Abstract
Patient adherence to treatment recommendations is an important issue for healthcare providers, in a multitude of specialties, and is critical when assessing the efficacy and effectiveness of a particular treatment approach. Patients who have swallowing impairment often require complex and specific interventions requiring altered daily patterns of behavior. Patients with dysphagia who do not follow recommendations or prescribed exercises may not receive maximum benefit of an intervention. Poor adherence also makes it more difficult to evaluate efficacy of a treatment both clinically and in experimental settings. Further, swallow safety can be compromised if certain recommendations are not followed. Our purpose was to systematically review the literature to understand what is known about adherence within the field of dysphagia treatment. We systematically identified 12 studies that tracked and reported patient-specific adherence. In this review, we found that the average adherence rate from these studies ranges between 21.9 and 51.9%. Adherence to prophylactic treatment recommendations for patients with head and neck cancer was the focus in 9/12 studies. The findings of this review identify a large gap in knowledge regarding adherence to dysphagia treatment. Few studies account for adherence within their study designs. When planning dysphagia treatment studies, it is imperative that investigators include information regarding patient adherence to accurately interpret findings. Given the variable adherence rates found in this review, factors influencing patient adherence with dysphagia treatments should be identified to increase adherence in future trials.


Similar content being viewed by others
Change history
04 May 2018
The original version of this article unfortunately contains mistakes. The second sentence in the section “Results”, under the heading “Study Design” was incorrect. It should read as: Two studies [24, 29] used a prospective cohort study design with a JAMA rating of 2. Four studies [17, 25, 27, 34] completed retrospective studies earning a JAMA score of 3. Four studies [26, 28, 30, 33] earned a JAMA quality rating score of 4 and used the following designs: case series [26, 28, 33], and pilot study [30]. In Table 1, “Study Population (n)” and “Design (JAMA quality rating)” values were incorrect for Shinn et al. (2013) [24]. The correct information is given here. HNC (n = 109) Prospective Cohort (2).
References
Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–42.
Donovan JL. Patient decision making: the missing ingredient in compliance research. Int J Technol Assess Health Care. 1995;11:443–55.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30.
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811.
Jack K, McLean SM, Moffett JK, Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther. 2010;15:220–8.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7.
Bartlett EE, Grayson M, Barker R, Levine DM, Golden A, Libber S. The effects of physician communications skills on patient satisfaction; recall, and adherence. J Chronic Dis. 1984;37:755–64.
Egolf RJ, BeGole EA, Upshaw HS. Factors associated with orthodontic patient compliance with intraoral elastic and headgear wear. Am J Orthod Dentofac Orthop. 1990;97:336–48.
Chapman K, Walker L, Cluley S, Fabbri L. Improving patient compliance with asthma therapy. Respir Med. 2000;94:2–9.
Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Ann Pharmacother. 1993;27:S1–24.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310.
Morris LS, Schulz R. Patient compliance—an overview. J Clin Pharm Ther. 1992;17:283–95.
Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99.
Lancaster J. Dysphagia: its nature, assessment and management. Br J Community Nurs. 2015. doi:10.12968/bjcn.2015.20.Sup6a.S28.
Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:98.
Serra-Prat M, Palomera M, Gomez C, Sar-Shalom D, Saiz A, Montoya JG, Navajas M, Palomera E, Clavé P. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: a population-based prospective study. Age Ageing. 2012;41:376–81.
Low J, Wyles C, Wilkinson T, Sainsbury R. The effect of compliance on clinical outcomes for patients with dysphagia on videofluoroscopy. Dysphagia. 2001;16:123–7.
Baijens LW, Clavé P, Cras P, Ekberg O, Forster A, Kolb GF, Leners J-C, Masiero S, Mateos-Nozal J, Ortega O. European Society for Swallowing Disorders-European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403.
Zolnierek KBH, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826.
Namasivayam AM, Steele CM, Keller H. The effect of tongue strength on meal consumption in long term care. Clin Nutr. 2016;35:1078–83.
Wright RW, Brand RA, Dunn W, Spindler KP. How to write a systematic review. Clin Orthop Relat Res. 2007;455:23–9.
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10.
Benzies KM, Premji S, Hayden KA, Serrett K. State-of-the-evidence reviews: advantages and challenges of including grey literature. Worldviews Evid Based Nurs. 2006;3:55–61.
Shinn EH, Basen-Engquist K, Baum G, Steen S, Bauman RF, Morrison W, Garden AS, Sheil C, Kilgore K, Hutcheson KA. Adherence to preventive exercises and self-reported swallowing outcomes in post-radiation head and neck cancer patients. Head Neck. 2013;35:1707–12.
Hutcheson KA, Bhayani MK, Beadle BM, Gold KA, Shinn EH, Lai SY, Lewin J. Eat and exercise during radiotherapy or chemoradiotherapy for pharyngeal cancers: use it or lose it. JAMA Otolaryngol Head Neck Surg. 2013;139:1127–34.
Duarte VM, Chhetri DK, Liu YF, Erman AA, Wang MB. Swallow preservation exercises during chemoradiation therapy maintains swallow function. Otolaryngol-Head Neck Surg. 2013;149(6):878–84.
Starmer H, Sanguineti G, Marur S, Gourin CG. Multidisciplinary head and neck cancer clinic and adherence with speech pathology. Laryngoscope. 2011;121:2131–5.
Cnossen IC, van Uden-Kraan CF, Rinkel RN, Aalders IJ, de Goede CJ, de Bree R, Doornaert P, Rietveld DH, Langendijk JA, Witte BI. Multimodal guided self-help exercise program to prevent speech, swallowing, and shoulder problems among head and neck cancer patients: a feasibility study. J Med Internet Res. 2014;16:e74.
Cnossen IC, van Uden-Kraan CF, Witte BI, Aalders YJ, de Goede CJ, de Bree R, Doornaert P, Rietveld DH, Buter J, Langendijk JA. Prophylactic exercises among head and neck cancer patients during and after swallowing sparing intensity modulated radiation: adherence and exercise performance levels of a 12-week guided home-based program. Eur Arch Oto-Rhino-Laryngol. 2016;274:1129–39.
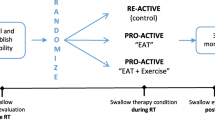
Hajdú SF, Wessel I, Johansen C, Kristensen CA, Kadkhoda ZT, Plaschke CC, Dalton SO. Swallowing therapy and progressive resistance training in head and neck cancer patients undergoing radiotherapy treatment: randomized control trial protocol and preliminary data. Acta Oncol. 2017;56:354–9.
Krisciunas GP, Castellano K, McCulloch TM, Lazarus CL, Pauloski BR, Meyer TK, Graner D, Van Daele DJ, Silbergleit AK, Crujido LR. Impact of compliance on dysphagia rehabilitation in head and neck cancer patients: results from a multi-center clinical trial. Dysphagia. 2016;32:327–36.
Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Adherence to a prophylactic swallowing therapy program during (chemo) radiotherapy: impact of service-delivery model and patient factors. Dysphagia. 2016. doi:10.1007/s00455-016-9757-z.
Leiter A, Windsor J. Compliance of geriatric dysphagic patients with safe-swallowing instructions. J Med Speech Lang Pathol. 1996;4:289–99.
Shim JS, Oh B-M, Han TR. Factors associated with compliance with viscosity-modified diet among dysphagic patients. Ann Rehabil Med. 2013;37:628–32.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9.
DiMatteo MR. Evidence-based strategies to foster adherence and improve patient outcomes: the author’s recent meta-analysis indicates that patients do not follow treatment recommendations unless they know what to do, are committed to doing it, and have the resources to be able to adhere. JAAPA J Am Acad Phys Assist. 2004;17:18–22.
Mekhail TM, Adelstein DJ, Rybicki LA, Larto MA, Saxton JP, Lavertu P. Enteral nutrition during the treatment of head and neck carcinoma. Cancer. 2001;91:1785–90.
Pezner RD, Archambeau JO, Lipsett JA, Kokal WA, Thayer W, Robert L. Tube feeding enteral nutritional support in patients receiving radiation therapy for advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 1987;13:935–9.
Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, Marsh R, Pameijer FA, Balm AJ. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004;60:1425–39.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA: Speech and swallowing rehabilitation for head and neck cancer patients. Oncology (Williston Park, NY). 1997;11:651–6, 659; (discussion 659, 663–4).
Frowen JJ, Perry AR. Swallowing outcomes after radiotherapy for head and neck cancer: a systematic review. Head Neck. 2006;28:932–44.
Frowen J, Cotton S, Corry J, Perry A. Impact of demographics, tumor characteristics, and treatment factors on swallowing after (chemo) radiotherapy for head and neck cancer. Head Neck. 2010;32:513–28.
Stenson KM, MacCracken E, List M, Haraf DJ, Brockstein B, Weichselbaum R, Vokes EE. Swallowing function in patients with head and neck cancer prior to treatment. Arch Otolaryngol Head Neck Surg. 2000;126:371–7.
Kotz T, Federman AD, Kao J, Milman L, Packer S, Lopez-Prieto C, Forsythe K, Genden EM. Prophylactic swallowing exercises in patients with head and neck cancer undergoing chemoradiation: a randomized trial. Arch Otolaryngol Head Neck Surg. 2012;138:376–82.
Mittal BB, Pauloski BR, Haraf DJ, Pelzer HJ, Argiris A, Vokes EE, Rademaker A, Logemann JA. Swallowing dysfunction—preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J Radiat Oncol Biol Phys. 2003;57:1219–30.
Adams AS, Soumerai SB, Lomas J, Ross-Degnan D. Evidence of self-report bias in assessing adherence to guidelines. Int J Qual Health Care. 1999;11:187–92.
Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42:649–52.
Bollen JC, Dean SG, Siegert RJ, Howe TE, Goodwin VA. A systematic review of measures of self-reported adherence to unsupervised home-based rehabilitation exercise programmes, and their psychometric properties. BMJ Open. 2014;4:e005044.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53:1483–9.
Rogus-Pulia N, Rusche N, Hind JA, Zielinski J, Gangnon R, Safdar N, Robbins J. Effects of device-facilitated isometric progressive resistance oropharyngeal therapy on swallowing and health-related outcomes in older adults with dysphagia. J Am Geriatr Soc. 2016;64:417–24.
Oh J-C. Effects of tongue strength training and detraining on tongue pressures in healthy adults. Dysphagia. 2015;30:315–20.
Colodny N. Dysphagic independent feeders’ justifications for noncompliance with recommendations by a speech-language pathologist. Am J Speech Lang Pathol. 2005;14:61–70.
Sabaté E. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, Wilson K, Buchan I, Gill CJ, Cooper C. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3:e438.
Rodrigues IB, Armstrong JJ, Adachi JD, MacDermid JC. Facilitators and barriers to exercise adherence in patients with osteopenia and osteoporosis: a systematic review. Osteoporos Int. 2017;28:735–45.
Warburton DE, Nicol CW, Bredin SS. Prescribing exercise as preventive therapy. Can Med Assoc J. 2006;174:961–74.
Carayon P, Hundt AS, Karsh B, Gurses A, Alvarado C, Smith M, Brennan PF. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15:i50–8.
Smith-Tamaray M, Wilson L, McAllister L. Factors affecting dysphagia management and compliance with recommendations in non-metropolitan healthcare settings. Int J Speech Lang Pathol. 2011;13:268–79.
Edmonds MF, McGuire DB. Treatment adherence in head and neck cancer patients undergoing radiation therapy: challenges for nursing. J Radiol Nurs. 2007;26:87–92.
Rosenvinge SK, Starke ID. Improving care for patients with dysphagia. Age Ageing. 2005;34:587–93.
Rogus-Pulia N, Hind J: Patient-centered dysphagia therapy—the critical impact of self-efficacy. SIG 13 Perspectives on Swallowing and Swallowing Disorders. Dysphagia. 2015;24:146–54.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191.
Zimmerman BJ. Self-efficacy: an essential motive to learn. Contemp Educ Psychol. 2000;25:82–91.
van Leer E, Hapner ER, Connor NP. Transtheoretical model of health behavior change applied to voice therapy. J Voice. 2008;22:688–98.
Desharnais R, Bouillon J, Godin G. Self-efficacy and outcome expectations as determinants of exercise adherence. Psychol Rep. 1986;59:1155–9.
Marks R, Allegrante JP. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract. 2005;6:148–56.
van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res. 2007;7:55.
Funding
This study was funded in part by the National Institute on Deafness and Other Communication Disorders (R01DC005935, R01DC008149, R01DC014358, T32-DC009401).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Krekeler, B.N., Broadfoot, C.K., Johnson, S. et al. Patient Adherence to Dysphagia Recommendations: A Systematic Review. Dysphagia 33, 173–184 (2018). https://doi.org/10.1007/s00455-017-9852-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9852-9