Abstract
Pulse oximetry is a commonly used means to measure peripheral capillary oxyhemoglobin saturation (SpO2). Potential use of pulse oximetry to detect aspiration is attractive to clinicians, as it is readily available, quick, and noninvasive. However, research regarding validity has been mixed. This systematic review examining evidence on the use of pulse oximetry to detect a decrease in SpO2 indicating aspiration during swallowing is undertaken to further inform clinical practice in dysphagia assessment. A multi-engine electronic search was conducted on 8/25/16 and updated on 4/8/17 in accordance with standards published by the Preferred Reporting for Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA). Inclusion criteria included use of pulse oximetry to detect aspiration with simultaneous confirmation of aspiration via a gold standard instrumental study. Keywords included dysphagia or aspiration AND pulse oximetry. Articles meeting criteria were reviewed by two blinded co-investigators. The search yielded 294 articles, from which 19 were judged pertinent and reviewed in full. Ten met the inclusion criteria and all were rated at Level III-2 on the Australian Diagnostic Levels of Evidence. Study findings were mixed with sensitivity ranging from 10 to 87%. Potentially confounding variables were observed in all studies reviewed, and commonly involved defining “desaturation” within a standard measurement error range (~ 2%), mixed populations, mixed viscosities/textures observed during swallowing, and lack of comparison group. The majority of studies failed to demonstrate an association between observed aspiration and oxygen desaturation. Current evidence does not support the use of pulse oximetry to detect aspiration.


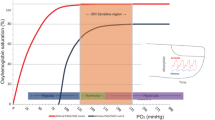
Image source Wikimedia Commons contributors, 'File:Oxyhaemoglobin dissociation curve.png', Wikimedia Commons, the free media repository, 19 February 2017, 01:04 UTC, (https://commons.wikimedia.org/w/index.php?title=File:Oxyhaemoglobin_dissociation_curve.png&oldid=234162700) [accessed 26 November 2017]
Similar content being viewed by others
References
Miller RM, Britton D. Dysphagia in neuromuscular diseases. In: Jones H, Rosenbek J, editors. Clinical dysphagia series. San Diego: Plural Publishing Inc.; 2011.
Gallegos C, et al. Nutritional aspects of dysphagia management. Adv Food Nutr Res. 2017;81:271–318.
Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010;136(8):784–9.
Zaidi NH, et al. Oxygen desaturation on swallowing as a potential marker of aspiration in acute stroke. Age Ageing. 1995;24(4):267–70.
Collins MJ, Bakheit AM. Does pulse oximetry reliably detect aspiration in dysphagic stroke patients? Stroke. 1997;28(9):1773–5.
Tremper KK, Barker SJ. Pulse oximetry. Anesthesiology. 1989;70(1):98–108.
Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med. 2013;107(6):789–99.
Colebatch HJH, Halmagyi DFJ. Reflex airway reaction to fluid aspiration. J Appl Physiol. 1962;17(5):787–94.
Ackerman MH. The effect of saline lavage prior to suctioning. Am J Crit Care. 1993;2(4):326–30.
Rodriguez-Roisin R, et al. Ventilation-perfusion mismatch after methacholine challenge in patients with mild bronchial asthma. Am Rev Respir Dis. 1991;144(1):88–94.
Clave P, et al. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27(6):806–15.
Rofes L, et al. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil. 2014;26(9):1256–65.
Colodny N. Pulse oximetry as an indicator for aspiration: the state of the art. ASHA. SIG13 Perspect. Swallowing Swallowing Disord. 2004;13:9–13.
Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Shamseer L, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Brown PA, et al. Conducting systematic evidence reviews: core concepts and lessons learned. Arch Phys Med Rehabil. 2012;93(8 Suppl):S177–84.
Merlin T, Weston A, Tooher R. Extending an evidence hierarchy to include topics other than treatment: revising the Australian ‘levels of evidence’. BMC Med Res Methodol. 2009;9:34.
Higo R, et al. Pulse oximetry monitoring for the evaluation of swallowing function. Eur Arch Otorhinolaryngol. 2003;260(3):124–7.
Sellars C, Dunnet C, Carter R. A preliminary comparison of videofluoroscopy of swallow and pulse oximetry in the identification of aspiration in dysphagic patients. Dysphagia. 1998;13(2):82–6.
Sherman B, et al. Assessment of dysphagia with the use of pulse oximetry. Dysphagia. 1999;14(3):152–6.
Smith HA, et al. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age Ageing. 2000;29(6):495–9.
Wang TG, et al. Pulse oximetry does not reliably detect aspiration on videofluoroscopic swallowing study. Arch Phys Med Rehabil. 2005;86(4):730–4.
Chong MS, et al. Bedside clinical methods useful as screening test for aspiration in elderly patients with recent and previous strokes. Ann Acad Med Singap. 2003;32(6):790–4.
Colodny N. Comparison of dysphagics and nondysphagics on pulse oximetry during oral feeding. Dysphagia. 2000;15(2):68–73.
Leder SB. Use of arterial oxygen saturation, heart rate, and blood pressure as indirect objective physiologic markers to predict aspiration. Dysphagia. 2000;15(4):201–5.
Marian T, et al. Measurement of oxygen desaturation is not useful for the detection of aspiration in dysphagic stroke patients. Cerebrovasc Dis Extra. 2017;7(1):44–50.
Jubran A. Pulse oximetry. Crit Care. 2015;19:272.
Van de Louw A, et al. Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 2001;27(10):1606–13.
Webb RK, Ralston AC, Runciman WB. Potential errors in pulse oximetry. II. Effects of changes in saturation and signal quality. Anaesthesia. 1991;46(3):207–12.
Tonelli MR, et al. An official multi-society statement: the role of clinical research results in the practice of critical care medicine. Am J Respir Crit Care Med. 2012;185(10):1117–24.
Steele CM, Grace-Martin K. Reflections on clinical and statistical use of the penetration-aspiration scale. Dysphagia. 2017;32(5):1–16.
Butler SG, et al. Effects of liquid type, delivery method, and bolus volume on penetration-aspiration scores in healthy older adults during flexible endoscopic evaluation of swallowing. Ann Otol Rhinol Laryngol. 2011;120(5):288–95.
Leonard RJ, et al. Effects of bolus rheology on aspiration in patients with dysphagia. J Acad Nutr Diet. 2014;114(4):590–4.
Rofes L, et al. The effects of a xanthan gum-based thickener on the swallowing function of patients with dysphagia. Aliment Pharmacol Ther. 2014;39(10):1169–79.
Pierson DJ, Kacmarek RM. Respiratory failure: introduction and overview, in foundations of respiratory care. New York: Churchill Livingstone; 1992. p. 295–302.
Jubran A, Tobin MJ. Monitoring during mechanical ventilation. Clin Chest Med. 1996;17(3):453–73.
Martin-Harris B, et al. Breathing and swallowing dynamics across the adult lifespan. Arch Otolaryngol. 2005;131(9):762–70.
Hadjikoutis S, et al. Abnormal patterns of breathing during swallowing in neurological disorders. Brain. 2000;123(Pt 9):1863–73.
Acknowledgements
The authors would like to thank Breanna Schwarz, B.S., for her assistance with literature searches and data organization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Deanna Britton continues to receive royalties from Plural Publishing, Pro-Ed, Inc., and Medbridge Education. She is additionally affiliated (Affiliate Assistant Professor) with the Department of Rehabilitation Medicine at the University of Washington, Seattle, WA. Joshua O. Benditt owns stock in Ventec. The remaining authors indicate no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Britton, D., Roeske, A., Ennis, S.K. et al. Utility of Pulse Oximetry to Detect Aspiration: An Evidence-Based Systematic Review. Dysphagia 33, 282–292 (2018). https://doi.org/10.1007/s00455-017-9868-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9868-1