Abstract
Purpose
The success of surgical treatment for idiopathic epiretinal membrane (ERM) is measured by postoperative best-corrected visual acuity (BCVA), metamorphopsia, and foveal retinal sensitivity (RS).This study searched for predictive biomarkers of surgical success by determining the association between foveal RS and various aspects of vessel density (VD) in the fovea of patients with ERM.
Methods
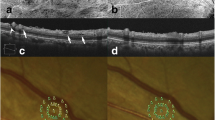
The study examined 25 eyes of 25 patients with ERM who underwent 27-gauge microincision vitrectomy surgery (MIVS). RS was measured with microperimetry (MP-3; NIDEK) at four central points in the fovea with an interpoint distance of 2°. VD was measured with SD-OCT (RS 3000; NIDEK) within the 1-mm2 square defined by the 4 RS points at various depths, including the superficial and deep retinal capillary plexus (SCP and DCP, respectively).
Results
Though VD did not change throughout the follow-up period, BCVA and RS significantly improved 1 and 3 months after surgery, respectively (both P < 0.0017). Postoperative RS at 6 months was positively correlated with postoperative DCP VD at 1, 3, and 6 months (r = 0.62, P = 0.001; r = 0.40, P = 0.049; r = 0.53, P = 0.007, respectively), but not with SCP VD at any time point. Multiple regression analysis confirmed that postoperative RS at 6 months was associated with postoperative DCP VD at 1 month (P = 0.03).
Conclusion
Higher postoperative DCP VD at 1 month contributed to better postoperative foveal RS at 6 months. Early postoperative VD in the fovea might be a useful predictive biomarker of late postoperative RS in the fovea in ERM patients.





Similar content being viewed by others
References
Kwok A, Lai TY, Yuen KS (2005) Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Exp Ophthalmol 33:379–385
Kwok AK, Lai TY, Li WW, Woo DC, Chan NR (2004) Indocyanine green-assisted internal limiting membrane removal in epiretinal membrane surgery: a clinical and histologic study. Am J Ophthalmol 138:194–199
Shimada H, Nakashizuka H, Hattori T, Mori R, Mizutani Y, Yuzawa M (2009) Double staining with brilliant blue G and double peeling for epiretinal membranes. Ophthalmology 116:1370–1376
Park DW, Dugel PU, Garda J, Sipperley JO, Thach A, Sneed SR, Blaisdell J (2003) Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology 110:62–64
Kadonosono K, Yamakawa T, Uchio E, Yanagi Y, Tamaki Y, Araie M (2006) Comparison of visual function after epiretinal membrane removal by 20-gauge and 25-gauge vitrectomy. Am J Ophthalmol 142:513–515
Lubinski W, Goslawski W, Podboraczynska-Jodko K, Mularczyk M, Post M (2020) Comparison of 27-gauge versus 25-gauge vitrectomy results in patients with epiretinal membrane: 6-month follow-up. Int Ophthalmol 40:867–875
Mori R, Naruse S, Shimada H (2018) Comparative study of 27-gauge and 25-gauge vitrectomy performed as day surgery. Int Ophthalmol 38:1575–1582
Naruse S, Shimada H, Mori R (2017) 27-Gauge and 25-gauge vitrectomy day surgery for idiopathic epiretinal membrane. BMC Ophthalmol 17:188
Kadonosono K, Itoh N, Nomura E, Ohno S (1999) Perifoveal microcirculation in eyes with epiretinal membranes. Br J Ophthalmol 83:1329–1331
Kadonosono K, Itoh N, Nomura E, Ohno S (1999) Capillary blood flow velocity in patients with idiopathic epiretinal membranes. Retina 19:536–539
Machado LM, Furlani BA, Navarro RM, Farah ME, Maia A, Magalhaes O Jr, Rodrigues EB, Moraes N, Maia M (2015) Preoperative and intraoperative prognostic factors of epiretinal membranes using chromovitrectomy and internal limiting membrane peeling. Ophthalmic Surg Lasers Imaging Retina 46:457–462
Xiao W, Chen X, Yan W, Zhu Z, He M (2017) Prevalence and risk factors of epiretinal membranes: a systematic review and meta-analysis of population-based studies. BMJ Open 7:e014644
Ye H, Zhang Q, Liu X, Cai X, Yu W, Yu S, Wang T, Lu W, Li X, Hu Y, Yang B, Zhao P (2015) Prevalence and associations of epiretinal membrane in an elderly urban Chinese population in China: the Jiangning Eye Study. Br J Ophthalmol 99:1594–1597
Koh V, Cheung CY, Wong WL, Cheung CM, Wang JJ, Mitchell P, Younan C, Saw SM, Wong TY (2012) Prevalence and risk factors of epiretinal membrane in Asian Indians. Invest Ophthalmol Vis Sci 53:1018–1022
Kawasaki R, Wang JJ, Mitchell P, Aung T, Saw SM, Wong TY (2008) Racial difference in the prevalence of epiretinal membrane between Caucasians and Asians. Br J Ophthalmol 92:1320–1324
Jia Y, Wei E, Wang X, Zhang X, Morrison JC, Parikh M, Lombardi LH, Gattey DM, Armour RL, Edmunds B, Kraus MF, Fujimoto JG, Huang D (2014) Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology 121:1322–1332
Jia Y, Bailey ST, Wilson DJ, Tan O, Klein ML, Flaxel CJ, Potsaid B, Liu JJ, Lu CD, Kraus MF, Fujimoto JG, Huang D (2014) Quantitative optical coherence tomography angiography of choroidal neovascularization in age-related macular degeneration. Ophthalmology 121:1435–1444
Jia Y, Tan O, Tokayer J, Potsaid B, Wang Y, Liu JJ, Kraus MF, Subhash H, Fujimoto JG, Hornegger J, Huang D (2012) Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express 20:4710–4725
Scarinci F, Nesper PL, Fawzi AA (2016) Deep retinal capillary nonperfusion is associated with photoreceptor disruption in diabetic macular ischemia. Am J Ophthalmol 168:129–138
Roisman L, Rosenfeld PJ (2016) Optical coherence tomography angiography of macular telangiectasia type 2. Dev Ophthalmol 56:146–158
Matet A, Daruich A, Dirani A, Ambresin A, Behar-Cohen F (2016) Macular telangiectasia type 1: capillary density and microvascular abnormalities assessed by optical coherence tomography angiography. Am J Ophthalmol 167:18–30
Lin TC, Chung YC, Lin CY, Lee FL, Chen SJ (2016) Focal nonperfusion of deep retinal capillary plexus in eyes with epiretinal membranes revealed by optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina 47:404–409
Zhang Q, Wang RK, Chen CL, Legarreta AD, Durbin MK, An L, Sharma U, Stetson PF, Legarreta JE, Roisman L, Gregori G, Rosenfeld PJ (2015) Swept source optical coherence tomography angiography of neovascular macular telangiectasia type 2. Retina 35:2285–2299
Spaide RF, Curcio CA (2017) Evaluation of segmentation of the superficial and deep vascular layers of the retina by optical coherence tomography angiography instruments in normal eyes. JAMA Ophthalmol 135:259–262
Team RC (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. Available: http://www.R-project.org. Accessed 27 Apr 2020
Soper DS (2020) Post-hoc Statistical Power Calculator for Multiple Regression [Software]. Available from http://www.danielsoper.com/statcalc. Accessed 27 Apr 2020
Weinberger D, Stiebel-Kalish H, Priel E, Barash D, Axer-Siegel R, Yassur Y (1999) Digital red-free photography for the evaluation of retinal blood vessel displacement in epiretinal membrane. Ophthalmology 106:1380–1383
Nitta E, Shiraga F, Shiragami C, Fukuda K, Yamashita A, Fujiwara A (2013) Displacement of the retina and its recovery after vitrectomy in idiopathic epiretinal membrane. Am J Ophthalmol 155:1014–1020 e1011
Kim YJ, Kim S, Lee JY, Kim JG, Yoon YH (2018) Macular capillary plexuses after epiretinal membrane surgery: an optical coherence tomography angiography study. Br J Ophthalmol 102:1086–1091
Mastropasqua R, D’Aloisio R, Viggiano P, Borrelli E, Iafigliola C, Di Nicola M, Aharrh-Gnama A, Di Marzio G, Toto L, Mariotti C, Carpineto P (2019) Early retinal flow changes after vitreoretinal surgery in idiopathic epiretinal membrane using swept source optical coherence tomography angiography. J Clin Med 8
Pierro L, Iuliano L, Marchese A, Arrigo A, Rabiolo A, Bandello F (2019) Reduced vascular perfusion density in idiopathic epiretinal membrane compared to macular pseudohole. Int Ophthalmol 39:2749–2755
Nelis P, Alten F, Clemens CR, Heiduschka P, Eter N (2017) Quantification of changes in foveal capillary architecture caused by idiopathic epiretinal membrane using OCT angiography. Graefes Arch Clin Exp Ophthalmol 255:1319–1324
Yu Y, Teng Y, Gao M, Liu X, Chen J, Liu W (2017) Quantitative choriocapillaris perfusion before and after vitrectomy in idiopathic epiretinal membrane by optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina 48:906–915
Romano MR, Cennamo G, Schiemer S, Rossi C, Sparnelli F (2017) Deep and superficial OCT angiography changes after macular peeling: idiopathic vs diabetic epiretinal membranes. Graefes Arch Clin Exp Ophthalmol 255:681–689
Mastropasqua L, Borrelli E, Carpineto P, Toto L, Di Antonio L, Mattei PA, Mastropasqua R (2018) Microvascular changes after vitrectomy with internal limiting membrane peeling: an optical coherence tomography angiography study. Int Ophthalmol 38:1465–1472
Clark A, Balducci N, Pichi F, Veronese C, Morara M, Torrazza C, Ciardella AP (2012) Swelling of the arcuate nerve fiber layer after internal limiting membrane peeling. Retina 32:1608–1613
Scupola A, Grimaldi G, Abed E, Sammarco MG, Giudiceandrea A, Greco A, Sasso P, Blasi MA (2018) Arcuate nerve fiber layer changes after internal limiting membrane peeling in idiopathic epiretinal membrane. Retina 38:1777–1785
Winegarner A, Wakabayashi T, Fukushima Y, Sato T, Hara-Ueno C, Busch C, Nishiyama I, Shiraki N, Sayanagi K, Nishida K, Sakaguchi H (2018) Changes in retinal microvasculature and visual acuity after antivascular endothelial growth factor therapy in retinal vein occlusion. Invest Ophthalmol Vis Sci 59:2708–2716
Wakabayashi T, Sato T, Hara-Ueno C, Fukushima Y, Sayanagi K, Shiraki N, Sawa M, Ikuno Y, Sakaguchi H, Nishida K (2017) Retinal microvasculature and visual acuity in eyes with branch retinal vein occlusion: imaging analysis by optical coherence tomography angiography. Invest Ophthalmol Vis Sci 58:2087–2094
Kang JW, Yoo R, Jo YH, Kim HC (2017) Correlation of microvascular structures on optical coherence tomography angiography with visual acuity in retinal vein occlusion. Retina 37:1700–1709
Lee J, Moon BG, Cho AR, Yoon YH (2016) Optical coherence tomography angiography of DME and its association with anti-VEGF treatment response. Ophthalmology 123:2368–2375
Moon BG, Um T, Lee J, Yoon YH (2018) Correlation between deep capillary plexus perfusion and long-term photoreceptor recovery after diabetic macular edema treatment. Ophthalmol Retina 2:235–243
Rice TA, De Bustros S, Michels RG, Thompson JT, Debanne SM, Rowland DY (1986) Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology 93:602–610
Kauffmann Y, Ramel JC, Lefebvre A, Isaico R, De Lazzer A, Bonnabel A, Bron AM, Creuzot-Garcher C (2015) Preoperative prognostic factors and predictive score in patients operated on for combined cataract and idiopathic epiretinal membrane. Am J Ophthalmol 160:185–192 e185
Oh HN, Lee JE, Kim HW, Yun IH (2013) Clinical outcomes of double staining and additional ILM peeling during ERM surgery. Korean J Ophthalmol 27:256–260
Pournaras CJ, Emarah A, Petropoulos IK (2011) Idiopathic macular epiretinal membrane surgery and ILM peeling: anatomical and functional outcomes. Semin Ophthalmol 26:42–46
Ripandelli G, Scarinci F, Piaggi P, Guidi G, Pileri M, Cupo G, Sartini MS, Parisi V, Baldanzellu S, Giusti C, Nardi M, Stirpe M, Lazzeri S (2015) Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina 35:498–507
Tari SR, Vidne-Hay O, Greenstein VC, Barile GR, Hood DC, Chang S (2007) Functional and structural measurements for the assessment of internal limiting membrane peeling in idiopathic macular pucker. Retina 27:567–572
Ueno S, Kondo M, Piao CH, Ikenoya K, Miyake Y, Terasaki H (2006) Selective amplitude reduction of the PhNR after macular hole surgery: ganglion cell damage related to ICG-assisted ILM peeling and gas tamponade. Invest Ophthalmol Vis Sci 47:3545–3549
Russo A, Morescalchi F, Gambicorti E, Cancarini A, Costagliola C, Semeraro F (2019) Epiretinal membrane removal with foveal-sparing internal limiting membrane peeling: a pilot study. Retina 39:2116–2124
Acknowledgments
The principal investigators, Dr. Urara Osada and Dr. Masayuki Yasuda, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis. This paper was supported by JST grants from JSPS KAKENHI Grants-in-Aid for Scientific Research (C) (H.K. 17K11445). The funders had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Involved in design and conduct of the study were (H.K. and T.N.); preparation, collection, management, analysis, and interpretation of the data (U.O., H.K., M.Y., K.H., K.N. and T.N.); and approval of the manuscript (T.N.). H.K. wrote the main manuscript text. U.O. and M.Y. prepared all tables and all figures, and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Osada, U., Kunikata, H., Yasuda, M. et al. Association of retinal vessel density with retinal sensitivity in surgery for idiopathic epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 258, 1911–1920 (2020). https://doi.org/10.1007/s00417-020-04754-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04754-0