Abstract
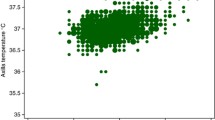
To better understand the role and reliability of axillary temperature measurements in clinical real life, axillary and rectal measurements in infants presenting in a private pediatric practice because of fever were compared. Prospectively, 169 infants (81 girls), median 9 (interquartile range 6–13) months of age, were examined at room temperature (20–24 °C). Two left and two right axillary, as well as two rectal measurements were taken with a digital thermometer and subsequently averaged. The median and interquartile range for axillary and rectal measurements were 36.9 (36.3–37.6) °C and 38.2 (37.4–38.9) °C, respectively (p < 0.0001). The limits of agreement in the Bland-Altman plots were 0.32 to 1.98 °C, with a mean bias of 1.15 °C. Axillary thermometers showed a good sensitivity for detecting rectal temperature > 38 °C (95%) but limited specificity (75%), with an area-under-the-curve of 0.95.
Conclusions: Axillary readings are always lower than rectal ones, the limits of agreement are quite wide. Axillary readings can be used for screening but critical measurements should be confirmed by more reliable methods.
What is Known • In infants and toddlers, temperature has been traditionally taken rectally. • Axillary measurements are better accepted and are recommended in current guidelines. | |
What is New • Axillary temperature was always lower than rectal temperature. • The limits of agreement of axillary thermometers are wide. • Axillary thermometers have a good sensitivity but limited specificity and are therefore adequate for fever screening. |



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- IQR:
-
Interquartile range
- JT :
-
Jan Teller
- ROC:
-
Receiver operating characteristics
- SD:
-
Standard deviation
References
Sarrell EM, Wielunsky E, Cohen HA (2006) Antipyretic treatment in young children with fever: acetaminophen, ibuprofen, or both alternating in a randomized, double-blind study. Arch Pediatr Adolesc Med 160:197–202. https://doi.org/10.1001/archpedi.160.2.197
Lava SA, Simonetti GD, Ferrarini A, Ramelli GP, Bianchetti MG (2013) Regional differences in symptomatic fever management among paediatricians in Switzerland: the results of a cross-sectional web-based survey. Br J Clin Pharmacol 75:236–243. https://doi.org/10.1111/j.1365-2125.2012.04311.x
de Vos-Kerkhof E, Geurts DHF, Steyerberg EW, Lakhanpaul M, Moll HA, Oostenbrink R (2018) Characteristics of revisits of children at risk for serious infections in pediatric emergency care. Eur J Pediatr 177:617–624. https://doi.org/10.1007/s00431-018-3095-0
Chiappini E, Venturini E, Remaschi G, Principi N, Longhi R, Tovo PA, Becherucci P, Bonsignori F, Esposito S, Festini F, Galli L, Lucchesi B, Mugelli A, Marseglia GL, de Martino M, Italian Pediatric Society Panel for the Management of Fever in Children (2017) 2016 Update of the Italian Pediatric Society guidelines for management of fever in children. J Pediatr 180:177–183.e1. https://doi.org/10.1016/j.jpeds.2016.09.043
Teller J, Ragazzi M, Simonetti GD, Lava SA (2014) Accuracy of tympanic and forehead thermometers in private paediatric practice. Acta Paediatr 103:e80–e83. https://doi.org/10.1111/apa.12464
Mogensen CB, Wittenhoff L, Fruerhøj G, Hansen S (2018) Forehead or ear temperature measurement cannot replace rectal measurements, except for screening purposes. BMC Pediatr 18:15. https://doi.org/10.1186/s12887-018-0994-1
Fields E, Chard J, Murphy MS, Richardson M, Guideline Development Group and Technical Team (2013) Assessment and initial management of feverish illness in children younger than 5 years: summary of updated NICE guidance. BMJ 346:f2866. https://doi.org/10.1136/bmj.f2866
Bland JM, Altman DG (2011) Agreed statistics - measurement method comparison. Anesthesiology 116:182–185. https://doi.org/10.1097/ALN.0b013e31823d7784
Paes BF, Vermeulen K, Brohet RM, van der Ploeg T, de Winter JP (2010) Accuracy of tympanic and infrared skin thermometers in children. Arch Dis Child 95:974–978. https://doi.org/10.1136/adc.2010.185801
Avner JR, Baker MD (2002) Management of fever in infants and children. Emerg Med Clin North Am 20:49–67
Schmitt BD (1980) Fever phobia: misconceptions of parents about fevers. Am J Dis Child 134:176–181
Brick T, Agbeko RS, Davies P, Davis PJ, Deep A, Fortune PM, Inwald DP, Jones A, Levin R, Morris KP, Pappachan J, Ray S, Tibby SM, Tume LN, Peters MJ, UK Paediatric Intensive Care Society Study Group (PICS-SG) (2017) Attitudes towards fever amongst UK paediatric intensive care staff. Eur J Pediatr 176:423–427. https://doi.org/10.1007/s00431-016-2844-1
Goldberg S, Heitner S, Mimouni F, Joseph L, Bromiker R, Picard E (2018) The influence of reducing fever on blood oxygen saturation in children. Eur J Pediatr 177:195–199. https://doi.org/10.1007/s00431-018-3188-9
Morley CJ, Hewson PH, Thornton AJ, Cole TJ (1992) Axillary and rectal temperature measurements in infants. Arch Dis Child 67:122–125
Craig JV, Lancaster GA, Williamson PR, Smyth RL (2000) Temperature measured at the axilla compared with rectum in children and young people: systematic review. BMJ 320:1174–1178. https://doi.org/10.1136/bmj.320.7243.1174
Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ, Roberts DJ, Stelfox HT (2015) Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med 163:768–777. https://doi.org/10.7326/M15-1150
Chiappini E, Principi N, Longhi R, Tovo PA, Becherucci P, Bonsignori F, Esposito S, Festini F, Galli L, Lucchesi B, Mugelli A, de Martino M, Writing Committee of the Italian Pediatric Society Panel for the Management of Fever in Children (2009) Management of fever in children: summary of the Italian Pediatric Society guidelines. Clin Ther 31:1826–1843. https://doi.org/10.1016/j.clinthera.2009.08.006
Forrest AJ, Juliano ML, Conley SP, Cronyn PD, McGlynn A, Auten JD (2017) Temporal artery and axillary thermometry comparison with rectal thermometry in children presenting to the ED. Am J Emerg Med 35:1855–1858. https://doi.org/10.1016/j.ajem.2017.06.017
Kettunen S, Lantto U, Koivunen P, Tapiainen T, Uhari M, Renko M (2018) Risk factors for periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA) syndrome: a case-control study. Eur J Pediatr 177:1201–1206. https://doi.org/10.1007/s00431-018-3175-1
Author information
Authors and Affiliations
Contributions
- Study concept and design: JT, SAGL
- Consent, Recruitment, Study execution: JT
- Statistical analysis: RB, SAGL
- Review of the literature, Preparation of the figures, Drafting of the manuscript: RB, SAGL
- Critical revision of the manuscript: GDS, SAGL
- Approval of the final manuscript: JT, RB, GDS, SAGL
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This project was performed in the context of a routine quality assessment. All procedures performed were in accordance with ethical standards as laid down in the 1964 Helsinki declaration.
Informed consent
Caregivers received information on the study and (anonymous) study participation and had to give oral consent in order for their children to be enrolled in the study. Since only infants < 24 months of age were included, children assent was not required.
Additional information
Communicated by Mario Bianchetti
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teller, J., Bernasconi, R., Simonetti, G.D. et al. Performance of axillary and rectal temperature measurement in private pediatric practice. Eur J Pediatr 178, 1501–1505 (2019). https://doi.org/10.1007/s00431-019-03438-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03438-0