Abstract
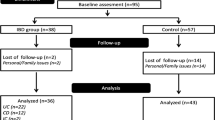
Nutritional status and dietary intake in pediatric-onset inflammatory bowel disease are complex and need to be further explored. Therefore, we have assessed anthropometric measures, body composition, and dietary intake of newly diagnosed pediatric patients, and compared them with healthy controls. This was a prospective cross-sectional study including newly diagnosed patients with inflammatory bowel disease (n = 89) and healthy controls (n = 159). Mean energy intake was significantly lower in healthy controls compared to patients with ulcerative colitis, but not in patients with Crohn’s disease. Intake of all macronutrients, dietary fiber, and calcium was significantly lower in patients with ulcerative colitis, whereas the only intake of animal protein, fruit, and calcium differed significantly in patients with Crohn’s disease. There were no significant differences in the body fat percentage between patients with ulcerative colitis or Crohn’s disease vs. controls; however, lean mass-for-age z-scores were significantly lower in patients with both diseases in comparison to controls.
Conclusion: Food intake of newly diagnosed pediatric patients with inflammatory bowel disease significantly differed from healthy controls. Altered anthropometry and body composition are present already at the time of diagnosis.
What is Known: • Children with inflammatory bowel disease suffer from malnutrition, especially children with Crohn’s disease in whom linear growth failure often precedes gastrointestinal symptoms. | |
What is New: • This study showed significantly lower intake of energy, macronutrients, and various micronutrients in patients with ulcerative colitis compared to healthy controls, while patients with Crohn’s disease have a lower intake of fruits, calcium, and animal protein at diagnosis. • Altered body composition is present in both groups of patients at the time of diagnosis. |

Similar content being viewed by others
Change history
23 January 2020
The authors of the published original version of the above article wanted to correct the below text in the Abstract section.
Abbreviations
- CD:
-
Crohn’s disease
- IBD:
-
Inflammatory bowel disease
- UC:
-
Ulcerative colitis
- PCDAI:
-
Pediatric Crohn’s disease activity index
- PUCAI:
-
Pediatric ulcerative colitis activity index
References
Sawczenko A, Sandhu BK, Logan RF, Jenkins H, Taylor CJ, Mian S, Lynn R (2001) Prospective survey of childhood inflammatory bowel disease in the British Isles. Lancet 357(9262):1093–1094
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG (2018) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390(10114):2769–2778. https://doi.org/10.1016/S0140-6736(17)32448-0
Amre DK, D'Souza S, Morgan K, Seidman G, Lambrette P, Grimard G, Israel D, Mack D, Ghadirian P, Deslandres C, Chotard V, Budai B, Law L, Levy E, Seidman EG (2007) Imbalances in dietary consumption of fatty acids, vegetables, and fruits are associated with risk for Crohn’s disease in children. Am J Gastroenterol 102(9):2016–2025. https://doi.org/10.1111/j.1572-0241.2007.01411.x
Levine A, Sigall Boneh R, Wine E (2018) Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut 67(9):1726–1738. https://doi.org/10.1136/gutjnl-2017-315866
Hildebrand H, Karlberg J, Kristiansson B (1994) Longitudinal growth in children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 18(2):165–173
Jakobsen C, Paerregaard A, Munkholm P, Faerk J, Lange A, Andersen J, Jakobsen M, Kramer I, Czernia-Mazurkiewicz J, Wewer V (2011) Pediatric inflammatory bowel disease: increasing incidence, decreasing surgery rate, and compromised nutritional status: a prospective population-based cohort study 2007-2009. Inflamm Bowel Dis 17(12):2541–2550. https://doi.org/10.1002/ibd.21654
Filippi J, Al-Jaouni R, Wiroth JB, Hebuterne X, Schneider SM (2006) Nutritional deficiencies in patients with Crohn’s disease in remission. Inflamm Bowel Dis 12(3):185–191. https://doi.org/10.1097/01.MIB.0000206541.15963.c3
Hyams JS (2005) Inflammatory bowel disease. Pediatr Rev 26(9):314–320. https://doi.org/10.1542/pir.26-9-314
Kugathasan S, Nebel J, Skelton JA, Markowitz J, Keljo D, Rosh J, LeLeiko N, Mack D, Griffiths A, Bousvaros A, Evans J, Mezoff A, Moyer S, Oliva-Hemker M, Otley A, Pfefferkorn M, Crandall W, Wyllie R, Hyams J, Wisconsin Pediatric Inflammatory Bowel Disease A, Pediatric Inflammatory Bowel Disease Collaborative Research G (2007) Body mass index in children with newly diagnosed inflammatory bowel disease: observations from two multicenter North American inception cohorts. J Pediatr 151(5):523–527. https://doi.org/10.1016/j.jpeds.2007.04.004
Long MD, Crandall WV, Leibowitz IH, Duffy L, del Rosario F, Kim SC, Integlia MJ, Berman J, Grunow J, Colletti RB, Schoen BT, Patel AS, Baron H, Israel E, Russell G, Ali S, Herfarth HH, Martin C, Kappelman MD, ImproveCareNow Collaborative for Pediatric IBD (2011) Prevalence and epidemiology of overweight and obesity in children with inflammatory bowel disease. Inflamm Bowel Dis 17(10):2162–2168. https://doi.org/10.1002/ibd.21585
Gerasimidis K, McGrogan P, Edwards CA (2011) The aetiology and impact of malnutrition in paediatric inflammatory bowel disease. J Hum Nutr Diet 24(4):313–326. https://doi.org/10.1111/j.1365-277X.2011.01171.x
Pons R, Whitten KE, Woodhead H, Leach ST, Lemberg DA, Day AS (2009) Dietary intakes of children with Crohn’s disease. Br J Nutr 102(7):1052–1057. https://doi.org/10.1017/S0007114509359085
Hartman C, Marderfeld L, Davidson K, Mozer-Glassberg Y, Poraz I, Silbermintz A, Zevit N, Shamir R (2016) Food intake adequacy in children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 63(4):437–444. https://doi.org/10.1097/MPG.0000000000001170
Thomas AG, Taylor F, Miller V (1993) Dietary intake and nutritional treatment in childhood Crohn’s disease. J Pediatr Gastroenterol Nutr 17(1):75–81
Diederen K, Krom H, Koole JCD, Benninga MA, Kindermann A (2018) Diet and anthropometrics of children with inflammatory bowel disease: a comparison with the general population. Inflamm Bowel Dis 24(8):1632–1640. https://doi.org/10.1093/ibd/izy027
Tsiountsioura M, Wong JE, Upton J, McIntyre K, Dimakou D, Buchanan E, Cardigan T, Flynn D, Bishop J, Russell RK, Barclay A, McGrogan P, Edwards C, Gerasimidis K (2014) Detailed assessment of nutritional status and eating patterns in children with gastrointestinal diseases attending an outpatients clinic and contemporary healthy controls. Eur J Clin Nutr 68(6):700–706. https://doi.org/10.1038/ejcn.2013.286
Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, Kolho KL, Veres G, Russell RK, Paerregaard A, Buderus S, Greer ML, Dias JA, Veereman-Wauters G, Lionetti P, Sladek M, Martin de Carpi J, Staiano A, Ruemmele FM, Wilson DC, European Society of Pediatric Gastroenterology H, Nutrition (2014) ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58(6):795–806. https://doi.org/10.1097/MPG.0000000000000239
Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, Fell J, Ruemmele FM, Walters T, Sherlock M, Dubinsky M, Hyams JS (2011) Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis 17(6):1314–1321. https://doi.org/10.1002/ibd.21493
Hyams JS, Ferry GD, Mandel FS, Gryboski JD, Kibort PM, Kirschner BS, Griffiths AM, Katz AJ, Grand RJ, Boyle JT, Michener WM, Levy JS, Lesser ML (1991) Development and validation of a pediatric Crohn’s disease activity index. J Pediatr Gastroenterol Nutr 12(4):439–447
Turner D, Otley AR, Mack D, Hyams J, de Bruijne J, Uusoue K, Walters TD, Zachos M, Mamula P, Beaton DE, Steinhart AH, Griffiths AM (2007) Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology 133(2):423–432. https://doi.org/10.1053/j.gastro.2007.05.029
Addo OY, Himes JH (2010) Reference curves for triceps and subscapular skinfold thicknesses in US children and adolescents. Am J Clin Nutr 91(3):635–642. https://doi.org/10.3945/ajcn.2009.28385
Wells JC, Williams JE, Chomtho S, Darch T, Grijalva-Eternod C, Kennedy K, Haroun D, Wilson C, Cole TJ, Fewtrell MS (2012) Body-composition reference data for simple and reference techniques and a 4-component model: a new UK reference child. Am J Clin Nutr 96(6):1316–1326. https://doi.org/10.3945/ajcn.112.036970
WHO Multicentre Growth Reference Study Group (2006) WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization, Geneva (312 pages)
Firouzbakhsh S, Mathis RK, Dorchester WL, Oseas RS, Groncy PK, Grant KE, Finklestein JZ (1993) Measured resting energy expenditure in children. J Pediatr Gastroenterol Nutr 16(2):136–142
Mocic Pavic A, Detelic D, Hojsak I, Kolacek S (2015) Validation of a food frequency questionnaire for adolescents in Croatia. J Pediatr Gastroenterol Nutr 60:835–836
Nutrient Data Laboratory (U.S.), & Consumer and Food Economics Institute (U.S.) (1999) USDA nutrient database for standard reference. USDA, Nutrient Data Laboratory, Agricultural Research Service, Riverdale, Md
Kaic-Rak A, Antonic K (1990) Tablice o sastavu namirnica i pića. Zavod za zaštitu zdravlja R Hrvatske, Zagreb
Hagin S, Lobato DJ, Sands BE, Korzenik J, Merrick M, Shah S (2017) Dietary behaviors in newly diagnosed youth with inflammatory bowel disease. Child Health Care 46(4):408–420
Serrano-Montalban B, Arias A, Friginal-Ruiz AB, Lucendo AJ (2017) The use of the fracture risk assessment (FRAX(R)) tool in predicting risk of fractures in patients with inflammatory bowel disease: a systematic review. J Clin Densitom 20(2):180–187. https://doi.org/10.1016/j.jocd.2016.08.010
Donnellan CF, Yann LH, Lal S (2013) Nutritional management of Crohn’s disease. Ther Adv Gastroenterol 6(3):231–242. https://doi.org/10.1177/1756283X13477715
Owczarek D, Rodacki T, Domagala-Rodacka R, Cibor D, Mach T (2016) Diet and nutritional factors in inflammatory bowel diseases. World J Gastroenterol 22(3):895–905. https://doi.org/10.3748/wjg.v22.i3.895
Veereman-Wauters G, de Ridder L, Veres G, Kolacek S, Fell J, Malmborg P, Koletzko S, Dias JA, Misak Z, Rahier JF, Escher JC, Group EIP (2012) Risk of infection and prevention in pediatric patients with IBD: ESPGHAN IBD Porto Group commentary. J Pediatr Gastroenterol Nutr 54(6):830–837. https://doi.org/10.1097/MPG.0b013e31824d1438
Vasseur F, Gower-Rousseau C, Vernier-Massouille G, Dupas JL, Merle V, Merlin B, Lerebours E, Savoye G, Salomez JL, Cortot A, Colombel JF, Turck D (2010) Nutritional status and growth in pediatric Crohn’s disease: a population-based study. Am J Gastroenterol 105(8):1893–1900. https://doi.org/10.1038/ajg.2010.20
El Mouzan MI, Al Edreesi MH, Al-Hussaini AA, Saadah OI, Al Qourain AA, Al Mofarreh MA, Al Saleem KA (2016) Nutritional status of children with inflammatory bowel disease in Saudi Arabia. World J Gastroenterol 22(5):1854–1858. https://doi.org/10.3748/wjg.v22.i5.1854
Croatian Institute of Public Health. Health Behaviour in School-aged Children – HBSC 2013/2014
Harper JW, Zisman TL (2016) Interaction of obesity and inflammatory bowel disease. World J Gastroenterol 22(35):7868–7881. https://doi.org/10.3748/wjg.v22.i35.7868
Burnham JM, Shults J, Semeao E, Foster BJ, Zemel BS, Stallings VA, Leonard MB (2005) Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am J Clin Nutr 82(2):413–420. https://doi.org/10.1093/ajcn.82.2.413
Wiskin AE, Wootton SA, Hunt TM, Cornelius VR, Afzal NA, Jackson AA, Beattie RM (2011) Body composition in childhood inflammatory bowel disease. Clin Nutr 30(1):112–115. https://doi.org/10.1016/j.clnu.2010.07.014
Acknowledgments
We thank Professor Mary Fewtrell for her kind help in the calculation of SD scores for lean mass in our patients and healthy controls, with the new UK reference data for pediatric body composition developed as a part of her research.
Funding
This study was part of a research project IP-2014-09-3788 funded by the Croatian Science Foundation.
Author information
Authors and Affiliations
Contributions
SS was responsible for writing the research protocol, conducting the research, extracting the data, interpreting the results, and writing the manuscript. IT was responsible for writing the protocol, conducting the research, extracting the data, interpreting the results, and writing the manuscript. AMP was responsible for writing the protocol, conducting the research, extracting the data, and reviewing the manuscript. TN was responsible for conducting the research, interpreting the results, and reviewing the manuscript. SK was responsible for designing the research protocol, interpreting the results, and reviewing the manuscript. IH was responsible for designing the research protocol, analyzing the data, interpreting the results and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Iva Hojsak received payment/honorarium for lectures or consultation from BioGaia, Nutricia, Nestle, GM pharma, and Chr Hansen. Sanja Kolaček received fees for lectures from Abbott, AbbVie, Fresenius, Mead and Johnson, Nestle, Nutricia, and Oktal Pharma. Tena Niseteo received a fee for lectures from 4U Pharma. Sara Sila, Ivana Trivić, and Ana Močić Pavić declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee Children’s Hospital Zagreb (IRB no. 21102014).
Informed consent
Informed consent was obtained from all individual participants and at least one of their parents included in the study.
Additional information
Communicated by Mario Bianchetti
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sila, S., Trivić, I., Pavić, A.M. et al. Nutritional status and food intake in pediatric patients with inflammatory bowel disease at diagnosis significantly differs from healthy controls. Eur J Pediatr 178, 1519–1527 (2019). https://doi.org/10.1007/s00431-019-03443-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03443-3