Abstract
Clinical post-mortem radiology is a relatively new field of expertise and not common practice in most hospitals yet. With the declining numbers of autopsies and increasing demand for quality control of clinical care, post-mortem radiology can offer a solution, or at least be complementary. A working group consisting of radiologists, pathologists and other clinical medical specialists reviewed and evaluated the literature on the diagnostic value of post-mortem conventional radiography (CR), ultrasonography, computed tomography (PMCT), magnetic resonance imaging (PMMRI), and minimally invasive autopsy (MIA). Evidence tables were built and subsequently a Dutch national evidence-based guideline for post-mortem radiology was developed. We present this evaluation of the radiological modalities in a clinical post-mortem setting, including MIA, as well as the recently published Dutch guidelines for post-mortem radiology in foetuses, neonates, and children. In general, for post-mortem radiology modalities, PMMRI is the modality of choice in foetuses, neonates, and infants, whereas PMCT is advised in older children. There is a limited role for post-mortem CR and ultrasonography. In most cases, conventional autopsy will remain the diagnostic method of choice.
Conclusion: Based on a literature review and clinical expertise, an evidence-based guideline was developed for post-mortem radiology of foetal, neonatal, and paediatric patients.
What is Known: |
• Post-mortem investigations serve as a quality check for the provided health care and are important for reliable epidemiological registration. |
• Post-mortem radiology, sometimes combined with minimally invasive techniques, is considered as an adjunct or alternative to autopsy. |
What is New: |
• We present the Dutch guidelines for post-mortem radiology in foetuses, neonates and children. |
• Autopsy remains the reference standard, however minimal invasive autopsy with a skeletal survey, post-mortem computed tomography, or post-mortem magnetic resonance imaging can be complementary thereof. |
Similar content being viewed by others
Introduction
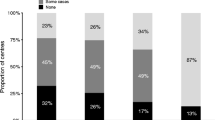
Paediatric post-mortem radiology, in addition to autopsy, is becoming widely accepted as an important component of cause of death determination [1,2,3,4,5]. The trend in declining clinical autopsy rates in adults [6,7,8,9] is also evident in the foetal and paediatric population, though higher autopsy rates of approximately 50% remain [3, 10,11,12,13]. This decline is in spite of evidence that clinical error rates persist: approximately 25% discrepancy between clinical ante-mortem diagnosis and autopsy cause of death diagnosis [3, 11, 14, 15].
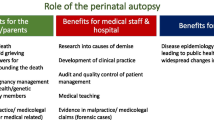
If an alternative, less- or non-invasive diagnostic method could adequately determine the cause of death, current objections to conventional autopsy (e.g. its invasiveness) could be met. Consequently, this might increase quality control and subsequently improve clinical care. Post-mortem radiology might be such an alternative diagnostic method. It can be helpful for diagnosing anatomic abnormalities, identification of syndromes, or to narrow down the differential diagnosis of genetic disorders. Consequently, it can also be useful for identifying potential siblings at risk, counselling for future pregnancies, and helping the parents in their process of grief [7, 16].
Post-mortem radiology is evolving into a subspecialty, reflected by the large increase of publications and the broad spectrum of used techniques [1]. Nevertheless, a guideline on the indications and contraindications for the use of post-mortem conventional radiography (CR), ultrasonography, computed tomography (PMCT), magnetic resonance imaging (PMMRI), and minimally invasive autopsy (MIA), was not yet available. This article provides the literature review that is the basis for the evidence-based Dutch guideline for clinical foetal, neonatal, and paediatric post-mortem radiology [17].
Materials and methods
The guideline was developed under the guidance of the Dutch knowledge institute of medical specialists. An important objective of the Dutch knowledge institute is to preserve and pool knowledge and expertise about the design and execution of quality assurance projects in the realm of specialist medical care. Medline and Embase were searched for studies comparing clinical post-mortem radiology to autopsy in foetal, neonatal, and paediatric patients from January 2000 up to January 2016, when the guideline committee started her work (Appendix 1, a further detailed search strategy is available upon request). Language selection was restricted to studies published in Dutch and English. The study selection and analysis was performed separately for the group of foetal and neonatal cases (deceased within 28 days post-partum) and for the group of paediatric cases (aged 1 month to 18 years). Studies were initially screened on title and abstract (JE, RR), and hereafter analysed on full text (EK, JE, RR). Case reports and forensic articles were excluded. Outcomes in sensitivity and specificity were mandatory. Reference lists of included studies were screened for additional relevant studies.
Methodological quality assessment of included studies was performed (EK) according to the AMSTAR checklist, PRISMA checklist, or QUADAS II, depending on the type of article [18,19,20]. The joint evidence of included articles was scored (EK) according to the Grading Recommendations Assessment, Development and Evaluation (GRADE) tool [21]. GRADE divides the quality (or certainty) of evidence and conclusions into four categories: high, medium, low or very low. A high GRADE level of evidence means that the conclusion is unlikely to change with future research, whereas in a very low GRADE level of evidence the conclusion is very precarious. In addition to the level of evidence in literature, expertise from the Dutch post-mortem imaging guideline group members was taken into account, along with preferences of bereaved relatives, costs, availability of devices, and organisational issues when formulating the guideline recommendations.
Results
Study identification
The literature search resulted in 268 eligible articles for foetuses and neonates and 415 articles for paediatric studies. After title, abstract, and full-text selection 14 foetal-neonatal articles and 9 paediatric studies remained (Figs. 1 and 2). Studies on CR, PMCT, PMMRI, and MIA were included, other post-mortem imaging methods (e.g. post-mortem ultrasound) did not meet the inclusion criteria.
Study quality
Both in foetal and neonatal patients, as well as in paediatric patients, the GRADE evidence for post-mortem CR, PMCT, and MIA was graded as low because few studies, with few patients included, have been performed. More studies were published on PMMRI, yet the evidence for PMMRI was also graded as low in both groups, because almost all results were based on the Magnetic Resonance Imaging Autopsy Study (MaRIAS). This study was performed in a specialised setting with well-trained specialists and a relatively low number of patients.
Post-mortem conventional radiography (CR)
One article was included from the literature review on post-mortem CR in foetal and neonatal patients. No articles on post-mortem CR of paediatric patients met the inclusion criteria.
Foetal-neonatal
A clinical, foetal post-mortem skeletal survey consists mainly of a whole-body radiograph; a ‘babygram’ (Fig. 3). A study of 377 foetal post-mortem skeletal surveys showed a 100% sensitivity and 97% specificity for detection of skeletal abnormalities compared to diagnosis based on autopsy, genetics, and prenatal investigations [22]. However, the number of diagnostic abnormalities in this population was limited. The authors concluded that there is no indication for a foetal post-mortem skeletal survey in cases without previous suspicion of skeletal abnormalities on prenatal ultrasound or during post-mortem external inspection. If a foetal ‘babygram’ is obtained, it should preferably be done using a high resolution ‘cabinet radiography’ system. If this is not available, the use of a mammography system is advised.
Example of a diagnostic babygram. This pregnancy was terminated at 22 weeks of gestation because of micromelia on prenatal 2nd trimester ultrasound, suspected to be a skeletal dysplasia. The babygram showed skeletal abnormalities with shortened ribs, metaphyseal flaring (1) and shortened and bowed long bones (2). Histology revealed abnormalities in the liver, kidneys, lungs, bone and cartilage compatible with ciliopathy with major skeletal involvement. Jeune syndrome is the most likely diagnosis
Post-mortem computed tomography (PMCT)
One study was included on the sensitivity and specificity of PMCT for both foetal-neonatal and paediatric patients, and an additional article on paediatric patients (Table 1).
Foetal-neonatal
PMCT and PMMRI were both compared to autopsy, and to each other in 53 foetuses, finding 40% of the PMCT’s non-diagnostic in foetuses below 24 weeks of gestation (n = 35) compared to 11% of PMMRI’s, with twice as many correct diagnoses on PMMRI compared to PMCT (10 vs. 5, p < 0.005) [23]. In foetuses above 24 weeks of gestation (n = 18), 22% of PMCT’s were non-diagnostic, compared to 0% of PMMRI’s (p < 0.005). In cases where radiology was diagnostic, both PMCT and PMMRI showed a 50% sensitivity and 100% specificity for main diagnosis or cause of death. Also, no significant differences were observed for identification of pathological lesions in individual organ systems, irrespective of contribution to death.
Paediatric
Sensitivity of PMCT for cause of death determination depends on the type of pathology and age of the child [23, 24]. The same study as for foetuses and neonates, included 29 children with an average age of 6.9 months (range 1 day–16 years) [23]. In this small group, both PMCT and PMMRI showed a 50% sensitivity and 100% specificity for the main diagnosis or cause of death. The overall concordance was slightly lower for PMCT than PMMR (59.4% vs. 62.8%). In another study with 12 children under the age of 1 year, PMCT’s of the lungs were non-diagnostic in 75% prior to post-mortem ventilation, compared to 0% of PMCT’s with ventilation [24]. A 100% sensitivity and 63% specificity were found for the detection of abnormal lung areas with ventilated PMCT. Therefore, ventilated PMCT could be used to improve identification of abnormal areas of the lungs.
Post-mortem magnetic resonance imaging (PMMRI)
Seven articles were included on the diagnostic performance of PMMRI in foetuses and neonates, along with five articles on paediatric patients (Table 2). The majority of these studies reported on the Magnetic Resonance Imaging Autopsy Study (MaRIAS) (sub)population [23, 25, 27,28,29,30]. MaRIAS is a large, 3.5 year, double-blind prospective study in 277 foetuses (185 foetuses of 24 weeks gestation or less and 92 foetuses of 24 weeks gestation or more) and 123 children (42 neonates, 53 infants up to 1 year of age, and 28 children above 1 year of age), which compared the diagnostic accuracy of 1.5 T PMMRI to conventional autopsy [31, 32].
Foetal-neonatal
Before the MaRIAS study, a systematic review, investigating the diagnostic accuracy of PMMRI, included five studies on foetuses [33]. In four of those five studies, a complete autopsy was used as the reference standard. The included studies were of moderate quality as the groups were small and the population heterogeneity large. There was a pooled sensitivity of 69% (95%CI 56–80) and a pooled specificity of 95% (95%CI 88–98) for detection of clinically significant abnormalities.
The MaRIAS study reported high sensitivities (82–100%) and high specificities (93–97%) for both major and minor cardiac pathology, as well as for structural and non-structural heart disease in foetuses below and above 24 weeks of gestation [25]. Votino et al. (2012) compared high-field PMMRI (9.4 T) to lower-field PMMRI (1.5 T and 3.0 T) and stereomicroscopic autopsy (MIA) [26]. In contrast to lower-field PMMRI, the heart situs, four-chamber view and outflow tracts could be visualised in all foetuses with 9.4 T, irrespective of gestational age. High-field PMMRI identified seven out of eight cases with major congenital heart disease. In foetuses below and above 24 weeks of gestation, MaRIAS reported low sensitivities of 30 and 38% and high specificities of 96 and 88% respectively for the detection of non-cardiac, thoracic abnormalities with 1.5 T [27]. Based on these results and the reasonable negative predictive values of approximately 85%, PMMRI appeared to be more useful in the exclusion of thoracic abnormalities, rather than in its identification. Detection of pulmonary tract infection and diffuse alveolar haemorrhage was difficult, whereas PMMRI was most sensitive for detection of anatomical abnormalities, including pleural effusions and lung hypoplasia.
Based on MaRIAS, very high sensitivities (80–100%) and specificities (87–100%) were found for the detection of brain malformations (Fig. 4) and minor and major intracranial bleedings [28]. A lower sensitivity of 30% was found for the detection of hypoxic-ischaemic brain injury in foetuses above 24 weeks of gestation. Furthermore, cerebral PMMRI provided clinically important information in 23 out of 43 foetuses in whom neuropathological examination was non-diagnostic due to maceration.
a, b Example of abnormalities of the central nervous system diagnosed at PMMRI in a female foetus. This pregnancy was terminated at 23 weeks of gestation because of corpus callosum agenesis (1), an interhemispheric cyst (2) and fossa posterior anomalies on prenatal 2nd trimester ultrasound, which were confirmed by PMMRI and/or conventional autopsy. A non-cystic dilatation of the fourth ventricle (3) was found on PMMRI along with the additional findings of a left choroid plexus cyst (4) and polymicrogyria (5). Furthermore, autopsy diagnosed a choroid plexus papilloma in the left lateral ventricle, but the additional finding of polymicrogyria (5) on PMMRI revealed Aicardi syndrome as the most likely diagnosis. a Axial. b Sagittal
PMMRI showed moderate sensitivities of 77 and 65% for abdominal abnormalities in foetuses below and above 24 weeks gestation, respectively [29]. Diagnostic accuracy was variable per organ system, with the highest sensitivity for renal abnormalities (18/21 = 86%) and the lowest for intestinal abnormalities (2/7 = 29%). In addition, MaRIAS reported moderate and very low sensitivities for detection of musculoskeletal abnormalities in foetuses below and over 24 weeks of gestation, respectively 69 and 17% [30].
Paediatric
MaRIAS reported a 100% sensitivity and 98% specificity for major and minor structural heart defects in neonates and children with 1.5 T PMMRI [25]. A substantial lower sensitivity of 62% was observed for any cardiac pathology, both structural and non-structural. Identification of non-cardiac, thoracic abnormalities was difficult, especially in case of pneumonia [27]. Sensitivities of 100% and specificities of 98–100% were reported for the detection of brain malformations and minor and major intracranial haemorrhages [28]. In contrast to foetuses, PMMRI showed a high sensitivity (93%) for ischaemic brain injury in neonates and children. Just as in foetuses, PMMRI showed a moderate sensitivity (71%) and high specificity (87%) for abdominal abnormalities [29]. The sensitivity for skeletal abnormalities was poor (31%) [30].
Minimal invasive autopsy (MIA)
One article included from the literature search reported on MIA in both foetal-neonatal and paediatric patients (MaRIAS) [31]. This study compared the diagnostic accuracy of MIA to conventional autopsy. MIA consisted of PMMRI, combined with other post-mortem radiology, genetic and metabolic tests (ante-mortem and post-mortem blood sampling), a review of the clinical history, external examination, and examination of placental tissue, if available. No foetal-neonatal or paediatric studies combining PMMRI or PMCT with tissue biopsies or angiography met the inclusion criteria.
Foetal-neonatal
Both a high sensitivity (100%, 95%CI 97–100) and high specificity (98%, 95%CI 88–100) were reported for the detection of major pathological abnormalities or cause of death in foetuses below 24 weeks of gestation [31]. In foetuses above 24 weeks of gestation, sensitivity and specificity were also high (respectively 96%, 95%CI 86–99, and 95%, 95%CI 84–99). Moreover, MIA had a higher sensitivity and specificity compared to PMMRI alone. In both groups of foetuses, the sensitivity and specificity for detection of non-infectious pathologies were above 95%. Sensitivity for infectious pathologies was with 80% (95%CI 38–96) lower in foetuses above 24 weeks of gestation than in foetuses below 24 weeks of gestation (100%, 95%CI 92–100).
Paediatric
A 69% sensitivity (95%CI 58–78) and 93% specificity (95%CI 81–98) were found for major pathological abnormalities or cause of death in children [31]. Sensitivities of respectively 94% (95%CI 84–98) and 27% (95%CI 14–44) were reported for the detection of non-infectious and infectious pathologies, with specificities of respectively 96% (95%CI 89–99) and 100% (95%CI 96–100). Pneumonia and myocarditis were the main undetected abnormalities. This study showed an increase in the diagnostic accuracy of post-mortem radiology when PMMRI was extended with additional (minimal-invasive, genetic and metabolic) tests or examination of placental tissue. Like in the foetal patient group, MIA showed better results than PMMRI alone.
Dutch post-mortem imaging guideline
The Dutch guideline working group developed an evidence and practice-based flowchart for post-mortem radiology in non-forensic foetal and neonatal deaths (Fig. 5), and paediatric deaths (Fig. 6). It must be emphasised that, based on the literature, due to the low GRADE level of evidence, post-mortem radiology without clinical autopsy should be considered as insufficient for best-practice post-mortem diagnosis.
Flowchart for post-mortem radiology in foetal and neonatal deaths*. * adapted from the Dutch guideline for clinical foetal, neonatal, and paediatric post-mortem radiology [17]. GA: gestational age. US: ultrasonography. The ‘routine 2nd trimester ultrasound’ is a standard prenatal US in all growing foetuses. The ‘US for foetal death determination’ is a second, separate antenatal US by the gynaecologist in order to confirm death. PMMRI: post-mortem magnetic resonance imaging. CNS: central nervous system. NODOK:: The Dutch ‘Nader Onderzoek naar de DoodsOorzaak van Kinderen’ (i.e. ‘further examination of cause of death in children’) procedure is a stepwise approach to investigate the cause of death in children with an assumed natural unexpected and unexplained death [34]
Flowchart for post-mortem radiology in paediatric deaths*. * adapted from the Dutch guideline for clinical foetal, neonatal, and paediatric post-mortem radiology [17]. PMMRI: post-mortem magnetic resonance imaging. PMCT: post-mortem computed tomography. NODOK: The Dutch ‘Nader Onderzoek naar de DoodsOorzaak van Kinderen’ (i.e. ‘further examination of cause of death in children’) procedure is a stepwise approach to investigate the cause of death in children with an assumed natural unexpected and unexplained death [34]
Discussion
Autopsy is traditionally considered as the gold standard for post-mortem diagnoses and quality assessment of provided health care. However, the declining autopsy rates of the last decennia result in decreasing expertise, especially in foetal-neonatal and paediatric cases where mortality rates are low. Although autopsy remains the preferred diagnostic method in foetal, neonatal, and paediatric death, post-mortem radiology, after consent, can be used in adjunct to autopsy or as an alternative in cases without consent for conventional autopsy. In general, PMMRI is advised in foetuses, neonates, and young children, as PMMRI has a higher soft-tissue contrast compared to PMCT. The small body size enables high-resolution whole-body imaging in a reasonable amount of time. The limited value of PMCT in young children is illustrated in a study of 54 children (median age 1.0 years old, range 2 days–17.9 years) who died of an assumed natural cause, where PMCT could establish the cause of death in mere 12.9% [34]. In older children, just as in adults, PMCT is the preferred modality because of the lack of evidence of superiority of PMMRI over PMCT, its high availability, lower costs, and reduced scan time compared to PMMRI. With the limited amount of studies in children, it is not possible to be more specific about the age range where PMCT and PMMRI have equal diagnostic performances. The Dutch guideline for paediatric post-mortem radiology describes PMCT as a possible adjunct to PMMRI and autopsy, in children of 2 to 5 years of age (Fig. 7). Furthermore, either PMCT or PMMRI is advised in children of 5 years or older, depending on the type of pathology expected. Given the limited amount of evidence, we would like to underline that, especially in infants and children, post-mortem imaging should be seen as an adjunct to the autopsy and not as a replacement. The cut-off age levels were the results of combined expert opinion, this as there is insufficient evidence to define a set cut-off age level.
a, b Example of a PMCT (a) of a 4-year-old child with an unexpected and unexplained but assumed natural cause of death. Cardiopulmonary resuscitation was performed but not successful. PMCT and PMMRI showed a volvulus of the ileum around its mesentery (whirl sign) (arrow). Ischemic haemorrhagic volvulus of the ileum was confirmed by autopsy (b) as the cause of death
No eligible paediatric studies on post-mortem CR were included. Nevertheless, in deceased children up to 4 years of age, a skeletal survey (consisting of 20–30 images) is advised to detect fractures, potentially caused by non-accidental injury [35,36,37,38,39]. In deceased children of 5 years or older, with possible child abuse, conventional radiographs of the areas of interest are advised on a low-threshold basis. This is despite a lack of evidence for the supplementary value of a skeletal survey or conventional radiographs in natural causes of death. In a study in 542 perinatal deaths (from 16 weeks gestation to 1 week after birth), the diagnostic value was very limited: 30% had abnormal radiographs, of which only 0.9% were of diagnostic importance for establishing the cause of death [40].
Although ultrasound did not meet the inclusion criteria for the guideline it is a technique that could be considered in selected cases where parents do not approve the use of PMCT or PMMRI [41,42,43]. Due to open sutures and absence of inhaled air, the brain and lungs can be examined by ultrasonography in cases of foetal demise [44]. In 88 foetuses of 11–40 weeks of gestation sensitivities of 91, 88, and 87% and specificities of respectively 90, 92, and 95% were reported with ultrasound for respectively brain, thoracic and abdominal anomalies [45].
To meet the demand for less invasive alternatives to autopsy [46, 47], as well as a high diagnostic performance, it is likely that a combination of imaging and minimal invasive tissue acquisition will be increasingly used in future. Other minimal invasive techniques such as genetic and metabolic testing as well as virology and microbiology sampling can be added on indication. The more post-mortem radiology is expanded with minimally invasive investigations, the higher the diagnostic yield will be; the border area of a minimal invasive radiological test and a restricted autopsy demands for close collaboration between these two specialities. Furthermore, the diagnostic performance of post-mortem radiology will increase by improvements of diagnostic techniques such a high-field PMMRI (Fig. 8), post-mortem angiography, and post-mortem ventilation [24, 48, 49]. Non- or minimally invasive autopsy evokes much less objections from parents compared to conventional autopsy, resulting in overall increasing post-mortem investigation rates [46, 47]. Hence, post-mortem radiology can increase post-mortem investigation rates, and subsequently improve family counselling and quality control of clinical diagnosis.
As post-mortem radiology is a relatively new subspecialty, images should be evaluated by an experienced radiologist. This should preferably be a paediatric radiologist who is familiar with normal post-mortem changes, which to the untrained eye can mimic pathologic abnormalities (Fig. 9) [50, 51]. Therefore, it is advised for non-specialised centres to ask assistance from experienced radiologists.
To conclude, post-mortem radiology without clinical autopsy is yet considered as insufficient to establish the cause of death, due to the low GRADE level of evidence. Autopsy is therefore still regarded as the reference standard [23]. Post-mortem radiology, especially as part of a MIA procedure, is considered a useful adjunct or valuable alternative in cases where autopsy is not performed. In general, neonatologists or paediatricians will be the referring physicians and as such they will be the ones obtaining parental informed consent. Therefore, it is imperative that they are aware of the advantages and limitations of post-mortem imaging. A multidisciplinary approach including clinicians, radiologists, and pathologists seems most beneficial. At present, PMMRI is the imaging modality of choice in foetuses, neonates, and young children, whereas PMCT is preferred in in older children.
Abbreviations
- CR:
-
Conventional radiography
- GRADE:
-
Grading Recommendations Assessment, Development and Evaluation
- MaRIAS:
-
Magnetic Resonance Imaging Autopsy Study
- MIA:
-
Minimally invasive autopsy
- PMCT:
-
Post-mortem computed tomography
- PMMRI:
-
Post-mortem magnetic resonance imaging
References
Baglivo M, Winklhofer S, Hatch GM, Ampanozi G, Thali MJ, Ruder TD (2013) The rise of forensic and post-mortem radiology—analysis of the literature between the year 2000 and 2011. J Forensic Radiol Imaging 1(1):3–9. https://doi.org/10.1016/j.jofri.2012.10.003
Flach PM, Thali MJ, Germerott T (2014) Times have changed! Forensic radiology--a new challenge for radiology and forensic pathology. AJR Am J Roentgenol 202(4):W325–W334. https://doi.org/10.2214/ajr.12.10283
Gordijn SJ, Erwich JJ, Khong TY (2002) Value of the perinatal autopsy: critique. Pediatr Dev Pathol 5(5):480–488. https://doi.org/10.1007/s10024-002-0008-y
Lawn JE, Cousens S, Zupan J, Team LNSS (2005) 4 million neonatal deaths: when? Where? Why? Lancet 365(9462):891–900. https://doi.org/10.1016/S0140-6736(05)71048-5
Nijkamp JW, Sebire NJ, Bouman K, Korteweg FJ, Erwich JJHM, Gordijn SJ (2017) Perinatal death investigations: what is current practice? Semin Fetal Neonatal Med 22(3):167–175. https://doi.org/10.1016/j.siny.2017.02.005
Blokker BM, Wagensveld IM, Weustink AC, Oosterhuis JW, Hunink MG (2016) Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: a systematic review. Eur Radiol 26(4):1159–1179. https://doi.org/10.1007/s00330-015-3908-8
Burton JL, Underwood J (2007) Clinical, educational, and epidemiological value of autopsy. Lancet 369(9571):1471–1480. https://doi.org/10.1016/s0140-6736(07)60376-6
Hutchinson JC, Arthurs OJ, Ashworth MT, Ramsey AT, Mifsud W, Lombardi CM, Sebire NJ (2016) Clinical utility of postmortem microcomputed tomography of the fetal heart: diagnostic imaging vs macroscopic dissection. Ultrasound Obstet Gynecol 47(1):58–64. https://doi.org/10.1002/uog.15764
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, Maes A, van Rijn RR (2013) The value of post-mortem CT in neonaticide in case of severe decomposition: description of 12 cases. Forensic Sci Int 233(1–3):298–303. https://doi.org/10.1016/j.forsciint.2013.09.023
Adappa R, Paranjothy S, Roberts Z, Cartlidge PH (2007) Perinatal and infant autopsy. Arch Dis Child Fetal Neonatal Ed 92(1):F49–F50. https://doi.org/10.1136/adc.2005.091447
Brodlie M, Laing IA, Keeling JW, McKenzie KJ (2002) Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ 324(7340):761–763. https://doi.org/10.1136/bmj.324.7340.761
Hickey L, Murphy A, Devaney D, Gillan J, Clarke T (2012) The value of neonatal autopsy. Neonatology 101(1):68–73. https://doi.org/10.1159/000329094
Khong TY (1996) A review of perinatal autopsy rates worldwide, 1960s to 1990s. Paediatr Perinat Epidemiol 10(1):97–105; discussion 106–109. https://doi.org/10.1111/j.1365-3016.1996.tb00030.x
Custer JW, Winters BD, Goode V, Robinson KA, Yang T, Pronovost PJ, Newman-Toker DE (2015) Diagnostic errors in the pediatric and neonatal ICU: a systematic review. Pediatr Crit Care Med 16(1):29–36. https://doi.org/10.1097/pcc.0000000000000274
Shojania KG, Burton EC, McDonald KM, Goldman L (2003) Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 289(21):2849–2856. https://doi.org/10.1001/jama.289.21.2849
Rankin J, Wright C, Lind T (2002) Cross sectional survey of parents’ experience and views of the postmortem examination. BMJ 324(7341):816–818. https://doi.org/10.1136/bmj.324.7341.816
Knowledge Institute of Medical Specialists (2017) Klinische postmortem radiologie. https://richtlijnendatabase.nl/. Accessed 2017
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7(1):10. https://doi.org/10.1186/1471-2288-7-10
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, Liberati A, O'Connell D, Oxman AD, Phillips B (2004) Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches the GRADE working group. BMC Health Serv Res 4(1):38. https://doi.org/10.1186/1472-6963-4-38
Kamphuis-van Ulzen K, Koopmanschap DHJLM, Marcelis CLM, van Vugt JMG, Klein WM (2016) When is a post-mortem skeletal survey of the fetus indicated, and when not? J Matern Fetal Neonatal Med 29(6):991–997. https://doi.org/10.3109/14767058.2015.1029913
Arthurs OJ, Guy A, Thayyil S, Wade A, Jones R, Norman W, Scott R, Robertson NJ, Jacques TS, Chong WK, Gunny R, Saunders D, Olsen OE, Owens CM, Offiah AC, Chitty LS, Taylor AM, Sebire NJ (2016) Comparison of diagnostic performance for perinatal and paediatric post-mortem imaging: CT versus MRI. Eur Radiol 26(7):2327–2336. https://doi.org/10.1007/s00330-015-4057-9
Arthurs OJ, Guy A, Kiho L, Sebire NJ (2015) Ventilated postmortem computed tomography in children: feasibility and initial experience. Int J Legal Med 129(5):1113–1120. https://doi.org/10.1007/s00414-015-1189-z
Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RJ, Wade A, Chitty LS, Robertson N, Thayyil S (2014) Postmortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation 129(19):1937–1944. https://doi.org/10.1161/circulationaha.113.005641
Votino C, Jani J, Verhoye M, Bessieres B, Fierens Y, Segers V, Vorsselmans A, Kang X, Cos T, Foulon W, De Mey J, Cannie M (2012) Postmortem examination of human fetal hearts at or below 20 weeks’ gestation: a comparison of high-field MRI at 9.4 T with lower-field MRI magnets and stereomicroscopic autopsy. Ultrasound Obstet Gynecol 40(4):437–444. https://doi.org/10.1002/uog.11191
Arthurs OJ, Thayyil S, Olsen OE, Addison S, Wade A, Jones R, Norman W, Scott RJ, Robertson NJ, Taylor AM, Chitty LS, Sebire NJ, Owens CM (2014) Diagnostic accuracy of post-mortem MRI for thoracic abnormalities in fetuses and children. Eur Radiol 24(11):2876–2884. https://doi.org/10.1007/s00330-014-3313-8
Arthurs OJ, Thayyil S, Pauliah SS, Jacques TS, Chong WK, Gunny R, Saunders D, Addison S, Lally P, Cady E, Jones R, Norman W, Scott R, Robertson NJ, Wade A, Chitty L, Taylor AM, Sebire NJ (2015) Diagnostic accuracy and limitations of post-mortem MRI for neurological abnormalities in fetuses and children. Clin Radiol 70(8):872–880. https://doi.org/10.1016/j.crad.2015.04.008
Arthurs OJ, Thayyil S, Owens CM, Olsen OE, Wade A, Addison S, Jones R, Norman W, Scott RJ, Robertson NJ, Taylor AM, Chitty LS, Sebire NJ (2015) Diagnostic accuracy of post mortem MRI for abdominal abnormalities in foetuses and children. Eur J Radiol 84(3):474–481. https://doi.org/10.1016/j.ejrad.2014.11.030
Arthurs OJ, Thayyil S, Addison S, Wade A, Jones R, Norman W, Scott R, Robertson NJ, Chitty LS, Taylor AM, Sebire NJ, Offiah AC (2014) Diagnostic accuracy of postmortem MRI for musculoskeletal abnormalities in fetuses and children. Prenat Diagn 34(13):1254–1261. https://doi.org/10.1002/pd.4460
Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O, Gunny RS, Offiah AC, Owens CM, Saunders DE, Scott RJ, Jones R, Norman W, Addison S, Bainbridge A, Cady EB, Vita ED, Robertson NJ, Taylor AM (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 382(9888):223–233. https://doi.org/10.1016/s0140-6736(13)60134-8
Thayyil S, Sebire NJ, Chitty LS, Wade A, Olsen O, Gunny RS, Offiah A, Saunders DE, Owens CM, Chong WK, Robertson NJ, Taylor AM (2011) Post mortem magnetic resonance imaging in the fetus, infant and child: a comparative study with conventional autopsy (MaRIAS protocol). BMC Pediatr 11:120. https://doi.org/10.1186/1471-2431-11-120
Thayyil S, Chandrasekaran M, Chitty LS, Wade A, Skordis-Worrall J, Bennett-Britton I, Cohen M, Withby E, Sebire NJ, Robertson NJ, Taylor AM (2010) Diagnostic accuracy of post-mortem magnetic resonance imaging in fetuses, children and adults: a systematic review. Eur J Radiol 75(1):e142–e148. https://doi.org/10.1016/j.ejrad.2009.10.007
van Rijn RR, Beek EJ, van de Putte EM, Teeuw AH, Nikkels PG, Duijst WL, Nievelstein R-JA, Group DN (2017) The value of postmortem computed tomography in paediatric natural cause of death: a Dutch observational study. Pediatr Radiol 47(11):1514–1522
Belfer RA, Klein BL, Orr L (2001) Use of the skeletal survey in the evaluation of child maltreatment. Am J Emerg Med 19(2):122–124. https://doi.org/10.1053/ajem.2001.21345
Dubbins P, Price J, Johnson K, Maguire SA, Wall M, Jaspan T, Hobbs C, Stoodley N, Chapman S, Kemp AM (2008) Standards for radiological investigations of suspected non-accidental injury. Royal College of Paediatrics and Child Health, London
Kleinman PK, Morris NB, Makris J, Moles RL, Kleinman PL (2013) Yield of radiographic skeletal surveys for detection of hand, foot, and spine fractures in suspected child abuse. AJR Am J Roentgenol 200(3):641–644. https://doi.org/10.2214/ajr.12.8878
van Rijn RR, Sieswerda-Hoogendoorn T (2012) Educational paper: imaging child abuse: the bare bones. Eur J Pediatr 171(2):215–224. https://doi.org/10.1007/s00431-011-1499-1
Wootton-Gorges SL, Soares BP, Alazraki AL, Anupindi SA, Blount JP, Booth TN, Dempsey ME, Falcone RA Jr, Hayes LL, Kulkarni AV, Partap S, Rigsby CK, Ryan ME, Safdar NM, Trout AT, Widmann RF, Karmazyn BK, Palasis S (2017) ACR appropriateness criteria(R) suspected physical abuse-child. J Am Coll Radiol 14(5s):S338–s349. https://doi.org/10.1016/j.jacr.2017.01.036
Olsen ØE, Espeland A, Maartmann-Moe H, Lachman R, Rosendahl K (2003) Diagnostic value of radiography in cases of perinatal death: a population based study. Arch Dis Child Fetal Neonatal Ed 88(6):F521–F524. https://doi.org/10.1136/fn.88.6.F521
Charlier P, Chaillot PF, Watier L, Menetrier M, Carlier R, Cavard S, Herve C, de la Grandmaison GL, Huynh-Charlier I (2013) Is post-mortem ultrasonography a useful tool for forensic purposes? Med Sci Law 53(4):227–234. https://doi.org/10.1177/0025802413479946
Prodhomme O, Baud C, Saguintaah M, Béchard-Sevette N, Bolivar J, David S, Taleb-Arrada I, Couture A (2015) Comparison of postmortem ultrasound and X-ray with autopsy in fetal death: retrospective study of 169 cases. J Forensic Radiol Imaging 3(2):120–130. https://doi.org/10.1016/j.jofri.2015.04.002
Uchigasaki S, Oesterhelweg L, Gehl A, Sperhake JP, Puschel K, Oshida S, Nemoto N (2004) Application of compact ultrasound imaging device to postmortem diagnosis. Forensic Sci Int 140(1):33–41. https://doi.org/10.1016/j.forsciint.2003.11.029
Prodhomme O, Baud C, Saguintaah M, Béchard-Sevette N, Bolivar J, David S, Taleb-Arrada I, Couture A (2015) Principles of fetal postmortem ultrasound: a personal review. J Forensic Radiol Imaging 3(1):12–15. https://doi.org/10.1016/j.jofri.2015.01.008
Votino C, Bessieres B, Segers V, Kadhim H, Razavi F, Condorelli M, Votino R, D'Ambrosio V, Cos T (2014) Minimally invasive fetal autopsy using three-dimensional ultrasound: a feasibility study. Ultrasound Obstet Gynecol. https://doi.org/10.1002/uog.14642
Cannie M, Votino C, Moerman P, Vanheste R, Segers V, Van Berkel K, Hanssens M, Kang X, Cos T, Kir M, Balepa L, Divano L, Foulon W, De Mey J, Jani J (2012) Acceptance, reliability and confidence of diagnosis of fetal and neonatal virtuopsy compared with conventional autopsy: a prospective study. Ultrasound Obstet Gynecol 39(6):659–665. https://doi.org/10.1002/uog.10079
Kang X, Cos T, Guizani M, Cannie MM, Segers V, Jani JC (2014) Parental acceptance of minimally invasive fetal and neonatal autopsy compared with conventional autopsy. Prenat Diagn 34(11):1106–1110. https://doi.org/10.1002/pd.4435
Barber JL, Sebire NJ, Chitty LS, Taylor AM, Arthurs OJ (2015) Lung aeration on post-mortem magnetic resonance imaging is a useful marker of live birth versus stillbirth. Int J Legal Med 129(3):531–536. https://doi.org/10.1007/s00414-014-1125-7
Thayyil S, Cleary JO, Sebire NJ, Scott RJ, Chong K, Gunny R, Owens CM, Olsen OE, Offiah AC, Parks HG, Chitty LS, Price AN, Yousry TA, Robertson NJ, Lythgoe MF, Taylor AM (2009) Post-mortem examination of human fetuses: a comparison of whole-body high-field MRI at 9.4 T with conventional MRI and invasive autopsy. Lancet 374(9688):467–475. https://doi.org/10.1016/s0140-6736(09)60913-2
Klein WM, Bosboom DG, Koopmanschap DH, Nievelstein RA, Nikkels PG, van Rijn RR (2015) Normal pediatric postmortem CT appearances. Pediatr Radiol 45(4):517–526. https://doi.org/10.1007/s00247-014-3258-8
Offiah CE, Dean J (2016) Post-mortem CT and MRI: appropriate post-mortem imaging appearances and changes related to cardiopulmonary resuscitation. Br J Radiol 89(1058):20150851. https://doi.org/10.1259/bjr.20150851
Besselaar AT, Sakkers RJB, Schuppers HA, Witbreuk MMEH, Zeegers EVCM, Visser JD, Boekestijn RA, Margés SD, Van der Steen MCM, Burger KNJ (2017) Guideline on the diagnosis and treatment of primary idiopathic clubfoot. Acta Orthop 88(3):305–309. https://doi.org/10.1080/17453674.2017.1294416
OMS, Orde van Medisch Specialisten (2011). Eindrapport Medisch Specialistische Richtlijnen 2.0. Available from: www.kwaliteitskoepel.nl/kwaliteitsbibliotheek/leidraden/eindrapport-medisch-specialistische-richtlijnen-2-0.html.
Brouwers M, Kho ME, Browman GP, Cluzeau F, Feder G, Fervers B, Hanna S, Makarski J, on behalf of the AGREE Next Steps Consortium (2010) AGREE II: Advancing guideline development, reporting and evaluation in healthcare. Can Med Assoc J 182:E839–E842. https://doi.org/10.1503/cmaj.090449
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, de Beer H et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Schünemann H, Brożek J, Guyatt G, Oxman A, editors. (2013) GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group. Available from www.guidelinedevelopment.org/handbook.
Schünemann HJ, Wiercioch W, Etxeandia I, Falavigna M, Santesso N, Mustafa R, Ventresca M, Brignardello-Petersen R, Laisaar KT, Kowalski S, Baldeh T, Zhang Y, Raid U, Neumann I, Norris SL, Thornton J, Harbour R, Treweek S, Guyatt G, Alonso-Coello P, Reinap M, Brozek J, Oxman A, Akl EA (2014) Guidelines 2.0: systematic development of a comprehensive checklist for a successful guideline enterprise. CMAJ 186(3):E123–E142. https://doi.org/10.1503/cmaj.131237
Acknowledgements
M.M.J. Ploegmakers (Knowledge Institute of Medical Specialists, Utrecht, The Netherlands), M. Wessels (Knowledge Institute of Medical Specialists, Utrecht, The Netherlands), I.M.B. Russel (Department of Paediatrics, University Medical Center Utrecht, the Netherlands), M. ten Horn (Patientfederation, Utrecht, the Netherlands), R. Kranenburg (Patientfederation, Utrecht, the Netherlands), D. van Meersbergen (The Royal Dutch Medical Association (KNMG), the Netherlands).
Funding
The development of the Dutch postmortem imaging guideline was funded by the Quality Foundation of the Dutch Medical Specialists (SKMS).
Author information
Authors and Affiliations
Consortia
Contributions
L.S. reported on the literature review and Dutch guideline for postmortem radiology/wrote the submitted manuscript, and provided tables and figures for the manuscript.
M.V. reported on the literature review and Dutch guideline for postmortem radiology/wrote the submitted manuscript, and provided tables and figures for the manuscript.
E.K. analysed appropriate articles on full text, performed methodological quality assessment of included studies, and assessed the joint evidence of included articles according to the GRADE tool.
J.J.E. screened studies on title, abstract, and full text for the Dutch guideline development, and developed the Dutch guideline for clinical postmortem radiology.
P.K. developed the Dutch guideline for clinical postmortem radiology.
P.N. developed the Dutch guideline for clinical postmortem radiology.
R.R. screened studies on title, abstract, and full text for the Dutch guideline development, and developed the Dutch guideline for clinical postmortem radiology.
W.K. chaired the Dutch post-mortem imaging guideline group and developed the Dutch guideline for clinical postmortem radiology.
All authors contributed to the interpretation of the data and revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Dutch post-mortem imaging guideline group
Apart from the named authors, the following persons are the collaborators in the Dutch post-mortem imaging guideline group: W.L.J.M. Duijst (GGD IJsselland Zwolle, the Netherlands, and Maastricht University, the Netherlands), P.A.M. Hofman (Department of Radiology, Maastricht University Medical Center, the Netherlands), J.J.F. Kroll (Department of Radiology, Maastricht University Medical Center, the Netherlands), N.S. Renken (Department of Radiology, Reinier de Graaf Gasthuis, Delft, the Netherlands), Y.O. Rosier (NVMBR Utrecht, the Netherlands), C.I.E. Scheeren (Department of Intensive Care, Zuyderland Heerlen, the Netherlands), S.J. Stomp (GGD, Amsterdam, the Netherlands), P. van der Valk (Department of Pathology, Free University Medical Center, Amsterdam, the Netherlands).
Additional information
Communicated by Piet Leroy
Appendix 1. Materials and methods
Appendix 1. Materials and methods
Text adjusted from Acta Orthopedica (Besselaar et al [52]; PubMed PMID: 28266239).
Guideline working group
This guideline was developed and sponsored by the Radiological Society of the Netherlands (NVvR), using governmental funding from the Stichting Kwaliteitsgelden Medisch Specialisten in the Netherlands (SKMS, Quality foundation of the Dutch Federation of Medical Specialists). The early preparative phase started July 2015 and the guideline will officially be authorized by the Radiological Society of the Netherlands at the end of 2017. The working group had nine in-person meetings (between September 2015 and September 2017) and otherwise communicated by phone and email. Decisions were made by consensus. At the start of guideline development, all working group members completed conflict of interest forms.
Target group and aims
This guideline was developed for Dutch radiologists concerned with postmortem radiology, and other medical specialists involved in postmortem diagnostics. The main purpose of the guideline is to provide best possible care to fetuses or neonates, children and their relatives in a postmortem radiology setting, by informing optimal treatment decisions, and reduce unwarranted variation in the delivery of postmortem diagnostic care.
Methodology
The guideline was developed in agreement with the criteria set by the advisory committee on guideline development of the Federation of Medical Specialists in the Netherlands (Medisch Specialistische Richtlijnen 2.0; OMS [53], which are based on the AGREE II instrument (Brouwers [54]; www.agreetrust.org). The guideline was developed using an evidence-based approach endorsing GRADE methodology, and meeting all criteria of AGREE-II. Grading of Recommendations Assessment, Development and Evaluation (GRADE) is a systematic approach for synthesizing evidence and grading of recommendations offering transparency at each stage of the guideline development [55, 56].
The guideline development process involves a number of phases, a preparative phase, development phase, commentary phase, and authorization phase. After authorization, the guideline has to be disseminated and implemented, and uptake and use have to be evaluated. Finally, the guideline has to be kept up-to-date. Each phase involves a number of practical steps (see Schünemann [57]).
A methodologist together with the chairman of the working group drafted a concept list of key issues which was extensively discussed in the working group. The selected (high priority) issues were translated into carefully formulated clinical questions, defining patient/problem, intervention, and prioritizing the outcomes relevant for decision-making. Particular attention was paid to relevant outcomes for relatives of fetuses or children undergoing postmortem radiology and defining minimal clinically important differences. Therefore, a focus group was organized in cooperation with the Federation of Patient Organizations in the Netherlands.
The literature was systematically searched using the databases MEDLINE (Ovid) and Embase (a detailed search strategy is available upon request). Selection of the relevant literature was based on predefined inclusion and exclusion criteria and was carried out by members of the working group (JE, RR) in collaboration with the methodologist (EK). For each of the clinical questions, the evidence was summarized by the guideline methodologist using the GRADE approach: a systematic review was performed for each of the relevant outcomes and the quality of evidence was assessed in one of four grades (high, moderate, low, very low) by analyzing limitations in study design or execution (risk of bias), inconsistency of results, indirectness of evidence, imprecision, and publication bias. The evidence synthesis was complemented by a working group member (JE or RR) considering any additional arguments relevant to the clinical question, including relatives values and preferences, and resource use (costs, organization of care issues). Evidence synthesis, complementary arguments, and concept recommendations were extensively discussed in the working group and final recommendations were formulated. Final recommendations are based on the balance of desirable and undesirable outcomes, the quality of the body of evidence across all relevant outcomes, values and preferences, and resource use. The strength of a recommendation reflects the extent to which the guideline panel was confident that desirable effects of the intervention outweigh undesirable effects, or vice versa, across the range of patients for whom the recommendation is intended. The strength of a recommendation is determined by weighting all relevant arguments together, the weight of the body of evidence from the systematic literature analysis, as well as the weight of all complementary arguments. Guideline panels must use judgment in integrating these factors to make a strong or weak recommendation. Thus, a low quality of the body of evidence from the systematic literature analysis does not exclude a strong recommendation, and weak recommendations may follow from high quality evidence [56].
After reaching consensus in the working group, the concept guideline was subjected to peer review by all relevant stakeholders. Amendments were made and agreed upon by the working group, and the final text was presented to the Dutch societies of medical specialists and other organizations that participated in the working group for approval and formal authorization. The guideline will be published and be freely accessible in the Dutch guideline database (Richtlijnendatabase, www.richtlijnendatabase.nl). The Dutch guideline database has a modular structure, with each clinical question as a separate entry, thus allowing for modular updates.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sonnemans, L.J.P., Vester, M.E.M., Kolsteren, E.E.M. et al. Dutch guideline for clinical foetal-neonatal and paediatric post-mortem radiology, including a review of literature. Eur J Pediatr 177, 791–803 (2018). https://doi.org/10.1007/s00431-018-3135-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3135-9