Abstract
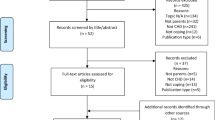
We aimed to describe the experiences of children and adolescents with congenital heart disease (CHD). Electronic databases were searched until August 2016. Qualitative studies of children’s perspectives on CHD were included. Data was extracted using thematic synthesis. From 44 studies from 12 countries involving 995 children, we identified 6 themes: disrupting normality (denying the diagnosis, oscillating between sickness and health, destabilizing the family dynamic), powerlessness in deteriorating health (preoccupation with impending mortality, vulnerability to catastrophic complications, exhaustion from medical testing), enduring medical ordeals (traumatized by invasive procedures, disappointed by treatment failure, displaced by transition, valuing empathy and continuity in care, overcoming uncertainty with information), warring with the body (losing stamina, distressing inability to participate in sport, distorted body image, testing the limits), hampering potential and goals (feeling disabled, unfair judgment and exclusion, difficulties with academic achievement, limiting attainment and maintenance of life milestones), and establishing one’s own pace (demarcating disease from life, determination to survive, taking limitations in their stride, embracing the positives, finding personal enrichment, relying on social or spiritual support).
Conclusion: Children with CHD feel vulnerable and burdened by debilitating physical symptoms, unpredictable complications, and discrimination. Clinicians may support patients by sharing recognition of these profound psychosocial consequences.
What is Known: • CHD is associated with difficulties in learning and attention, school absenteeism, decreased endurance, poor body image, and peer socialization • What is lesser known is how young patients cope with the symptoms, prognostic uncertainty, and treatment burden |
What is New: • We found that children are challenged by lifestyle restrictions, fear of invasive procedures, impaired body image, discrimination, and uncertainty about the future. Feelings of disempowerment are intensified by the unpredictability of disease progression • Thus, strategies to improve outcomes include improved patient education on disease and lifestyle management and partnership with school teachers and counselors for unique psychosocial support |


Similar content being viewed by others
Abbreviations
- CHD:
-
Congenital heart disease
- QOL:
-
Quality of life
References
Acuña Mora M, Sparud-Lundin C, Bratt E-L, Moons P (2017) Person-centred transition programme to empower adolescents with congenital heart disease in the transition to adulthood: a study protocol for a hybrid randomised controlled trial (STEPSTONES project). BMJ Open 7(4):e014593. https://doi.org/10.1136/bmjopen-2016-014593
Andresen B, Andersen MH, Lindberg H, Dohlen G, Fosse E (2014) Perceived health after percutaneous pulmonary valve implantation: in-depth interviews of patients and next-of-kin. BMJ Open 4(7):e005102. https://doi.org/10.1136/bmjopen-2014-005102
Apers S, RassartJ, LuyckxK, OrisL, GoossensE, BudtsW, MoonsP, for the IDI (2016) Bringing Antonovsky’s salutogenic theory to life: a qualitative inquiry into the experiences of young people with congenital heart disease. International Journal of Qualitative Studies on Health and Well-being 11:https://doi.org/10.3402/qhw.v3411.29346
Asif IM, Price D, Fisher LA, Zakrajsek RA, Larsen LK, Raabe JJ, Bejar MP, Rao AL, Harmon KG, Drezner JA (2015) Stages of psychological impact after diagnosis with serious or potentially lethal cardiac disease in young competitive athletes: a new model. J Electrocardiol 48(3):298–310. https://doi.org/10.1016/j.jelectrocard.2014.12.018
Asp A, Bratt EL, Bramhagen AC (2015) Transfer to adult care—experiences of young adults with congenital heart disease. J Pediatr Nurs 30(5):e3–10. https://doi.org/10.1016/j.pedn.2015.05.025
Berghammer MC, Brink E, Rydberg AM, Dellborg M, Ekman I (2015) Committed to life: adolescents’ and young adults’ experiences of living with Fontan circulation. Congenit 10(5):403–412. https://doi.org/10.1111/chd.12244
Birks Y, Sloper P, Lewin R, Parsons J (2007) Exploring health-related experiences of children and young people with congenital heart disease. Health Expect 10(1):16–29. https://doi.org/10.1111/j.1369-7625.2006.00412.x
Bjorbaekmo W, Engelsrud G (2008) I am almost like a fish: an investigation of how children with congenital heart disease experience and perform movement in daily life. Child Care Health Dev 34(6):781–788. https://doi.org/10.1111/j.1365-2214.2008.00851.x
Bratt EL, Sparud-Lundin C, Ostman-Smith I, Axelsson AB (2012) The experience of being diagnosed with hypertrophic cardiomyopathy through family screening in childhood and adolescence. Cardiol Young 22(05):528–535. https://doi.org/10.1017/S1047951111002101
Burstrom A, Ojmyr-Joelsson M, Bratt EL, Lundell B, Nisell M (2016) Adolescents with congenital heart disease and their parents: needs before transfer to adult care. J Cardiovasc Nurs 31(5):399–404. https://doi.org/10.1097/JCN.0000000000000288
Chiang Y-T, Chen C-W, Chen Y-C (2011) From limitation to mastery: exercise experience for adolescents with mild congenital heart disease. J Clin Nurs 20(15-16):2266–2276. https://doi.org/10.1111/j.1365-2702.2011.03723.x
Chiang Y-T, Chen C-W, Su W-J, Wang J-K, C-W L, Li Y-F, Moons P (2015) Between invisible defects and visible impact: the life experiences of adolescents and young adults with congenital heart disease. J Adv Nurs 71(3):599–608. https://doi.org/10.1111/jan.12546
Cornett L, Simms J (2014) At the ‘heart’ of the matter: an exploration of the psychological impact of living with congenital heart disease in adulthood. J Health Psychol 19(3):393–406. https://doi.org/10.1177/1359105312471569
Desai PP, Sutton LJ, Staley MD, Hannon DW (2014) A qualitative study exploring the psychosocial value of weekend camping experiences for children and adolescents with complex heart defects. Child Care Health Dev 40(4):553–561. https://doi.org/10.1111/cch.12056
Donovan EF, Mathews RA, Nixon PA (1983) An exercise program for pediatric patients with congenital heart disease: psychosocial aspects. J Cardiac Rehabil 3:476–480
Doucet SB (1981) The young adult’s perceptions of the effect of congenital heart disease on his life style. Nursing papers Perspectives en Nursing 13:3–16
Etchegary H, Pullman D, Simmonds C, Young TL, Hodgkinson K (2015) It had to be done’: genetic testing decisions for arrhythmogenic right ventricular cardiomyopathy. Clin Genet 88(4):344–351. https://doi.org/10.1111/cge.12513
Gantt LT (1992) Growing up heartsick: the experiences of young women with congenital heart disease. Health Care Women Int 13(3):241–248. https://doi.org/10.1080/07399339209515999
Gantt LT (2002) As normal a life as possible: mothers and their daughters with congenital heart disease. Health Care Women Int. 23(5):481-491
Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, Correa A (2010) Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation 122(22):2254–2263. https://doi.org/10.1161/CIRCULATIONAHA.110.947002
Green A, McSweeney J, Ainley K, Bryant J (2007) In my shoes: children’s quality of life after heart transplantation. Prog Transplant 17(3):199–208. https://doi.org/10.1177/152692480701700307
Gudmundsdottir M, Gilliss CL, Sparacino PS, Tong EM, Messias DK, Foote D (1996) Congenital heart defects and parent-adolescent coping. Fam Syst Health 14(2):245–255. https://doi.org/10.1037/h0089817
Hoffman JIE, Kaplan S, Liberthson RR (2004) Prevalence of congenital heart disease. Am Heart J 147(3):425–439. https://doi.org/10.1016/j.ahj.2003.05.003
Kaisar J, Strodl E, Schweitzer R (2012) Qualitative study of adversity activated development and resilience in adolescents and young adults with congenital heart disease and their parents. Trauma: recovering from deep wounds and exploring the potential for renewal. Nova Science Publishers; Hauppauge, pp 221-237
Kendall L, Lewin RJ, Parsons JM, Veldtman GR, Quirk J, Hardman GE (2001) Factors associated with self-perceived state of health in adolescents with congenital cardiac disease attending paediatric cardiologic clinics. Cardiol Young 11(04):431–438. https://doi.org/10.1017/S1047951101000555
Knowles RL, Tadic V, Hogan A, Bull C, Wren C, Rahi J, Dezateux C (2013) Illness narratives from school-age children with congenital heart defects: children’s perspectives on life experiences and coping strategies related to severity of cardiac diagnosis. Cardiol Young 23:S4
Lee S, Kim S-S (2012) The life experiences of Korean children and adolescents with complex congenital heart disease: a qualitative study. Nurs Health Sci 14(3):398–404. https://doi.org/10.1111/j.1442-2018.2012.00709.x
Lopez KN, Karlsten M, Bonaduce De Nigris F, King J, Salciccioli K, Jiang A, Marelli A, Kovacs AH, Fordis M, Thompson D (2015) Understanding age-based transition needs: perspectives from adolescents and adults with congenital heart disease. Congenit 10(6):561–571. https://doi.org/10.1111/chd.12283
Lunt D, Briffa T, Briffa NK, Ramsay J (2003) Physical activity levels of adolescents with congenital heart disease. Aust J Physiother 49(1):43–50. https://doi.org/10.1016/S0004-9514(14)60187-2
Mackie AS, Rempel GR, Kovacs AH, Kaufman M, Rankin KN, Jelen A, Manlhiot C, Anthony SJ, Magill-Evans J, Nicholas D, Sananes R, Oechslin E, Dragieva D, Mustafa S, Williams E, Schuh M, McCrindle BW (2016) A cluster randomized trial of a transition intervention for adolescents with congenital heart disease: rationale and design of the CHAPTER 2 study. BMC Cardiovasc Disord 16(1):127. https://doi.org/10.1186/s12872-016-0307-2
Mandalenakis Z, Dellborg M (2017) Prognosis is better, still not good, and variable, for adults with congenital heart disease. J Thoracic Dis 9(7):1789–1791. https://doi.org/10.21037/jtd.2017.06.54
McCrindle BW, Williams RV, Mital S, Clark BJ, Russell JL, Klein G, Eisenmann JC (2007) Physical activity levels in children and adolescents are reduced after the Fontan procedure, independent of exercise capacity, and are associated with lower perceived general health. Arch Dis Child 92(6):509–514. https://doi.org/10.1136/adc.2006.105239
McMurray R, Kendall L, Parsons JM, Quirk J, Veldtman GR, Lewin RJP, Sloper P (2001) A life less ordinary: growing up and coping with congenital heart disease. Coron Health Care 5(1):51–57. https://doi.org/10.1054/chec.2001.0112
Mellion K, Uzark K, Cassedy A, Drotar D, Wernovsky G, Newburger JW, Mahony L, Mussatto K, Cohen M, Limbers C, Marino BS (2014) Health-related quality of life outcomes in children and adolescents with congenital heart disease. J Pediatr 164:781–788.e781
Meulenkamp TM, Tibben A, Mollema ED, Van Langen IM, Wiegman A, De Wert GM, De Beaufort ID, Wilde AAM, Smets EMA (2008) Predictive genetic testing for cardiovascular diseases: impact on carrier children. Am J Med Genet A 146:3136–3146
Moola F, Norman M (2011) Down the rabbit hole’: enhancing the transition process for youth with cystic fibrosis and congenital heart disease by re-imagining the future and time. Child Care Health Dev 37(6):841–851. https://doi.org/10.1111/j.1365-2214.2011.01317.x
Moola F, Faulkner GE, Kirsh JA, Kilburn J (2008) Physical activity and sport participation in youth with congenital heart disease: perceptions of children and parents. Adapt Phys Act Q 25(1):49–70. https://doi.org/10.1123/apaq.25.1.49
Moola F, Fusco C, Kirsh JA (2011) “What I wish you knew”: social barriers toward physical activity in youth with congenital heart disease (CHD). Adapt Phys Act Q 28(1):56–77. https://doi.org/10.1123/apaq.28.1.56
Moons P, Pinxten S, Dedroog D, Van Deyk K, Gewillig M, Hilderson D, Budts W (2009) Expectations and experiences of adolescents with congenital heart disease on being transferred from pediatric cardiology to an adult congenital heart disease program. J Adolesc Health 44(4):316–322. https://doi.org/10.1016/j.jadohealth.2008.11.007
Moons P, Bovijn L, Budts W, Belmans A, Gewillig M (2010) Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 122(22):2264–2272. https://doi.org/10.1161/CIRCULATIONAHA.110.946343
Nukulkij P (1993) How Thai families define and manage childhood heart disease. Ph.d., University of illinois at chicago, health sciences center,
Overgaard D, King C, Christensen RF, Schrader A-M, Adamsen L (2013) Living with half a heart—experiences of young adults with single ventricle physiology: a qualitative study. J Cardiovasc Nurs 28:187–196
Pagé MG, Kovacs AH, Irvine J (2012) How do psychosocial challenges associated with living with congenital heart disease translate into treatment interests and preferences? A qualitative approach. Psychol Health 27(11):1260–1270. https://doi.org/10.1080/08870446.2012.667099
Rahman B, Macciocca I, Sahhar M, Kamberi S, Connell V, Duncan RE (2012) Adolescents with implantable cardioverter defibrillators: a patient and parent perspective. Pacing Clin Electrophysiol 35(1):62–72. https://doi.org/10.1111/j.1540-8159.2011.03229.x
Schrøder M, Boisen KA, Reimers J, Teilmann G, Brok J (2015) Quality of life in adolescents and young adults with CHD is not reduced: a systematic review and meta-analysis. Cardiol Young 26:415–425
Shearer K, Rempel GR, Norris CM, Magill-Evans J (2013) “It’s no big deal”: adolescents with congenital heart disease. J Pediatr Nurs 28(1):28–36. https://doi.org/10.1016/j.pedn.2012.03.031
Smart A (2010) Impediments to DNA testing and cascade screening for hypertrophic cardiomyopathy and long QT syndrome: a qualitative study of patient experiences. J Genet Couns 19(6):630–639. https://doi.org/10.1007/s10897-010-9314-0
Sterne GG (1988) Age limits of pediatrics. Pediatrics 81:736–736. Reaffirmed October 2011
Thomas J, Harden A (2008) Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 8(1):45. https://doi.org/10.1186/1471-2288-8-45
Thomason BN (1998) The lived experience of adolescents with significant congenital heart disease. Diss Abstr Int: Section B: Sci Eng 58:2359
Tong EM, Sparacino PS, Messias DK, Foote D, Chesla CA, Gilliss CL (1998) Growing up with congenital heart disease: the dilemmas of adolescents and young adults [see comment]. Cardiol Young 8(3):303–309
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357. https://doi.org/10.1093/intqhc/mzm042
Tong A, Flemming K, McInnes E, Oliver S, Craig J (2012) Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 12:1–8
van der Linde D, Konings EEM, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJM, Roos-Hesselink JW (2011) Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 58(21):2241–2247. https://doi.org/10.1016/j.jacc.2011.08.025
van Staa A, Jedeloo S, van Meeteren J, Latour J (2011) Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents and providers. Child Care Health Dev 37(6):821–832. https://doi.org/10.1111/j.1365-2214.2011.01261.x
Veldtman GR, Matley SL, Kendall L, Quirk J, Gibbs JL, Parsons JM, Hewison J (2000) Illness understanding in children and adolescents with heart disease. Heart 84(4):395–397. https://doi.org/10.1136/heart.84.4.395
Wray J, Maynard L (2008) Specialist cardiac services: what do young people want? Cardiol Young 18(06):569–574. https://doi.org/10.1017/S104795110800317X
Wray J, Frigiola A, Bull C (2013) Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart 99(7):485–490. https://doi.org/10.1136/heartjnl-2012-302831
Zahmacioglu O, Yildiz CE, Koca B, Ugurlucan M, Gokalp S, Cetin G, Eroglu A, Oztunc F (2012) Coming from behind to win—a qualitative research about psychological conditions of adolescents who have undergone open-heart surgery for single ventricle between the ages 0–5. Heart Surg Forum 15:S92
Funding
No funding was secured for this study. LC is supported by the University of Sydney Summer Research Scholarship. AT is supported by the National Health and Medical Research Council Fellowship (1106716). NK is the recipient of a Heart Foundation Future Leader Fellowship (101229).
Author information
Authors and Affiliations
Contributions
Lauren Chong: conceptualized the study, carried out the data collection and analysis, coding of data,drafted the initial manuscript, drafted the manuscript, and approved the final manuscript as submitted.
Dominic Fitzgerald: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Jonathan Craig: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Karine Manera: conceptualized the study, carried out the data collection and analysis, coding of data, drafted the initial manuscript, and approved the final manuscript as submitted.
Camilla Hanson: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
David Celermajer: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Julian Ayer: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Nadine Kasparian: conceptualized the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Allison Tong: conceptualized the study, carried out the data collection and analysis, coding of data, drafted the initial manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed consent
No informed consent was required for this systematic review.
Additional information
Communicated by Peter de Winter
Electronic supplementary material
ESM 1
(DOCX 109kb)
Rights and permissions
About this article
Cite this article
Chong, L.S.H., Fitzgerald, D.A., Craig, J.C. et al. Children’s experiences of congenital heart disease: a systematic review of qualitative studies. Eur J Pediatr 177, 319–336 (2018). https://doi.org/10.1007/s00431-017-3081-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-3081-y