Abstract
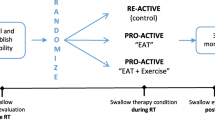
Research advocates for the use of intensive, prophylactic swallowing therapy to help reduce the severity of dysphagia in patients receiving (chemo)radiotherapy ([C]RT) for head/neck cancer (HNC). Unfortunately, the intensity of this therapy, coupled with growing patient numbers and limited clinical resources, provides challenges to many international cancer facilities. Telepractice has been proposed as a potential method to provide patients with greater support in home-practice, whilst minimising burden to the health service. This study investigated the clinical and patient-attributable costs of delivering an intensive, prophylactic swallowing therapy protocol via a new telepractice application “SwallowIT” as compared to clinician-directed FTF therapy and independent patient self-directed therapy. Patients (n = 79) with oropharyngeal HNC receiving definitive (C)RT were randomised to receive therapy via a: clinician-directed (n = 26), patient-directed (n = 27), or SwallowIT-assisted (n = 26) model of care. Data pertaining to health service costs (service time, consumables, therapy resources), patient-attributable costs (travel and wages) and patient-reported health-related quality of life (QoL) (AQoL-6D) were collected. SwallowIT provided a cost-efficient model of care when compared to the clinician-directed model, with significant cost savings to both the health service and to HNC consumers (total saving of $1901.10 AUD per patient; p < 0.001). The SwallowIT model also proved more cost-effective than the patient-directed model, yielding clinically significantly superior QoL at the end of (C)RT, for comparable costs. Overall, when compared to the alternate methods of service-delivery, SwallowIT provided a financially viable and cost-effective method for the delivery of intensive, prophylactic swallowing therapy to patients with HNC during (C)RT.


Similar content being viewed by others
References
De Souza JA, Santana IA, De Castro G, de Lima Lopes G, Shih Y-CT. Economic analyses in squamous cell carcinoma of the head and neck: a review of the literature from a clinical perspective. Int J Radiat Oncol Biol Phys. 2014;89(5):989–96.
Lee JM, Turini M, Botteman MF, Stephens JM, Pashos CL. Economic burden of head and neck cancer. Eur J Health Econ. 2004;5(1):70–80.
Wissinger E, Griebsch I, Lungershausen J, Foster T, Pashos CL. The economic burden of head and neck cancer: a systematic literature review. Pharmacoeconomics. 2014;32(9):865–82.
Amonkar MM, Chastek B, Samant N, Teitelbaum A. Economic burden of resected squamous cell carcinoma of the head and neck in a US managed-care population. J Med Econ. 2011;14(4):421–32.
Kim K, Amonkar MM, Högberg D, Kasteng F. Economic burden of resected squamous cell carcinoma of the head and neck in an incident cohort of patients in the UK. Head Neck Oncol. 2011;3(1):1.
Wild CP, Stewart BW, editors. World cancer report 2014. World Health Organization; 2014.
Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and-unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26(4):612–9.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–301.
Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–81.
Porter ME. A strategy for health care reform: toward a value-based system. N Engl J Med. 2009;361(2):109–12.
Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060–5.
Roman BR, Awad MI, Patel SG. Defining value-driven care in head and neck oncology. Curr Oncol Rep. 2015;17(1):424.
Carnaby-Mann G, Crary MA, Schmanlfuss I, Amdur R. “Pharyngocise”: randomized controlled trial of preventative exercises to maintain muscle structure and swallowing function during head-and-neck chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2011;83(1):210–9. https://doi.org/10.1016/j.ijrobp.2011.06.1954.
Duarte VM, Chhetri DK, Liu YF, Erman AA, Wang MB. Swallow preservation exercises during chemoradiation therapy maintains swallow function. Otolaryngol Head Neck Surg. 2013;149(6):878–84.
Hutcheson K, Bhayani MK, Beadle BM, Gold KA, Shinn E, Lai SY, Lewin J. Eat and exercise during radiotherapy or chemoradiotherapy for pharyngeal cancers: use it or lose it. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1127–34.
Ohba S, Yokoyama J, Kojima M, Fujimaki M, Anzai T, Komatsu H, Ikeda K. Significant preservation of swallowing function in chemoradiotherapy for advanced head and neck cancer by prophylactic swallowing exercise. Head Neck. 2016;38(4):517–21.
Peng KA, Kuan EC, Unger L, Lorentz WC, Wang MB, Long JL. A swallow preservation protocol improves function for veterans receiving chemoradiation for head and neck cancer. Otolaryngol Head Neck Surg. 2015;152(5):863–7.
van der Molen L, van Rossman M, Burkhead L, Smeele L, Rasch C, Hilgers F. A randomised preventive rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance and short-term effects. Dysphagia. 2011;26(2):155–70. https://doi.org/10.1007/s00455-010-9288-y.
Virani A, Kunduk M, Fink DS, McWhorter AJ. Effects of 2 different swallowing exercise regimens during organ-preservation therapies for head and neck cancers on swallowing function. Head Neck. 2015;37(2):162–70.
Retèl VP, van der Molen L, Hilgers FJ, Rasch CR, l’Ortye AA, Steuten LM, van Harten WH. A cost-effectiveness analysis of a preventive exercise program for patients with advanced head and neck cancer treated with concomitant chemo-radiotherapy. BMC Cancer. 2011;11(1):1.
Krisciunas GP, Sokoloff W, Stepas K, Langmore SE. Survey of usual practice: dysphagia therapy in head and neck cancer patients. Dysphagia. 2012;27(4):538–49.
Lawson N, Krisciunas GP, Langmore SE, Castellano K, Sokoloff W, Hayatbakhsh R. Comparing dysphagia therapy in head and neck cancer patients in Australia with international healthcare systems. Int J Speech Lang Pathol. 2017;19:128–38.
Roe JW, Carding PN, Rhys-Evans PH, Newbold KL, Harrington KJ, Nutting CM. Assessment and management of dysphagia in patients with head and neck cancer who receive radiotherapy in the United Kingdom: a web-based survey. Oral Oncol. 2012;48(4):343–8.
Hegney D, Pearce S, Rogers-Clark C, Martin-McDonald K, Buikstra E. Close, but still too far. The experience of Australian people with cancer commuting from a regional to a capital city for radiotherapy treatment. Eur J Cancer Care. 2005;14(1):75–82.
Martin-McDonald K, Rogers-Clark C, Hegney D, McCarthy A, Pearce S. Experiences of regional and rural people with cancer being treated with radiotherapy in a metropolitan centre. Int J Nurs Pract. 2003;9(3):176–82.
Beswick DM, Vashi A, Song Y, Pham R, Holsinger FC, Rayl JD, Walker B, Chardos J, Yuan A, Benadam-Lenrow E. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a Veterans Health Administration population. Head Neck. 2016;38(6):925–9.
Burns C, Ward EC, Hill AJ, Malcolm K, Bassett L, Kenny LM, Greenup P. A pilot trial of a speech pathology telehealth service for head and neck cancer patients. J Telemed Telecare. 2012;18(8):443–6.
Burns CL, Kularatna S, Ward EC, Hill AJ, Byrnes J, Kenny LM. Cost analysis of a speech pathology synchronous telepractice service for patients with head and neck cancer. Head Neck. 2017;39(12):2470–80. https://doi.org/10.1002/hed.24916.
Coyle JL. Tele-dysphagia management: an opportunity for prevention, cost-savings and advanced training. Int J Telerehabilit. 2012;4:(1).
Head BA, Keeney C, Studts JL, Khayat M, Bumpous J, Pfeifer M. Feasibility and acceptance of a telehealth intervention to promote symptom management during treatment for head and neck cancer. J Support Oncoloy. 2011;9(1):e1.
Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: an acceptable telehealth model for rural patients and health workers. Intern Med J. 2012;42(7):780–5.
Wall LR, Cartmill B, Ward EC, Hill AJ, Isenring E, Byrnes J, Chambers S, Dunn J, Nixon J, Whelan J. “ScreenIT”: computerized screening of swallowing, nutrition and distress in head and neck cancer patients during (chemo) radiotherapy. Oral Oncol. 2016;54(3):47–53. https://doi.org/10.1016/j.oraloncology.2016.01.004.
Ward E, Crombie J, Trickey M, Hill A, Theodoros D, Russell T. Assessment of communication and swallowing post-laryngectomy: a telerehabilitation trial. J Telemed Telecare. 2009;15(5):232–7.
Deshpande A, Khoja S, Lorca J, McKibbon A, Rizo C, Husereau D, Jadad AR. Asynchronous telehealth: a scoping review of analytic studies. Open Med. 2009;3(2):69–91.
Cherney LR, Kaye RC, Hitch RS. The best of both worlds: combining synchronous and asynchronous telepractice in the treatment of aphasia. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2011;21(3):83–93.
Mortley J, Wade J, Davies A, Enderby P. An investigation into the feasibility of remotely monitored computer therapy for people with aphasia. Adv Speech Lang Pathol. 2003;5(1):27–36.
Wade J, Mortley J, Enderby P. Talk about IT: views of people with aphasia and their partners on receiving remotely monitored computer-based word finding therapy. Aphasiology. 2003;17(11):1031–56.
Dávalos ME, French MT, Burdick AE, Simmons SC. Economic evaluation of telemedicine: review of the literature and research guidelines for benefit–cost analysis. Telemed e-Health. 2009;15(10):933–48.
Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Examining user perceptions of SwallowIT: a pilot study of a new telepractice application for delivering intensive swallowing therapy to head and neck cancer patients. J Telemed Telecare. 2017;23(1):53–9. https://doi.org/10.1177/1357633x15617887.
Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:332–42.
Richardson J, Atherton Day N, Peacock S, Iezzi A. Measurement of the quality of life for economic evaluation and the Assessment of Quality of Life (AQoL) Mark 2 instrument. Aust Econ Rev. 2004;37(1):62–88.
Bensadoun R-J, Riesenbeck D, Lockhart PB, Elting LS, Spijkervet FK, Brennan MT. A systematic review of trismus induced by cancer therapies in head and neck cancer patients. Support Care Cancer. 2010;18(8):1033–8.
Kraaijenga S, van der Molen L, van den Brekel M, Hilgers F. Current assessment and treatment strategies of dysphagia in head and neck cancer patients: a systematic review of the 2012/13 literature. Curr Opin Support Palliat Care. 2014;8(2):152–63.
Retèl VP, van der Molen L, Steuten LM, van den Brekel MW, Hilgers FJ. A cost-effectiveness analysis of using TheraBite in a preventive exercise program for patients with advanced head and neck cancer treated with concomitant chemo-radiotherapy. Eur Arch Otorhinolaryngol. 2016;273(3):709–18.
Hawthorne G, Osborne R. Population norms and meaningful differences for the Assessment of Quality of Life (AQoL) measure. Aust N Z J Public Health. 2005;29(2):136–42.
Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes. 2003;1(1):1.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Adherence to a prophylactic swallowing therapy program during (chemo) radiotherapy: impact of service-delivery model and patient factors. Dysphagia. 2017;32(2):279–92. https://doi.org/10.1007/s00455-016-9757-z.
Badr H, Gupta V, Sikora A, Posner M. Psychological distress in patients and caregivers over the course of radiotherapy for head and neck cancer. Oral Oncol. 2014;50(10):1005–11.
Murphy B, Gilbert J. Dysphagia in head and neck cancer patients treated with radiation: assessment, sequelae, and rehabilitation. Semin Radiat Oncol. 2009;19(1):35–42. https://doi.org/10.1016/j.semradonc.2008.09.007.
American Cancer Society (2016) Oral cavity and pharynx. https://cancerstatisticscenter.cancer.org/?_ga=1.248200067.529372574.1470011905#/cancer-site/Oral%20cavity%20and%20pharynx. Accessed Aug 2016.
Australian Institute of Health and Welfare (2016) Australian Cancer Incidence and Mortality (ACIM) books: head and neck including lip cancer. AIHW. https://head-neck-cancer.canceraustralia.gov.au/statistics#proj. Accessed Aug 2016.
Cancer Research UK (2016) Oral cancer incidence statistics. Cancer Research UK. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/oral-cancer. Accessed Aug 2016.
Acknowledgements
The authors would like to acknowledge the Princess Alexandra Hospital Study, Education and Research Trust Account (SERTA) and Princess Alexandra Hospital Research Foundation for providing funding to conduct this research. The authors disclose that ATOS Medical (Hörby, Sweden) supplied the Therabite™ ActivBands and subsidised the costs of the Therabite™ devices used in this study. We acknowledge Alison Phelan, Alana Hutchison and the clinical teams at the Metro South Radiation Oncology Service (Brisbane, Australia) for their assistance with data collection, and we thank the participants for their time.
Funding
This study was funded by PA Research Foundation (Grant No. Project Grant), PA Hospital SERTA (Grant No. Small Grant).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wall, L.R., Kularatna, S., Ward, E.C. et al. Economic Analysis of a Three-Arm RCT Exploring the Delivery of Intensive, Prophylactic Swallowing Therapy to Patients with Head and Neck Cancer During (Chemo)Radiotherapy. Dysphagia 34, 627–639 (2019). https://doi.org/10.1007/s00455-018-9960-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9960-1