Abstract
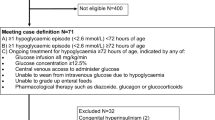
Admission to neonatal care causes separation of infants from their parents, can adversely affect breast-feeding and is associated with painful procedures. Our aim was to identify perinatal factors and cost of care associated with transient neonatal hyperinsulinaemic hypoglycaemia (HH). Infants born after 35 weeks of gestation admitted because of hypoglycaemia were studied. The neonates were divided into two groups (HH and non-HH), and their length and cost of care were compared and perinatal factors predicting those outcomes explored. Forty of the 474 infants admitted with hypoglycaemia were diagnosed with HH. The HH group had a lower median (IQR) glucose level on admission compared to the non-HH group (p < 0.001). The median (IQR) cost of stay was higher in the HH group (p < 0.001). In the HH group, the GIRmax was significantly correlated with cost of stay (p < 0.001). GIRmax predicted a cost of stay > £9140 with an area under the ROC curve of 0.956. GIRmax > 13.9 mg/kg/min predicted admission cost > £9140 with 86% sensitivity and 93% specificity.
Conclusion: Transient neonatal HH was associated with a higher length and cost of stay in infants admitted for hypoglycaemia. The GIRmax can predict the length and cost of stay.
What is Known: • Neonatal hypoglycaemia is the leading cause of term and late preterm neonatal admissions. • Hyperinsulinism (HH) is the commonest cause of persistent hypoglycaemia, and delay in the diagnosis and management can have a detrimental impact on long-term development. | |
What is New: • We have demonstrated prior to NICU admission that blood glucose concentrations were lower in infants with HH compared to those without. • The maximum GIR had a stronger correlation with total length and cost of hospital stay compared to insulin levels in HH infants. |
Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CTG:
-
Cardiotocograph
- FGR:
-
Foetal growth restriction
- GDM:
-
Gestational diabetes mellitus
- GIRmax :
-
Maximum glucose infusion rate
- HH:
-
Hyperinsulinaemic hypoglycaemia
- IQR:
-
Interquartile range
- NICU:
-
Neonatal intensive care unit
- OGTT:
-
Oral glucose tolerance test
- ROC:
-
Receiver operator characteristic curve
References
Arya VB, Flanagan SE, Kumaran A, Shield JP, Ellard S, Hussain K, Kapoor RR (2013) Clinical and molecular characterisation of hyperinsulinaemic hypoglycaemia in infants born small for gestational age. Arch Dis Child Fetal Neonatal Ed 98:F356–F358
British Association of Perinatal Medicine. Identification and management of neonatal hypoglycaemia in the full-term infant – A framework for practice: British Association of Perinatal Medicine; 2017
Burns CM, Rutherford MA, Boardman JP, Cowan FM (2008) Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 122:65–74
Collins JE, Leonard JV, Teale D, Marks V, Williams DM, Kennedy CR, Hall MA (1990) Hyperinsulinaemic hypoglycaemia in small for dates babies. Arch Dis Child 65:1118–1120
Cornblath M, Levin EY, Hopkins J (1959) Symptomatic neonatal hypoglycemia associated with toxemia of pregnancy. J Pediatr 55:545–562
Dassios T, Greenough A, Leontiadi S (2017) Admissions for hypoglycaemia after 35 weeks of gestation: perinatal predictors of cost of stay. J Matern Fetal Neonatal Med 18:1–9
De León DD, Stanley CA (2007) Mechanisms of disease: advances in diagnosis and treatment of hyperinsulinism in neonates. Nat Clin Pract Endocrinol Metab 3:57–68
Fafoula O, Alkhayyat H, Hussain K (2006) Prolonged hyperinsulinaemic hypoglycaemia in newborns with intrauterine growth retardation. Arch Dis Child Fetal Neonatal Ed 91:F467
Ferrara C, Patel P, Becker S, Stanley CA, Kelly A (2016) Biomarkers of insulin for the diagnosis of hyperinsulinemic hypoglycemia in infants and children. J Pediatr 168:212–219
Figueras F, Gratacós E (2014) Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn Ther 36:86–98
Güemes M, Hussain K (2015) Hyperinsulinemic hypoglycemia. Pediatr Clin N Am 62:1017–1036
Harding JE, Hegarty JE, Crowther CA, Edlin R, Gamble G, Alsweiler JM (2015) Randomised trial of neonatal hypoglycaemia prevention with oral dextrose gel (hPOD): study protocol. BMC Pediatr 15:120
Harris DL, Weston PJ, Signal M, Edlin R, Gamble G, Alsweiler JM (2013) Dextrose gel for neonatal hypoglycaemia (the sugar babies study): a randomised, double-blind, placebo-controlled trial. Lancet 382:2077–2083
Harris D, Weston P, Alsweiler J, Thompson B (2014) Two year outcomes of children treated with dextrose gel for neonatal hypoglycaemia: follow up of a randomised trial. Arch Dis Child A64-A65
Hay WW, Raju TN, Higgins RD, Kalhan SC, Devaskar SU (2009) Knowledge gaps and research needs for understanding and treating neonatal hypoglycemia: workshop report from Eunice Kennedy Shriver National Institute of Child Health and Human Development. J Pediatr 155:612–617
Hoe FM, Thornton PS, Wanner LA, Steinkrauss L, Simmons RA, Stanley CA (2006) Clinical features and insulin regulation in infants with a syndrome of prolonged neonatal hyperinsulinism. J Pediatr 148:207–212
Joseph J, Lall A, Sherratt L (2012) Guideline: hypoglycaemia of the newborn. King’s College London
Kapoor RR, Flanagan SE, James C, Shield J, Ellard S, Hussain K (2009) Hyperinsuinaemic hypoglycaemia. Arch Dis Child 94:450–457
Koh THHG, Aynsley-Green A, Tarbit M, Eyre JA (1988) Neural dysfunction during hypoglycaemia. Arch Dis Child 63:1353–1358
Kurtoǧlu S, Akcakus M, Keskin M, Ozcan A, Hussain K (2005) Severe hyperinsulinaemic hypoglycaemia in a baby born to a mother taking oral ritodrine therapy for preterm labour. Horm Res 64:61–63
March of Dimes (2011) March of dimes perinatal data center. Special care nursery admissions
McKinlay CJ, Alsweiler JM, Ansell JM, Anstice NS, Chase JG, Gamble GD, Harris DL, Jacobs RJ, Jiang Y, Paudel N, Signal M, Thompson B, Wouldes TA, Yu TY, Harding JE, CHYLD Study Group (2015) Neonatal glycemia and neurodevelopmental outcomes at 2 years. N Engl J Med 373:1507–1518
Mohamed Z, Arya VB, Hussain K (2012) Hyperinsulinaemic hypoglycaemia: genetic mechanisms, diagnosis and management. J Clin Res Pediatr Endocrinol 4:169–181
National Institute for Health and Care Excellence (2014) Intrapartum care: care of healthy women and their babies during childbirth. NICE Clin Guidel 190. Available from: http://www.nice.org.uk/guidance/index.jsp?action=folder&o=67642
Poon LCY, Volpe N, Muto B, Syngelaki A, Nicolaides KH (2012) Birthweight with gestation and maternal characteristics in live births and stillbirths. Fetal Diagn Ther 32:156–165
Stanley CA, Rozance PJ, Thornton PS, De Leon DD, Harris D, Haymond MW, Hussain K, Levitsky LL, Murad MH, Simmons RA, Sperling MA, Weinstein DA, White NH, Wolfsdorf JI (2015) Re-evaluating “transitional neonatal hypoglycemia”: mechanism and implications for management. J Pediatr 166:1520–1525.e1
Sweet CB, Grayson S, Polak M (2013) Management strategies for neonatal hypoglycemia. J Pediatr Pharmacol Ther 18:199–208
Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, Zeeman GG, Brown MA (2014) The classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHP. Pregnancy Hypertens 4:97–104
Vannucci RC, Vannucci SJ (2001) Hypoglycemic brain injury. Semin Neonatol 6:147–155
Funding
The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
KK collected the data, participated in the analysis of the data and drafted the first version of the article. TD conceived the study, participated in the analysis of the data and contributed to writing the manuscript. NK contributed the antenatal maternal data, calculated the z-scores and approved the last version of the manuscript. RK contributed to the design of the study and critically appraised the manuscript. AG supervised the project, contributed to the study design and interpretation of the results and critically revised the manuscript. All authors were involved in the preparation of the manuscript, critically reviewed the manuscript and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Infants whose parents gave informed written consent were recruited.
Additional information
Communicated by Patrick Van Reempts
Rights and permissions
About this article
Cite this article
Kozen, K., Dassios, T., Kametas, N. et al. Transient neonatal hyperinsulinaemic hypoglycaemia: perinatal predictors of length and cost of stay. Eur J Pediatr 177, 1823–1829 (2018). https://doi.org/10.1007/s00431-018-3242-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3242-7