Abstract
Gene-protein assay (GPA), a combination of immunohistochemistry and dual in situ hybridization, allows simultaneous visualization of HER2 protein and gene on a single slide. We aimed to clarify the clinical significance of HER2 intratumoral heterogeneity (ITH) using GPA. We investigated the relationships between various HER2 ITH indicators and clinical course in 102 patients with HER2-positive breast cancer, treated with neoadjuvant trastuzumab and chemotherapy. Five representative microscopic images were captured from each GPA slide of pre-therapeutic biopsy materials. All evaluable cancer cells in the images were individually assessed for HER2 gene copy number and protein expression. Mean and coefficient of variation (CV) of both gene copy number and protein category were calculated, and each was divided into negative, equivocal, and positive. Based on their combined status, cancer cells were classified into nine types. Pathological complete response (pCR) to neoadjuvant treatments showed positive relationships to mean gene copy number (P < 0.001), mean protein category (P < 0.001), and proportion of gene- and protein-positive tumor cells (P < 0.001) and showed negative relationships to the CV of protein category (P < 0.001) and the proportion of gene-amplified but protein-negative tumor cells (P = 0.002). Two diagnostic models, created by combining clinicopathological factors and ITH indicators, showed excellent potential diagnostic ability for pCR (mean gene copy number and protein category CV; AUC = 0.837, proportion of gene- and protein-positive tumor cells; AUC = 0.831). HER2 ITH quantified by GPA is a potential predictive indicator for efficacy of HER2-targeted treatment.




Similar content being viewed by others
Data availability
All data relevant to the study are included in the article.
References
Zardavas D, Irrthum A, Swanton C, Piccart M (2015) Clinical management of breast cancer heterogeneity. Nat Rev Clin Oncol 12:381–394
Beca F, Polyak K (2016) Intratumor heterogeneity in breast cancer. Adv Exp Med Biol 82:169–189
Luque-Cabal M, Garcia-Teijido P, Fernandez-Perez Y et al (2016) Mechanisms behind the resistance to trastuzumab in HER2-amplified breast cancer and strategies to overcome it. Clin Med Insight Oncol 10:21–30
Carey LA, Berry DA, Cirrincione CT, Barry WT, Pitcher BN, Harris LN, Ollila DW, Krop IE, Henry NL, Weckstein DJ, Anders CK, Singh B, Hoadley KA, Iglesia M, Cheang MCU, Perou CM, Winer EP, Hudis CA (2016) Molecular heterogeneity and response to neoadjuvant human epidermal growth factor receptor 2 targeting in CALGB 40601, a randomized phase III trial of paclitaxel plus trastuzumab with or without lapatinib. J Clin Oncol 34:542–549
Vance GH, Barry TS, Bloom KJ et al (2009) Genetic heterogeneity in HER2 testing in breast cancer. Arch Pathol Lab Med 133:611–612
Hanna WM, Ruschoff J, Bilous M et al (2014) HER2 in situ hybridization in breast cancer: clinical implications of polysomy 17 and genetic heterogeneity. Mod Pathol 27:4–18
Wolff AC, Hammond ME, Hicks DG et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, Jenkins RB, Press MF, Spears PA, Vance GH, Viale G, McShane LM, Dowsett M (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J Clin Oncol 36:2105–2122
Lee HJ, Seo AN, Kim EJ, Jang MH, Suh KJ, Ryu HS, Kim YJ, Kim JH, Im SA, Gong G, Jung KH, Park IA, Park SY (2014) HER2 heterogeneity affects trastuzumab responses and survival in patients with HER2-positive metastatic breast cancer. Am J Clin Pathol 142:755–766
Lee HJ, Kim JY, Park SY, Park IA, Song IH, Yu JH, Ahn JH, Gong G (2015) Clinicopathologic significance of the intratumoral heterogeneity of HER2 gene amplification in HER2-positive breast cancer patients treated with adjuvant trastuzumab. Am J Clin Pathol 144:570–578
Seol H, Lee HJ, Choi Y, Lee HE, Kim YJ, Kim JH, Kang E, Kim SW, Park SY (2012) Intratumoral heterogeneity of HER2 gene amplification in breast cancer: its clinicopathological significance. Mod Pathol 25:938–948
Metzger-Filho O, Viale G, Trippa L et al (2019) HER2 heterogeneity as a predictor of response to neoadjuvant T-DM1 plus pertuzumab: results from a prostective clinical trial. J Clin Oncol 37:502–502
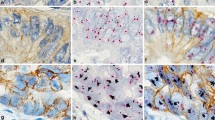
Nitta H, Kelly BD, Padilla M, Wick N, Brunhoeber P, Bai I, Singh S, Ranger-Moore J, Bieniarz C, Tsuda H, Grogan TM (2012) A gene-protein assay for human epidermal growth factor receptor 2 (HER2): brightfield tricolor visualization of HER2 protein, the HER2 gene, and chromosome 17 centromere (CEN17) in formalin-fixed, paraffin-embedded breast cancer tissue sections. Diagn Pathol 7:60
Eckyen EV (2017) Breast Tumours. In: Brierley JD, Gospodarowicz MK, Wittekind C (ed) Union for International Cancer Control (UICC). TNM classification of malignant tumors, 8th edn. John Wiley & Sons, Oxford, pp 151-158
Tsuda H, Akiyama F, Kurosumi M, Sakamoto G, Watanabe T, Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) Pathology Section (1998) Establishment of histological criteria for high-risk node-negative breast carcinoma for a multi-institutional randomized clinical trial of adjuvant therapy. Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) Pathology Section. Jpn J Clin Oncol 28:486–491
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, Hayes DF, Lakhani SR, Chavez-MacGregor M, Perlmutter J, Perou CM, Regan MM, Rimm DL, Symmans WF, Torlakovic EE, Varella L, Viale G, Weisberg TF, McShane LM, Wolff AC (2020) Estrogen progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366
Coates AS, Winer ER, Goldhirsch A et al (2015) Tailoring therapies-improving the management of early breast cancer: St Gallen International Expert Consensus on the primary therapy of early breast cancer 2015. Annals of Oncol 26:1533–1546
Horii R, Nitta H, Ito Y et al (2017) Abstract P1-03-08: simultaneous analyses of HER2 gene and protein status can more precisely predict pathological complete response (pCR) to neoadjuvant trastuzumab with chemotherapy in primary HER2-positive breast cancer. Cancer Res 77 (4 Supplement) P1-03-08-P1-03-08. https://doi.org/10.1158/1538-7445.SABCS16-P1-03-08
Vicario R, Peg V, Morancho B, Zacarias-Fluck M, Zhang J, Martínez-Barriocanal Á, Navarro Jiménez A, Aura C, Burgues O, Lluch A, Cortés J, Nuciforo P, Rubio IT, Marangoni E, Deeds J, Boehm M, Schlegel R, Tabernero J, Mosher R, Arribas J (2015) Patterns of HER2 gene amplification and response to anti-HER2 therapies. PLoS One 10:e0129876
Varga Z, Tubbs RR, Moch H (2014) Concomitant detection of HER2 protein and gen alterations by immunohistochemistry (IHC) and silver enhanced in situ hybridization (SISH) identifies HER2 positive breast cancer with and without gene amplification. PLoS One 9:e105961
Kurozumi S, Padilla M, Kurozumi M et al (2016) HER2 intratumoral heterogeneity analyses by concurrent HER2 gene and protein assessment for the prognosis of HER2 negative invasive breast cancer patients. Breast Cancer Res Treat 158:99–111
Hou Y, Nitta H, Wei L, Banks PM, Portier B, Parwani AV, Li Z (2017) HER2 intratumoral heterogeneity is independently associated with incomplete response to anti-HER2 neoadjuvant chemotherapy in HER2-positive breast carcinoma. Breast Cancer Res Treat 166:447–457
Loh HY, Norman BP, Lai KS, Rahman NMANA, Alitheen NBM, Osman MA (2019) The regulatory role of microRNAs in breast cancer. Int J Mol Sci 20:4940
Jeong J, VanHouten JN, Wonnam K et al (2017) The scaffolding protein NHERF1 regulates the stability and activity of the tyrosine kinase HER2. J Biol Chem 292:6555–6568
Loi S, Dafni U, Karlis D, Polydoropoulou V, Young BM, Willis S, Long B, de Azambuja E, Sotiriou C, Viale G, Rüschoff J, Piccart MJ, Dowsett M, Michiels S, Leyland-Jones B (2016) Effects of estrogen receptor and human epidermal growth factor receptor 2 levels on the efficacy of trastuzumab: a secondary analysis of the HERA trial. JAMA Oncol 2:1040–1047
Harbeck N (2015) Insight into biology of luminal HER2 vs. enriched HER2 subtypes: therapeutic implications. Breast 24:S44–S48
Montagna E, Colleoni M (2019) Hormonal treatment combined with targeted therapies inendocrine-responsive and HER2-positive metastatic breast cancer. Ther Adv Med Oncol 11:1–10
Paradiso A, Scarpi E, Malfettone A, Addati T, Giotta F, Simone G, Amadori D, Mangia A (2013) Nuclear NHERF1 expression as a prognostic marker in breast cancer. Cell Death and Disease 4:e904
Acknowledgments
The authors would like to thank Ms. Tomoyo Kakita, Japanese Foundation for Cancer Research, and Mr. Motoyoshi Iwakoshi, Japanese Foundation for Cancer Research, for their excellent technical support and to thank Dr. Masaaki Matsuura, Teikyo University, and Dr. Toshinari Yamashita, Kanagawa Cancer Center, for their advice.
Funding
This work was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (Grant No. 17K10567).
Author information
Authors and Affiliations
Contributions
RH: conceptualization, data curation, funding acquisition, investigation, methodology, writing of the original draft, and writing of review and editing. HN: conceptualization, investigation, methodology, visualization, and writing of review and editing. MN: statistical analysis and writing of review and editing. RM: conceptualization and writing-review and editing. TU: conceptualization and writing of review and editing. YI: supervision and writing of review and editing. SO: supervision and writing of review and editing. PB: writing of review and editing. HK: supervision and writing of review and editing. FA: conceptualization, methodology, project administration and writing of review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of the Japanese Foundation for Cancer Research on August fourth, 2014 (No. 2014-1033). General consent for the use of specimens was obtained preoperatively from all patients participating in this study.
Consent for publication
This work has not been published before, and it is not under consideration for publication anywhere else. Its publication has been approved by all authors.
Conflict of interest
RH reports receiving honoraria from Chugai Pharmaceutical Co., Ltd. and US-Lead Inc. HN is an employee of Roche Tissue Diagnostics. MN reports receiving honoraria from Chugai Pharmaceutical Co., Ltd. TU reports receiving honoraria from Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd. and Novartis Pharma K.K. YI reports receiving research grants from Chugai Pharmaceutical Co., Ltd., AstraZeneca K.K., PAREXEL International Corp., Novartis Pharma K.K., Eli Lilly Japan K.K., and MSD K.K. SO reports receiving honoraria from Chugai Pharmaceutical Co., Ltd., AstraZeneca K.K. and Eisai Co., Ltd. FA reports receiving a consulting fee from Sysmex Corporation and research grants from Roche Tissue Diagnostics and Hitachi, Ltd. No potential conflicts of interest were disclosed by the other authors.
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Figure 1.
Quantification of HER2 diversity comparing between pCR and non-pCR patient groups (TIF 116 kb). Heat maps of all patients showed the magnitude of the cell proportions as contrasting densities of red color. The maps were arranged from most homogeneous to most heterogeneous, with patients who achieved pCR separated from those who did not.
Supplementary Figure 2.
Relationships between the proportion of each cell type and hormone receptor (HR) status Patients with HR-positive cancer had significantly more type C (P = 0.037), E (P = 0.025), F (P = 0.009), H (P = 0.023) and I cells (P = 0.012) compared to those with HR-negative cancer, while patients with HR-positive cancer included significantly fewer type D (P = 0.047) and G cells (P = 0.021). (TIF 45 kb)
Supplementary Figure 3.
Outcome analyses using the novel diagnostic models Patients with pCR showed a significantly better prognosis compared to those with non-pCR (disease free survival (DFS): P = 0.010, overall survival (OS): P = 0.049). However there was no significant relationship between the novel diagnostic models and prognosis (Model 2: DFS, P = 0.513, OS, P = 0.753; Model 3: DFS, P = 0.206, OS, P = 0.681; Model 4: DFS, P = 0.142, OS, P = 0.579). Only Model 4 tended to be associated with DFS. (TIF 108 kb)
ESM 4
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Horii, R., Nitta, H., Nojima, M. et al. Predictive significance of HER2 intratumoral heterogeneity, determined by simultaneous gene and protein analysis, for resistance to trastuzumab-based treatments for HER2-positive breast cancer. Virchows Arch 479, 13–21 (2021). https://doi.org/10.1007/s00428-021-03036-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-021-03036-2