Abstract
Purpose
Esophageal cancer is one of the deadliest cancers worldwide. Esophagectomy with lymphadenectomy is regarded as the only curative option for resectable esophageal cancer, but it is associated with high morbidity and mortality. Multidisciplinary team (MDT) management was recently associated with improved outcomes after surgery for esophageal cancer. The aim of this study was to investigate the effect of standardizing procedures for minimally invasive esophagectomy (MIE) in the MDT setting.
Methods
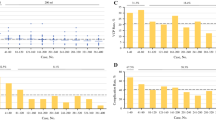
This was a case-matched control study of 154 patients with esophageal cancer who underwent thoracoscopic esophagectomy in the prone position (TEP) between 2012 and 2016. Surgery was performed by two attending surgeons (surgeons A and B) who began working together in the same MDT in 2015. At that time, the following surgical procedures were standardized between surgeons A and B: mediastinal lymphadenectomy, abdominal procedures, and estimation of the blood supply of the gastric conduit. Short-term outcomes were compared between the following paired groups using propensity scores: surgeon A’s pre- and post-standardization groups, surgeon B’s pre- and post-standardization groups, and surgeon A’s post-standardization group and surgeon B’s post-standardization group.
Results
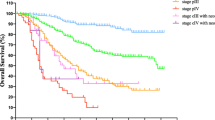
Concerning surgeon A, the estimated total blood loss in the post-standardization group (142 ± 87 mL) was significantly lower than that in the pre-standardization group (376 ± 215 mL, P = 0.006). The rate of left recurrent laryngeal nerve palsy in the post-standardization group (13%) was significantly lower than that in the pre-standardization group (47%, P = 0.046). Concerning surgeon B, the rate of anastomotic leakage in the post-standardization group (0%) was significantly lower than that in the pre-standardization group (11%, P = 0.039). Comparing the post-standardization groups of surgeons A and B, there were no significant differences in operative outcomes or morbidity.
Conclusions
Standardizing procedures for MIE improved and homogenized surgical short-term outcomes.




Similar content being viewed by others
References
Pennathur A, Gibson MK, Jobe BA, Luketich JD (2013) Oesophageal carcinoma. Lancet 381:400–412
Enzinger PC, Mayer RJ (2003) Esophageal cancer. N Engl J Med 349:2241–2252
Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, Gebski V (2011) Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol 12:681–692
Scheepers JJ, Mulder CJ, van der Peet DL, Meijer S, Cuesta MA (2006) Minimally invasive oesophageal resection for distal oesophageal cancer; a review of literature. Scand J Gastroenterol 41:123–134
Watson A (1994) Operable esophageal cancer: current results from the West. World J Surg 18:361–366
Stephens MR, Lewis WG, Brewster AE, Lord I, Blackshaw GR, Hodzovic I, Thomas GV, Roberts SA, Crosby TD, Gent C, Allison MC, Shute K (2006) Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 19:164–171
Oshikiri T, Yasuda T, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Nakamura T, Fujino Y, Tominaga M, Suzuki S, Kakeji Y (2016) Trainee competence in thoracoscopic esophagectomy in the prone position: evaluation using cumulative sum techniques. Langenbeck's Arch Surg 401:797–804
Oshikiri T, Yasuda T, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Nakamura T, Fujino Y, Tominaga M, Suzuki S, Kakeji Y (2017) Short-term outcomes and one surgeon’s learning curve for thoracoscopic esophagectomy performed with the patient in the prone position. Surg Today 47:313–319
Sobin LH, Gospodarowicz MK, Wittekind C (2010) TNM classification of malignant tumors, 7th edn. Wiley-Blackwell, Oxford
Oshikiri T, Yasuda T, Kawasaki K, Harada H, Oyama M, Hasegawa H, Ohara T, Sendo H, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2016) Hand-assisted laparoscopic surgery (HALS) is associated with less-restrictive ventilatory impairment and less risk for pulmonary complication than open laparotomy in thoracoscopic esophagectomy. Surgery 159:459–466
Oshikiri T, Yasuda T, Harada H, Goto H, Oyama M, Hasegawa H, Ohara T, Sendo H, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2015) A new method (the “Bascule method”) for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 29:2442–2450
Oshikiri T, Nakamura T, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Suzuki S, Kakeji Y (2017) Reliable surgical techniques for lymphadenectomy along the left recurrent laryngeal nerve during thoracoscopic esophagectomy in the prone position. Ann Surg Oncol 24:1018
Oshikiri T, Nakamura T, Miura Y, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Suzuki S, Kakeji Y (2017) A new method (the “Pincers maneuver”) for lymphadenectomy along the right recurrent laryngeal nerve during thoracoscopic esophagectomy in the prone position for esophageal cancer. Surg Endosc 31:1496–1504
Oshikiri T, Nakamura T, Miura Y, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda Y, Matsuda T, Sumi Y, Suzuki S, Kakeji Y (2017) Practical surgical techniques for lymphadenectomy along the right recurrent laryngeal nerve during thoracoscopic esophagectomy in the prone position. Ann Surg Oncol 24:2302
Shimada Y, Okumura T, Nagata T, Sawada S, Matsui K, Hori R, Yoshioka I, Yoshida T, Osada R, Tsukada K (2011) Usefulness of blood supply visualization by indocyanine green fluorescence for reconstruction during esophagectomy. Esophagus 8:259–266
Murawa D, Hünerbein M, Spychata A, Nowaczyk P, Połom K, Murawa P (2012) Indocyanine green angiography for evaluation of gastric conduit perfusion during esophagectomy—first experience. Acta Chir Belg 112:275–280
Pacheco PE, Hill SM, Henriques SM, Paulsen JK, Anderson RC (2013) The novel use of intraoperative laser-induced fluorescence of indocyanine green tissue angiography for evaluation of the gastric conduit in esophageal reconstructive surgery. Am J Surg 205:349–353
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Bertelsen CA, Bols B, Ingeholm P, Jansen JE, Neuenschwander AU, Vilandt J (2011) Can the quality of colonic surgery be improved by standardization of surgical technique with complete mesocolic excision? Color Dis 13:1123–1129
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Oshikiri, T., Nakamura, T., Hasegawa, H. et al. Standardizing procedures improves and homogenizes short-term outcomes after minimally invasive esophagectomy. Langenbecks Arch Surg 403, 221–234 (2018). https://doi.org/10.1007/s00423-018-1661-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1661-6