Abstract
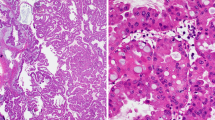
Intraductal papillary epithelial neoplasms of the pancreatobiliary system (intraductal papillary neoplasm of the bile duct (IPNB) and intraductal papillary mucinous neoplasm (IPMN)) seem to share many clinicopathological features; however, IPNB has not been fully characterized. In order to understand the clinicopathological/immunohistochemical features of IPNB better, we compared 52 cases of IPNB with 42 cases of IPMNs with mural nodules. The IPNB cases were divided into two groups according to their histological similarity and according to five key histological findings. All IPNB and IPMN cases mainly affected middle-aged to elderly people, predominantly men. Mucin hypersecretion was less frequent in IPNB compared to IPMN. Group 2 IPNB more frequently had a higher histopathological grade and more extensive stromal invasion than IPMN. Group 1 IPNB and IPMN were further classified into four subtypes (gastric, intestinal, pancreatobiliary, and oncocytic). Although each subtype of IPNB and IPMN showed similar histology, the immunohistochemical results were different. The gastric type of IPNB was less frequently positive for CDX2, and intestinal IPNB was more frequently positive for MUC1 and less frequently positive for MUC2, MUC5AC, and CDX2 compared to each subtype of IPMN, respectively. In conclusion, IPNB and IPMN have some clinicopathological features in common, but mucin hypersecretion was less frequent both in IPNBs than in IPMN. Group 2 IPNB differed from IPMN in several parameters of tumor aggressiveness. Additional clinicopathological and molecular studies should be performed with respect to the subtypes of IPNB and IPMN.





Similar content being viewed by others
References
Nakanuma Y, Curado M-P, Franceschi S, Gores G, Paradis V, Sripa B (2010) Intrahepatic cholangiocarcinoma. In: Bosman F, Carmeiro F, Hruban RH, Theise ND (eds) WHO classification of tumours of the digestive system, 4th edn. International Agency for Research on Cancer, Lyon, pp 217–224
Klöppel G, Kosmahl M (2006) Is the intraductal papillary mucinous neoplasia of the biliary tract a counterpart of pancreatic papillary mucinous neoplasm? J Hepatol 44:249–250
Chen TC, Nakanuma Y, Zen Y, Chen MF, Jan YY, Yeh TS, Chiu CT, Kuo TT, Kamiya J, Oda K, Hamaguchi M, Ohno Y, Hsieh LL, Nimura Y (2001) Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology 34:651–658
Shibahara H, Tamada S, Goto M, Oda K, Nagino M, Nagasaka T, Batra SK, Hollingsworth MA, Imai K, Nimura Y, Yonezawa S (2004) Pathologic features of mucin-producing bile duct tumors. Two histopathologic categories as counterparts of pancreatic intraductal papillary-mucinous neoplasms. Am J Surg Pathol 28:327–338
Ohtsuka M, Shimizu H, Kato A, Yoshitomi H, Furukawa K, Tsuyuguchi T, Sakai Y, Yokosuka O, Miyazaki M (2014) Intraductal papillary neoplasms of the bile duct. Int J Hepatol. doi:10.1155/2014/45909
Hruban RH, Pitman MB, Klimstra DS (2007) Intraductal neoplasms. In: AFIP ATLAS OF TUMOR PATHOLOGY Series 4. Tumors of the pancreas. American Registry of Pathology and Armed Forces Institute of Pathology, Washington, DC, pp 75–110
Minagawa N, Sato N, Mori Y, Tamura T, Higure A, Yamaguchi K (2013) A comparison between intraductal papillary neoplasms of the biliary tract (BT-IPMNs) and intraductal papillary mucinous neoplasms of the pancreas (P-IPMNs) reveals distinct clinical manifestations and outcomes. Eur J Surg Oncol 39:554–558
Kloek JJ, van der Gaag NA, Erdogan D, Rauws EA, Busch OR, Gouma DJ, ten Kate FJ, van Gulik TM (2011) A comparative study of intraductal papillary neoplasia of the biliary tract and pancreas. Hum Pathol 42:824–832
Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, Yamamoto M, Isayama H, Tabata M, Kinoshita H, Kamisawa T, Inui K (2014) Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci 21:176–185
Nakanuma Y (2010) A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int 60:419–429
Wang M, Deng BY, Wen TF, Peng W, Li C, Trishul NM (2016) An observational and comparative study on intraductal papillary mucinous neoplasm of the biliary tract and the cohort. Clin Res Hepatol Gastroenterol 40:161–168
Adsay NV, Fukushima N, Furukawa T, Hruban RH, Klimstra DS, Klöppel G, Offerhaus GJA, Pitman MB, Shimizu M, Zamboni G (2010) Intraductal neoplasms of the pancreas. In: Bosman F, Carmeiro F, Hruban RH, Theise ND (eds) WHO classification of tumours of the digestive system, 4th edn. International Agency for Research on Cancer, Lyon, pp 304–313
Zen Y, Fujii T, Itatsu K, Nakamura K, Minato H, Kasashima S, Kurumaya H, Katayanagi K, Kawashima A, Masuda S, Niwa H, Mitsui T, Asada Y, Miura S, Ohta T, Nakanuma Y (2006) Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology 44:1333–1343
Schlitter AM, Jang KT, Klöppel G, Saka B, Hong SM, Choi H, Offerhaus GJ, Hruban RH, Zen Y, Konukiewitz B, Regel I, Allgauer M, Balci S, Basturk O, Reid MD, Esposito I, Adsay V (2015) Intraductal tubulopapillary neoplasms of the bile ducts: clinicopathologic, immunohistochemical, and molecular analysis of 20 cases. Modern Pathol 28:1249–1264
Schlitter AM, Born D, Bettstetter M, Specht K, Kim-Fuchs C, Riener MO, Jeliazkova P, Sipos B, Siveke JT, Terris B, Zen Y, Schuster T, Hofler H, Perren A, Kloppel G, Esposito I (2014) Intraductal papillary neoplasms of the bile duct: stepwise progression to carcinoma involves common molecular pathways. Modern Pathol 27:73–86
Tsai JH, Yuan RH, Chen YL, Liau JY, Jeng YM (2013) GNAS is frequently mutated in a specific subgroup of intraductal papillary neoplasms of the bile duct. Am J Surg Pathol 37:1862–1870
Sasaki M, Matsubara T, Nitta T, Sato Y, Nakanuma Y (2013) GNAS and KRAS mutations are common in intraductal papillary neoplasms of the bile duct. PLoS One 8:e81706
Matthaei H, Wu J, Dal Molin M, Debeljak M, Lingohr P, Katabi N, Klimstra DS, Adsay NV, Eshleman JR, Schulick RD, Kinzler KW, Vogelstein B, Hruban RH, Maitra A (2012) GNAS codon 201 mutations are uncommon in intraductal papillary neoplasms of the bile duct. HPB 14:677–683
Ajioka Y, Watanabe H, Jass JR (1997) MUC1 and MUC2 mucins in flat and polypoid colorectal adenomas. Clin Pathol 50:417–421
Yonezawa S, Higashi M, Yamada N, Yokoyama S, Kitamoto S, Kitajima S, Goto M (2011) Mucins in human neoplasms: clinical pathology, gene expression and diagnostic application. Pathol Int 61:697–716
Drummond F, Putt W, Fox M, Edwards YH (1997) Cloning and chromosome assignment of the human CDX2 gene. Ann Hum Genet 61:393–400
Werling RW, Yaziji H, Bacchi CE, Gown AM (2003) CDX2, a highly sensitive and specific marker of adenocarcinomas of intestinal origin. An immunohistochemical survey of 476 primary and metastatic carcinomas. Am J Surg Pathol 27:303–310
Reid MD, Stallworth CR, Lewis MM, Akkas G, Memis B, Bastrurk O, Adsay NV (2016) Cytopathologic diagnosis of oncocytic type intraductal papillary mucinous neoplasm: criteria and clinical implications of accurate diagnosis. Cancer Cytopathol 124:122–134
Adsay NV, Adair DF, Heffess CS, Klimstra DS (1996) Intraductal oncocytic papillary neoplasms of the pancreas. Am J Surg Pathol 20:980–994
Marchegiani G, Mino-Kenudson M, Ferrone CR, Warshaw AL, Lillemore KD, Fernandez-del Castillo C (2015) Oncocytic-type intraductal papillary mucinous neoplasms: a unique malignant pancreatic tumor with good long-term prognosis. J Am Coll Surg 220:839–844
Basturk O, Khayyata S, Klimstra DS, Hruban RH, Zamboni G, Coban I, Adsay NV (2010) Preferential expression of MUC6 in oncocytic and pancreatobiliary types of intraductal papillary neoplasms highlights a pyloropancreatic pathway, in pancreatic carcinogenesis. Am J Surg Pathol 34:364–370
Acknowledgements
The authors thank Dr. Katsuhiko Uesaka, Director of the Department of Hepatobiliary Surgery in Shizuoka Cancer Center, for his support on the clinicopathological analysis of biliary tract carcinoma cases in Shizuoka Cancer Center, and also Dr. Jo Matsuoka, Research Support Center, Juntendo University Graduate School of Medicine, Tokyo, Japan, for his advice on statistical methods. The authors also thank Dr. R Wada, Professor of Juntendo Shizuoka Hospital, Department of Clinical Pathology; Dr. N. Tomita, Professor of Juntendo Urayasu Hospital, Department of Clinical Pathology; and Dr. T. Matsumoto, Professor of Juntendo Nerima Hospital, Department of Clinical Pathology, for providing us the opportunity to analyze IPMN cases resected at their hospitals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board approval was obtained from Shizuoka Cancer Center.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Fukumura, Y., Nakanuma, Y., Kakuda, Y. et al. Clinicopathological features of intraductal papillary neoplasms of the bile duct: a comparison with intraductal papillary mucinous neoplasm of the pancreas with reference to subtypes. Virchows Arch 471, 65–76 (2017). https://doi.org/10.1007/s00428-017-2144-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2144-9