Abstract
Introduction
Aerobic exercise has a favorable effect on systemic vascular function, reducing both central (large elastic artery) and peripheral (smaller muscular artery) stiffness. The effects of resistance exercise (RE) on arterial stiffness are more complex. Acute RE increases central artery stiffness while decreasing peripheral stiffness. To date, the majority of studies have been performed in predominantly male participants.
Purpose
To examine the effect of acute RE on central and peripheral arterial stiffnesses in women, a secondary purpose was to explore the influence of cyclic changes in estrogen status across the menstrual cycle on the arterial response to acute RE.
Methods
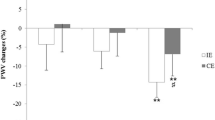
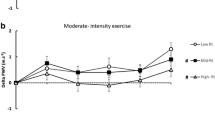
18 healthy women [28 ± 7 years, body mass index (BMI) 22.6 ± 2.9 kg/m2] completed an acute RE bout during the early follicular and the early luteal phase of their menstrual cycle. Salivary 17β-Estradiol concentration was measured during each phase, using a passive drool technique. Pulse-wave velocity (PWV) was obtained from the carotid–femoral and carotid–radial pulse sites to measure central and peripheral stiffness, respectively, using applanation tonometry. PWV was measured at rest, immediately, 10, 20, and 30 min post-RE.
Results
17β-Estradiol concentration was significantly lower in the early follicular vs. the early luteal phase of the menstrual cycle (1.78 ± 0.51 vs. 2.40 ± 0.26 pg/ml, p = 0.01). Central PWV significantly increased (p < 0.05) and peripheral PWV significantly decreased (p < 0.05) post-RE in both the early follicular and early luteal phases. No phase-by-time interaction was detected for either vascular segment (p > 0.05).
Conclusion
Women experience increases in central arterial stiffness and reductions in peripheral arterial stiffness following acute RE. Menstrual cycle phase may not influence changes in arterial stiffness in response to acute RE.


Similar content being viewed by others
Abbreviations
- AIx(75):
-
Augmentation index (@Heart Rate 75)
- AP:
-
Augmented pressure
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- cMAP:
-
Central mean arterial pressure
- CCA:
-
Common carotid artery
- DBP:
-
Diastolic blood pressure
- Pf:
-
Forward wave pressure
- PP:
-
Pulse pressure
- PWV:
-
Pulse-wave velocity
- Pb:
-
Reflected wave pressure
- RM:
-
Repetition maximum
- RE:
-
Resistance exercise
- SBP:
-
Systolic blood pressure
- Tr:
-
Time to reflection
- WSA:
-
Wave separation analysis
References
Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW (2010) Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med (Maywood NJ) 235(1):111–118. https://doi.org/10.1258/ebm.2009.009186
Arce Esquivel AA, Welsch MA (2007) High and low volume resistance training and vascular function. Int J Sports Med 28(3):217–221. https://doi.org/10.1055/s-2006-924291
Baechle TR, Earle RW (2008) Essentials of strength training and conditioning, 3rd edn. Champaign, IL. Human kinetics
Choi Y, Akazawa N, Zempo-Miyaki A, Ra SG, Shiraki H, Ajisaka R, Maeda S (2016) Acute effect of high-intensity eccentric exercise on vascular endothelial function in young men. J Strength Cond Res 30(8):2279–2285. https://doi.org/10.1519/jsc.0000000000000536
Collier SR, Diggle MD, Heffernan KS, Kelly EE, Tobin MM, Fernhall B (2010) Changes in arterial distensibility and flow-mediated dilation after acute resistance vs. aerobic exercise. J Strength Cond Res 24(10):2846–2852. https://doi.org/10.1519/JSC.0b013e3181e840e0
Cortez-Cooper MY, DeVan AE, Anton MM, Farrar RP, Beckwith KA, Todd JS, Tanaka H (2005) Effects of high intensity resistance training on arterial stiffness and wave reflection in women. Am J hypertens 18(7):930–934. https://doi.org/10.1016/j.amjhyper.2005.01.008
DeVan AE, Anton MM, Cook JN, Neidre DB, Cortez-Cooper MY, Tanaka H (2005) Acute effects of resistance exercise on arterial compliance. J Appl Physiol (Bethesda Md 1985) 98(6):2287–2291. https://doi.org/10.1152/japplphysiol.00002.2005
Fahs CA, Heffernan KS, Fernhall B (2009) Hemodynamic and vascular response to resistance exercise with l-arginine. Med Sci Sports Exerc 41(4):773–779. https://doi.org/10.1249/MSS.0b013e3181909d9d
Fok H, Guilcher A, Li Y, Brett S, Shah A, Clapp B, Chowienczyk P (2014) Augmentation pressure is influenced by ventricular contractility/relaxation dynamics: novel mechanism of reduction of pulse pressure by nitrates. Hypertension (Dallas Tex 1979) 63(5):1050–1055. https://doi.org/10.1161/hypertensionaha.113.02955
Franklin NC, Ali M, Goslawski M, Wang E, Phillips SA (2014) Reduced vasodilator function following acute resistance exercise in obese women. Front Physiol 5:253. https://doi.org/10.3389/fphys.2014.00253
Harris RA, Tedjasaputra V, Zhao J, Richardson RS (2012) Premenopausal women exhibit an inherent protection of endothelial function following a high-fat meal. Reprod Sci (Thousand Oaks Calif) 19(2):221–228. https://doi.org/10.1177/1933719111418125
Heffernan KS, Rossow L, Jae SY, Shokunbi HG, Gibson EM, Fernhall B (2006) Effect of single-leg resistance exercise on regional arterial stiffness. Eur J Appl Physiol 98(2):185–190. https://doi.org/10.1007/s00421-006-0259-9
Heffernan KS, Collier SR, Kelly EE, Jae SY, Fernhall B (2007a) Arterial stiffness and baroreflex sensitivity following bouts of aerobic and resistance exercise. Int J Sports Med 28(3):197–203. https://doi.org/10.1055/s-2006-924290
Heffernan KS, Jae SY, Echols GH, Lepine NR, Fernhall B (2007b) Arterial stiffness and wave reflection following exercise in resistance-trained men. Med Sci Sports Exerc 39(5):842–848. https://doi.org/10.1249/mss.0b013e318031b03c
Heffernan KS, Patvardhan EA, Hession M, Ruan J, Karas RH, Kuvin JT (2010) Elevated augmentation index derived from peripheral arterial tonometry is associated with abnormal ventricular-vascular coupling. Clin Physiol Funct Imaging 30(5):313–317. https://doi.org/10.1111/j.1475-097X.2010.00943.x
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ (2011) Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 123(8):933–944. https://doi.org/10.1161/CIR.0b013e31820a55f5
Hughes AD, Park C, Davies J, Francis D, Mc GTSA., Mayet J, Parker KH (2013) Limitations of augmentation index in the assessment of wave reflection in normotensive healthy individuals. PloS One 8(3):e59371. https://doi.org/10.1371/journal.pone.0059371
Joyner MJ, Halliwill JR (2000) Neurogenic vasodilation in human skeletal muscle: possible role in contraction-induced hyperaemia. Acta Physiol Scand 168(4):481–488. https://doi.org/10.1046/j.1365-201x.2000.00700.x
Kingsley JD, Tai YL, Mayo X, Glasgow A, Marshall E (2017) Free-weight resistance exercise on pulse wave reflection and arterial stiffness between sexes in young, resistance-trained adults. Eur J Sport Sci 17(8):1056–1064. https://doi.org/10.1080/17461391.2017.1342275
Kingwell BA, Berry KL, Cameron JD, Jennings GL, Dart AM (1997) Arterial compliance increases after moderate-intensity cycling. Am J Physiol 273(5 Pt 2):H2186-2191
Lefferts WK, Augustine JA, Heffernan KS (2014) Effect of acute resistance exercise on carotid artery stiffness and cerebral blood flow pulsatility. Front Physiol 5:101. https://doi.org/10.3389/fphys.2014.00101
MacDougall JD, McKelvie RS, Moroz DE, Sale DG, McCartney N, Buick F (1992) Factors affecting blood pressure during heavy weight lifting and static contractions. J Appl Physiol (Bethesda, Md: 1985) 73(4):1590–1597
Mendelsohn ME, Karas RH (2005) Molecular and cellular basis of cardiovascular gender differences. Science 308(5728):1583–1587. https://doi.org/10.1126/science.1112062
Miyachi M, Donato AJ, Yamamoto K, Takahashi K, Gates PE, Moreau KL, Tanaka H (2003) Greater age-related reductions in central arterial compliance in resistance-trained men. Hypertension (Dallas Tex 1979) 41(1):130–135
Miyachi M, Kawano H, Sugawara J, Takahashi K, Hayashi K, Yamazaki K, Tabata I, Tanaka H (2004) Unfavorable effects of resistance training on central arterial compliance: a randomized intervention study. Circulation 110(18):2858–2863. https://doi.org/10.1161/01.cir.0000146380.08401.99
Okamoto T, Sakamaki MS, Min SK, Yoshida S, Watanabe Y, Ogasawara R (2015) Repeated cessation and resumption of resistance training attenuates increases in arterial stiffness. Int J Sports Med 36(6):440–445. https://doi.org/10.1055/s-0034-1398584
Okamoto T, Kobayashi R, Sakamaki-Sunaga M (2017) Effect of resistance exercise on arterial stiffness during the follicular and luteal phases of the menstrual cycle. Int J Sports Med 38(5):347–352. https://doi.org/10.1055/s-0043-101377
Otsuki T, Maeda S, Iemitsu M, Saito Y, Tanimura Y, Ajisaka R, Miyauchi T (2007) Vascular endothelium-derived factors and arterial stiffness in strength- and endurance-trained men. Am J Physiol Heart Circ Physiol 292(2):H786-791. https://doi.org/10.1152/ajpheart.00678.2006
Phillips SA, Das E, Wang J, Pritchard K, Gutterman DD (2011) Resistance and aerobic exercise protects against acute endothelial impairment induced by a single exposure to hypertension during exertion. J Appl Physiol (Bethesda, Md: 1985) 110(4):1013–1020. https://doi.org/10.1152/japplphysiol.00438.2010
Raastad T, Glomsheller T, Bjoro T, Hallen J (2001) Changes in human skeletal muscle contractility and hormone status during 2 weeks of heavy strength training. Eur J Appl Physiol 84(1–2):54–63. https://doi.org/10.1007/s004210000328
Seals DR, Desouza CA, Donato AJ, Tanaka H (2008) Habitual exercise and arterial aging. J Appl Physiol (Bethesda, Md: 1985) 105(4):1323–1332. https://doi.org/10.1152/japplphysiol.90553.2008
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, Berra K, Blair SN, Costa F, Franklin B, Fletcher GF, Gordon NF, Pate RR, Rodriguez BL, Yancey AK, Wenger NK (2003) Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 107(24):3109–3116. https://doi.org/10.1161/01.cir.0000075572.40158.77
Tinken TM, Thijssen DH, Hopkins N, Dawson EA, Cable NT, Green DJ (2010) Shear stress mediates endothelial adaptations to exercise training in humans. Hypertension (Dallas: 1979) 55(2):312–318. https://doi.org/10.1161/hypertensionaha.109.146282
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, Heffernan KS, Lakatta EG, McEniery CM, Mitchell GF, Najjar SS, Nichols WW, Urbina EM, Weber T (2015) Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American heart association. Hypertension (Dallas: 1979) 66(3):pp 698–722. https://doi.org/10.1161/hyp.0000000000000033
Vlachopoulos C, Aznaouridis K, Stefanadis C (2010) Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 55(13):1318–1327. https://doi.org/10.1016/j.jacc.2009.10.061
Vongpatanasin W, Tuncel M, Mansour Y, Arbique D, Victor RG (2001) Transdermal estrogen replacement therapy decreases sympathetic activity in postmenopausal women. Circulation 103(24):2903–2908
Wang M, Baker L, Tsai BM, Meldrum KK, Meldrum DR (2005) Sex differences in the myocardial inflammatory response to ischemia-reperfusion injury. Am J Physiol Endocrinol Metabol 288(2):E321-326. https://doi.org/10.1152/ajpendo.00278.2004
Weber T, Wassertheurer S, Rammer M, Maurer E, Hametner B, Mayer CC, Kropf J, Eber B (2011) Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension (Dallas Tex 1979) 58(5):825–832. https://doi.org/10.1161/hypertensionaha.111.176313
Weber T, Wassertheurer S, Schmidt-Trucksass A, Rodilla E, Ablasser C, Jankowski P, Lorenza Muiesan M, Giannattasio C, Mang C, Wilkinson I, Kellermair J, Hametner B, Pascual JM, Zweiker R, Czarnecka D, Paini A, Salvetti M, Maloberti A, McEniery C (2017) Relationship between 24-hour ambulatory central systolic blood pressure and left ventricular mass: a prospective multicenter study. Hypertension (Dallas., Tex: 1979) 70(6):1157–1164. https://doi.org/10.1161/hypertensionaha.117.09917
Westerhof BE, Guelen I, Westerhof N, Karemaker JM, Avolio A (2006) Quantification of wave reflection in the human aorta from pressure alone: a proof of principle. Hypertension (Dallas Tex 1979) 48(4):595–601. https://doi.org/10.1161/01.hyp.0000238330.08894.17
Williams MR, Westerman RA, Kingwell BA, Paige J, Blombery PA, Sudhir K, Komesaroff PA (2001) Variations in endothelial function and arterial compliance during the menstrual cycle. J Clin Endocrinol Metabol 86(11):5389–5395
Yoon ES, Jung SJ, Cheun SK, Oh YS, Kim SH, Jae SY (2010) Effects of acute resistance exercise on arterial stiffness in young men. Korean Circ J 40(1):16–22. https://doi.org/10.4070/kcj.2010.40.1.16
Zaydun G, Tomiyama H, Hashimoto H, Arai T, Koji Y, Yambe M, Motobe K, Hori S, Yamashina A (2006) Menopause is an independent factor augmenting the age-related increase in arterial stiffness in the early postmenopausal phase. Atherosclerosis 184(1):137–142. https://doi.org/10.1016/j.atherosclerosis.2005.03.043
Zhai P, Eurell TE, Cotthaus R, Jeffery EH, Bahr JM, Gross DR (2000) Effect of estrogen on global myocardial ischemia-reperfusion injury in female rats. Am J Physiol Heart Circ Physiol 279(6):H2766–2775
Acknowledgements
NIH NIA P30 AG0344645 05 (KSH) supported this study.
Author information
Authors and Affiliations
Contributions
JAA data collection, statistical analyses, writing of manuscript, response, and management of reviewer comments and manuscript submission. KNN data collection and recruitment. KSH Assist with writing of manuscript and manuscript edits, supervisor.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose. The results of this study are presented clearly, honestly and without fabrication, or inappropriate data manipulation.
Additional information
Communicated by I. Mark Olfert.
Rights and permissions
About this article
Cite this article
Augustine, J.A., Nunemacher, K.N. & Heffernan, K.S. Menstrual phase and the vascular response to acute resistance exercise. Eur J Appl Physiol 118, 937–946 (2018). https://doi.org/10.1007/s00421-018-3815-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-018-3815-1