Abstract
Introduction
Radiosurgery (SRS) or stereotactic fractionated radiotherapy (SFRT) is increasing in the treatment of brain metastases (BMs). Aim of the present study was to evaluate the safety and effectiveness of SRS/SFRT for BMs, using a new mono-isocenter non-coplanar solution (HyperArc™ Varian Medical System).
Methods
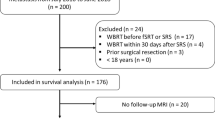
BMs patients with a diameter inferior to 3 cm, a life expectancy of more than 3 months and a good performance status, were eligible for Linac-based volumetric modulated arc therapy (VMAT) SFRT/SRS with HyperArc™. A retrospective analysis of patients and BMs was performed.
Results
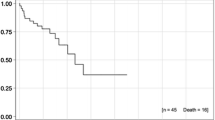
From August 2017 to May 2018, 381 BMs in 64 patients were treated and 246 BMs (43 patients, median number of BMs: 5) of them were suitable for analysis. With a median FU time of 6 months, 244 out 246 (99%) BMs were controlled (18% complete response; 41% partial response, 40% stable disease), 2 BMs showed a progression, at the first control. No acute or late toxicities were reported. Median overall survival (OS) has not yet been achieved, while median time to progression was 5 months. In univariate analysis, statistically negative prognostic factors for OS were histology of primary tumor (p = 0.009): lung/breast cancer had better survival rates as compared to others. Cumulative intracranial volume disease ≥ 15 cc and systemic progression disease were independent prognostic factors for OS at univariate (p = 0.04; p = 0.005) and multivariate (p = 0.04; p = 0.009) analysis, respectively.
Conclusion
The present first clinical data show that SFRT/SRS with HyperArc™ is safe and effective for BMs patients. The utilization of SFRT/SRS for BMs is promising and should be further explored in randomized trials.


Similar content being viewed by others
References
Alongi F, Fiorentino A, Mancosu P et al (2016) Stereotactic radiosurgery for intracranial metastases: linac-based and gamma-dedicated unit approach. Expert Rev Anticancer Ther 16(7):731–740
Aoyama H, Shirato H, Tago M et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Bachelot T, Romieu G, Campone M et al (2013) Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol 14(1):64–71
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316(4):401–409
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Davis FG, Dolecek TA, McCarthy BJ et al (2012) Toward determining the lifetime occurrence of metastatic brain tumors estimated from 2007 United States cancer incidence data. Neuro Oncol 14:1171–1177
De Mattos-Arruda L, Nag C, Piscuoglio S et al (2018) Genetic heterogeneity and actionable mutations in HER2-positive primary breast cancers and their brain metastases. Oncotarget 9(29):20617–20630
Fiorentino A, Tebano U, Sicignano G et al (2018) Hippocampal dose during Linac-based stereotactic radiotherapy for brain metastases: an observational study. Phys Med 49:135–138
Giaj Levra N, Sicignano G, Fiorentino A et al (2016) Whole brain radiotherapy with hippocampal avoidance and simultaneous integrated boost for brain metastases: a dosimetric volumetric-modulated arc therapy study. Radiol Med 121(1):60–69
Halasz LM, Uno H, Hughes M et al (2016) Comparative effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for patients with brain metastases from breast or nonsmall cell lung cancer. Cancer 122(13):2091–2100
Kennecke H, Yerushalmi R, Woods R et al (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28(20):3271–3277
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29:134–141
Kocher M, Wittig A, Piroth MD et al (2014) Stereotactic radiosurgery for treatment of brain metastases. A report of the DEGRO Working Group on Stereotactic Radiotherapy. Strahlenther Onkol 190(6):521–532
Kohutek ZA, Yamada Y, Chan TA et al (2015) Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J Neurooncol 125(1):149–156
Lin NU, Claus E, Sohl J et al (2008) Sites of distant recurrence and clinical outcomes in patients with metastatic triple-negative breast cancer: high incidence of central nervous system metastases. Cancer 113(10):2638–2645
Long GV, Flaherty KT, Stroyakovskiy D et al (2017) Dabrafenib plus trametinib versus dabrafenib monotherapy in patients with metastatic BRAF V600E/K-mutant melanoma: long-term survival and safety analysis of a phase 3 study. Ann Oncol 28(7):1631–1639
Magnuson WJ, Lester-Coll NH, Wu AJ et al (2017) Management of brain metastases in tyrosine kinase inhibitor-naive epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol 35(10):1070–1077
Margolin K, Ernstoff MS, Hamid O et al (2012) Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol 13(5):459–465
Minniti G, Clarke E, Lanzetta G et al (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6:48
Moraes FY, Winter J, Atenafu EG et al (2018) Outcomes following SRS for small- to medium-sized brain metastases are exceptionally dependent upon tumor size and prescribed dose. Neuro Oncol. https://doi.org/10.1093/neuonc/noy159
Muller-Riemenschneider F, Bockelbrink A, Ernst I et al (2009) Stereotactic radiosurgery for the treatment of brain metastases. Radiother Oncol 91:67–74
Nayak L, Lee EQ, Wen PY et al (2012) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
NCCN Central Nervous System Cancers (2018) Version 1.2018 guidelines. https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf. Accessed Sept 2018
O’Sullivan CC, Davarpanah N, Abraham J, Bates SE (2017) Current challenges in the management of breast cancer brain metastases. Semin Oncol 44:85–100
Regina A, Demeule M, Che C et al (2008) Anti tumour activity of ANG1005, a conjugate between paclitaxel and the new brain delivery vector Angiopep-2. Br J Pharmacol 155(2):185–197
Robin TP, Camidge DR, Stuhr K et al (2018) Excellent outcomes with radiosurgery for multiple brain metastases in ALK and EGFR driven non-small cell lung cancer. J Thorac Oncol 13(5):715–720
Ruggieri R, Naccarato S, Mazzola R et al (2018) Linac-based VMAT radiosurgery for multiple brain lesions: comparison between a conventional multi-isocenter approach and a new dedicated mono-isocenter technique. Radiat Oncol 13(1):38
Sahgal A, Aoyama H, Kocher M et al (2015) Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol 91(4):710–717
Sahgal A, Ruschin M, Ma L et al (2017) Stereotactic radiosurgery alone for multiple brain metastases? A review of clinical and technical issues. Neuro Oncol 19(suppl_2):ii2–ii15
Schwartz LH, Seymour L, Litière S et al (2016) RECIST 1.1—standardisation and disease-specific adaptations: perspectives from the RECIST working group. Eur J Cancer 62:138–145
Scoccianti S, Ricardi U (2012) Treatment of brain metastases: review of phase III randomized controlled trials. Radiother Oncol 102:168–179
Sperduto PW, Kased N, Roberge D et al (2012) Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30(4):419–425
Weber JS, D’Angelo SP, Minor D et al (2015) Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 16:375–384
Wiggenraad R, Verbeek-de Kanter A, Kal HB, et (2011) Dose–effect relation in stereotactic radiotherapy for brain metastases. A systematic review. Radiother Oncol 98:292–297
Yamamoto M, Serizawa T, Shuto T et al (2014) Results of stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective study. Lancet Oncol 15:387–395
Funding
No funding or financial interests for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
For this type of study formal consent is not required. However, all procedures were in accordance with the ethical standards and the Helsinki declaration.
Informed consent
A specific informed consent was obtained from all individual participants included in the study.
Conflict of interest
FA acts as Varian Consultant and he had Speacker Onoraria. Remaining authors (AF, FG, SC, NGL, LR, MR, FR, AB, GL, RM, RR) declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Alongi, F., Fiorentino, A., Gregucci, F. et al. First experience and clinical results using a new non-coplanar mono-isocenter technique (HyperArc™) for Linac-based VMAT radiosurgery in brain metastases. J Cancer Res Clin Oncol 145, 193–200 (2019). https://doi.org/10.1007/s00432-018-2781-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2781-7