Abstract
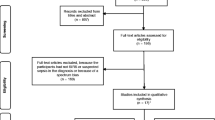
There is growing evidence that presepsin is a promising biomarker in the diagnosis of sepsis in adults. The objective of our study is to investigate current evidence related to the diagnostic accuracy of presepsin in neonatal sepsis. To accomplish this, we searched the Medline (1966–2017), Scopus (2004–2017), Clinicaltrials.gov (2008–2017), EMBASE (1980–2017), Cochrane Central Register of Controlled Trials CENTRAL (1999–2017), and Google Scholar (2004–2017) databases. Eleven studies were included in the present meta-analysis, with a total number of 783 neonates. The pooled sensitivity of serum presepsin for the prediction of neonatal sepsis was 0.91 (95% CI [0.87–0.93]) and the pooled specificity was 0.91 (95% CI [0.88–0.94]). The diagnostic odds ratio was 170.28 (95% CI [51.13–567.11]) and the area under the curve (AUC) was 0.9751 (SE 0.0117). Head-to-head comparison with AUC values of C-reactive protein (0.9748 vs. 0.8580) and procalcitonin (0.9596 vs. 0.7831) revealed that presepsin was more sensitive in detecting neonatal sepsis.
Conclusion: Current evidence support the use of presepsin in the early neonatal period in high-risk populations as its diagnostic accuracy seems to be high in detecting neonatal sepsis.
What is known: • Neonatal sepsis is a leading cause of morbidity and mortality. • Current laboratory tests cannot accurately discriminate endangered neonates. |
What is new: • The diagnostic odds ratio of presepsin is 170.28 and the area under the curve is 0.9751. • According to our meta-analysis, presepsin is a useful protein that may help clinicians identify neonates at risk. |




Similar content being viewed by others
Abbreviations
- 95% CI:
-
95% confidence interval
- AUC:
-
Area under the curve
- DOR:
-
Diagnostic odds ratio
- EOS:
-
Early-onset sepsis
- LOS:
-
Late-onset sepsis
- LPS-LBP:
-
Lipopolysaccharide-lipopolysaccharide binding protein
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- sCD14-ST:
-
Soluble CD14 subtype
- SD:
-
Standard error
- SROC:
-
Summary receiver operating characteristic
References
Adams-Chapman I, Stoll BJ (2006) Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Curr Opin Infect Dis 19(3):290–297. https://doi.org/10.1097/01.qco.0000224825.57976.87
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
Bakhuizen SE, de Haan TR, Teune MJ, van Wassenaer-Leemhuis AG, van der Heyden JL, van der Ham DP, Mol BW (2014) Meta-analysis shows that infants who have suffered neonatal sepsis face an increased risk of mortality and severe complications. Acta Paediatr 103(12):1211–1218. https://doi.org/10.1111/apa.12764
Chiesa C, Panero A, Osborn JF, Simonetti AF, Pacifico L (2004) Diagnosis of neonatal sepsis: a clinical and laboratory challenge. Clin Chem 50(2):279–287. https://doi.org/10.1373/clinchem.2003.025171
Shabuj KH, Hossain J, Moni SC, Dey SK (2017) C-reactive protein (CRP) as a single biomarker for diagnosis of neonatal sepsis: a comprehensive meta-analysis. Mymensingh Med J 26(2):364–371
Pontrelli G, De Crescenzo F, Buzzetti R, Jenkner A, Balduzzi S, Calo Carducci F, Amodio D, De Luca M, Chiurchiu S, Davies EH, Copponi G, Simonetti A, Ferretti E, Di Franco V, Rasi V, Della Corte M, Gramatica L, Ciabattini M, Livadiotti S, Rossi P (2017) Accuracy of serum procalcitonin for the diagnosis of sepsis in neonates and children with systemic inflammatory syndrome: a meta-analysis. BMC Infect Dis 17(1):302. https://doi.org/10.1186/s12879-017-2396-7
Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB, Kipnis P, Escobar GJ (2017) A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr 171(4):365–371. https://doi.org/10.1001/jamapediatrics.2016.4678
Zhou M, Cheng S, Yu J, Lu Q (2015) Interleukin-8 for diagnosis of neonatal sepsis: a meta-analysis. PLoS One 10(5):e0127170. https://doi.org/10.1371/journal.pone.0127170
Memar MY, Alizadeh N, Varshochi M, Kafil HS (2017) Immunologic biomarkers for diagnostic of early-onset neonatal sepsis. J Matern Fetal Neonatal Med:1–11. https://doi.org/10.1080/14767058.2017.1366984
Zou Q, Wen W, Zhang XC (2014) Presepsin as a novel sepsis biomarker. World J Emerg Med 5(1):16–19. https://doi.org/10.5847/wjem.j.1920-8642.2014.01.002
Chenevier-Gobeaux C, Borderie D, Weiss N, Mallet-Coste T, Claessens YE (2015) Presepsin (sCD14-ST), an innate immune response marker in sepsis. Clin Chim Acta 450:97–103. https://doi.org/10.1016/j.cca.2015.06.026
Wu CC, Lan HM, Han ST, Chaou CH, Yeh CF, Liu SH, Li CH, Blaney GN 3rd, Liu ZY, Chen KF (2017) Comparison of diagnostic accuracy in sepsis between presepsin, procalcitonin, and C-reactive protein: a systematic review and meta-analysis. Ann Intensive Care 7(1):91. https://doi.org/10.1186/s13613-017-0316-z
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Weston EJ, Pondo T, Lewis MM, Martell-Cleary P, Morin C, Jewell B, Daily P, Apostol M, Petit S, Farley M, Lynfield R, Reingold A, Hansen NI, Stoll BJ, Shane AL, Zell E, Schrag SJ (2011) The burden of invasive early-onset neonatal sepsis in the United States, 2005–2008. Pediatr Infect Dis J 30(11):937–941. https://doi.org/10.1097/INF.0b013e318223bad2
Quinn JA, Munoz FM, Gonik B, Frau L, Cutland C, Mallett-Moore T, Kissou A, Wittke F, Das M, Nunes T, Pye S, Watson W, Ramos AA, Cordero JF, Huang WT, Kochhar S, Buttery J, Brighton Collaboration Preterm Birth Working Group (2016) Preterm birth: case definition and guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine 34(49):6047–6056. https://doi.org/10.1016/j.vaccine.2016.03.045
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31. https://doi.org/10.1186/1471-2288-6-31
Walter SD (2002) Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med 21(9):1237–1256. https://doi.org/10.1002/sim.1099
Galbraith RF (1988) A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 7(8):889–894
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58(9):882–893. https://doi.org/10.1016/j.jclinepi.2005.01.016
Montaldo P, Rosso R, Santantonio A, Chello G, Giliberti P (2017) Presepsin for the detection of early-onset sepsis in preterm newborns. Pediatr Res 81(2):329–334. https://doi.org/10.1038/pr.2016.217
Xiao T, Chen LP, Zhang LH, Lai FH, Zhang L, Qiu QF, Que RL, Xie S, Wu DC (2017) The clinical significance of sCD14-ST for blood biomarker in neonatal hematosepsis: a diagnostic accuracy study. Medicine (Baltimore) 96(18):e6823. https://doi.org/10.1097/MD.0000000000006823
Tabl HA, Abed NT (2016) Diagnostic value of presepsin in neonatal sepsis. Egypt J Immunol 23(2):29–37
Ozdemir AA, Elgormus Y (2017) Diagnostic value of presepsin in detection of early-onset neonatal sepsis. Am J Perinatol 34(6):550–556. https://doi.org/10.1055/s-0036-1593851
Topcuoglu S, Arslanbuga C, Gursoy T, Aktas A, Karatekin G, Uluhan R, Ovali F (2016) Role of presepsin in the diagnosis of late-onset neonatal sepsis in preterm infants. J Matern Fetal Neonatal Med 29(11):1834–1839. https://doi.org/10.3109/14767058.2015.1064885
Sabry J, Elfeky O, Elsadek A, Eldaly A (2016) Presepsin as an early reliable diagnostic and prognostic marker of neonatal sepsis. Int J Adv Res 4(6):1538–1549
Mussap M, Puxeddu E, Puddu M, Ottonello G, Coghe F, Comite P, Cibecchini F, Fanos V (2015) Soluble CD14 subtype (sCD14-ST) presepsin in premature and full term critically ill newborns with sepsis and SIRS. Clin Chim Acta 451(Pt A):65–70. https://doi.org/10.1016/j.cca.2015.07.025
Poggi C, Bianconi T, Gozzini E, Generoso M, Dani C (2015) Presepsin for the detection of late-onset sepsis in preterm newborns. Pediatrics 135(1):68–75. https://doi.org/10.1542/peds.2014-1755
Saied Osman A, Goudah Awadallah M, Tabl HAEL-M, Samir Saad Goudah E (2015) Presepsin as a novel diagnostic marker in neonatal septicemia. Egypt J Med Microbiol 24(3):21–26
Mostafa R, Kholouss S, Nea M (2015) Detection of presepsin and surface CD14 as a biomarker for early diagnosis of neonatal sepsis. J Am Sci 1111(1010):104–116
Motalib T, Khalaf F, Hendawy GE, Kotb S, Ali A, Sharnoby AE (2015) Soluble CD14-subtype (prespsin) and hepcidin as diagnostic and prognostic markers in early onset neonatal sepsis. Egypt J Med Microbiol 24(3)
Astrawinata D (2017) The role of Presepsin, C-reactive protein and procalcitonin as a marker of therapy response and prognosis for late onset neonatal sepsis in preterm neonates. J Med Sci Clin Res 5(8)
Pavcnik-Arnol M, Hojker S, Derganc M (2007) Lipopolysaccharide-binding protein, lipopolysaccharide, and soluble CD14 in sepsis of critically ill neonates and children. Intensive Care Med 33(6):1025–1032. https://doi.org/10.1007/s00134-007-0626-y
Małgorzata S, Jakub B, Szymańska A, Pukas-Bochenek A, Stachurska A, Godula-Stuglik U (2015) Diagnostic value of presepsin (Scd14-St subtype) evaluation in the detection of severe neonatal infections. Int J Res Stud Biosci 3(1):110–116
Xiao T, Chen LP, Liu H, Xie S, Luo Y, Wu DC (2017) The analysis of etiology and risk factors for 192 cases of neonatal sepsis. Biomed Res Int 2017:8617076. https://doi.org/10.1155/2017/8617076
Chen L, Xiao T, Luo Y, Qiu Q, Que R, Huang X, Wu D (2017) Soluble CD14 subtype (sCD14-ST) is a biomarker for neonatal sepsis. Int J Clin Exp Pathol 10(9):9718–9724
Iroh Tam PY, Bendel CM (2017) Diagnostics for neonatal sepsis: current approaches and future directions. Pediatr Res 82(4):574–583. https://doi.org/10.1038/pr.2017.134
Connell TG, Rele M, Cowley D, Buttery JP, Curtis N (2007) How reliable is a negative blood culture result? Volume of blood submitted for culture in routine practice in a children’s hospital. Pediatrics 119(5):891–896. https://doi.org/10.1542/peds.2006-0440
Pugni L, Pietrasanta C, Milani S, Vener C, Ronchi A, Falbo M, Arghittu M, Mosca F (2015) Presepsin (soluble CD14 subtype): reference ranges of a new sepsis marker in term and preterm neonates. PLoS One 10(12):e0146020. https://doi.org/10.1371/journal.pone.0146020
Dai J, Jiang W, Min Z, Yang J, Tan Y, Ma T, Ge Z (2017) Neutrophil CD64 as a diagnostic marker for neonatal sepsis: meta-analysis. Adv Clin Exp Med 26(2):327–332. https://doi.org/10.17219/acem/58782
Author information
Authors and Affiliations
Contributions
Ioannis Bellos performed the meta-analysis and conducted the electronic search.
Georgia Fitrou conducted the electronic search and tabulated the data.
Vasilios Pergialiotis conceived the idea, formed the tables, designed the statistical analysis, and wrote the manuscript.
Despina N. Perrea performed the sensitivity and meta-regression analysis and wrote the manuscript.
Nikolaos Thomakos tabulated data and wrote the manuscript.
Georgios Daskalakis conceived the idea, wrote, and revised the manuscript.
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Informed consent
The present systematic review and meta-analysis is based on aggregated data that were retrieved from studies already retrieved. We did not collect individual patient data and did not have direct contact with patients included.
Additional information
Communicated by Patrick Van Reempts
Electronic supplementary material
Suppl Fig. 1
(PNG 25 kb)
Suppl Fig. 2
(PNG 55 kb)
Suppl Fig. 3
(PNG 46 kb)
Suppl Fig. 4
(PNG 166 kb)
ESM 1
(DOC 64 kb)
Rights and permissions
About this article
Cite this article
Bellos, I., Fitrou, G., Pergialiotis, V. et al. The diagnostic accuracy of presepsin in neonatal sepsis: a meta-analysis. Eur J Pediatr 177, 625–632 (2018). https://doi.org/10.1007/s00431-018-3114-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3114-1