informed choice. Curr Opin in Crit Care 17(6):641–647. doi:10.1097/MCC.0b013e32834b3e55
Nacht J, Macht M, Ginde AA (2013) Interhospital transfers from U.S. emergency departments: implications for resource utilization, patient safety, and regionalization. Acad Emerg Med 20(9):888–893. doi:10.1111/acem.12209
Santry HP, Janjua S, Chang Y, Petrovick L, Velmahos GC (2011) Interhospital transfers of acute care surgery patients: Should care for nontraumatic surgical emergencies be regionalized? World J Surg 35(12):2660–2667. doi:10.1007/s00268-011-1292-3
Gupta R, Greer SE, Martin ED (2010) Inefficiencies in a rural trauma system: the burden of repeat imaging in interfacility transfers. J Trauma 69(2):253–255. doi:10.1097/TA.0b013e3181e4d579
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, group D-Es (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 35(6):1477–1483. doi:10.1097/01.ccm.0000266585.74905.5a
Holena DN, Mills AM, Carr BG, Wirtalla C, Sarani B, Kim PK, Braslow BM, Kelz RR (2011) Transfer status: a risk factor for mortality in patients with necrotizing fasciitis. Surgery 150(3):363–370. doi:10.1016/j.surg.2011.06.005
Singh JM, MacDonald RD, Bronskill SE, Schull MJ (2009) Incidence and predictors of critical events during urgent air-medical transport. CMAJ Can Med Assoc J 181(9):579–584. doi:10.1503/cmaj.080886
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B, American College of C, American Heart Association Task Force on Practice G, American College of Emergency P, Society for Cardiovascular A, Interventions, Society of Thoracic S, American Association of C, Pulmonary R, Society for Academic Emergency M (2007) ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 50(7):e1–e157. doi:10.1016/j.jacc.2007.02.013
Nathens AB, Maier RV, Brundage SI, Jurkovich GJ, Grossman DC (2003) The effect of interfacility transfer on outcome in an urban trauma system. J Trauma 55(3):444–449. doi:10.1097/01.ta.0000047809.64699.59
Libassi P (2013) A new front door. Expanding the hospital’s reach with freestanding EDs. Health Facil Manag 26(6):28–33
Rylko-Bauer B (1988) The development and use of freestanding emergency centers: a review of the literature. Med Care Rev 45(1):129–163
Simon EL, Griffin P, Medepalli K, Griffin G, Williams CJ, Hewit M, Lloyd TS (2014) Door-to-balloon times from freestanding emergency departments meet ST-segment elevation myocardial infarction reperfusion guidelines. J Emerg Med 46(5):734–740. doi:10.1016/j.jemermed.2013.08.089
User Guide for the Participate Use of Data File—American College of Surgeons National Quality Improvement Program (2007). http://www.acsnsqip.org Accessed Nov 2014
Disclosures
Drs. Huntington, Cox, Blair, Lincourt, Matthews, Augenstein, Heniford, and Ms. Prasad have no personal or financial conflicts of interest to disclose relevant to this manuscript or its data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huntington, C.R., Cox, T.C., Blair, L.J. et al. Acuity, outcomes, and trends in the transfer of surgical patients: a national study. Surg Endosc 30, 1301–1309 (2016). https://doi.org/10.1007/s00464-015-4361-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4361-0