Abstract
Purpose
To determine the prevalence of and identify factors associated with visual impairment and blindness in institutionalized elderly in Germany.
Methods
In this prospective multicenter cross-sectional study, ophthalmic health care need and provision were investigated in institutionalized elderly in 32 nursing homes in Germany. All participants underwent a standardized examination including medical and ocular history, refraction, visual acuity testing, tonometry, biomicroscopy, and dilated funduscopy. A standardized questionnaire was used to identify factors associated with eye healthcare utilization, visual impairment and/or blindness.
Results
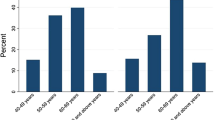
Visual acuity of 566 (94.3%; 413 women and 153 men) of a total of 600 institutionalized elderly was determined. Mean age of the included patients was 82.9 years (± 9.8). Of all participants, 30 (5.3%; 95% CI 3.4–7.2%) were blind and 106 (18.7%; 95% CI 15.5–21.9%) were moderately or severely visually impaired according to the World Health Organization definition. The 136 blind and moderately or severely visually impaired participants were older (OR, Odds Ratio = 1.1, 95% CI 1.0–1.1; p < 0.001), and more likely to have reduced mobility (OR = 12.6, 95% CI 2.8–57.6; p = 0.001).
Conclusion
A high proportion of blindness and visual impairment was found amongst nursing home residents. Age and reduced mobility were factors associated with an increased likelihood of blindness and visual impairment. Any surveys of blindness and visual impairment excluding nursing homes may considerably underestimate the prevalence of visual impairment and blindness.
Similar content being viewed by others
Change history
06 March 2019
The original version of this article inadvertently contained a mistake. Authors incorrectly listed in PDF version while correctly presented in the html version.
References
Bourne RRA, Flaxman SR, Braithwaite T et al (2017) Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 5(9):e888–e897. https://doi.org/10.1016/S2214-109X(17)30293-0
VanNewkirk MR, Weih LA, McCarty CA et al (2000) Visual impairment and eye diseases in elderly institutionalized Australians. Ophthalmology 107(12):2203–2208. https://doi.org/10.1016/S0161-6420(00)00459-0
Tielsch JM, Javitt JC, Coleman A et al (1995) The prevalence of blindness and visual impairment among nursing home residents in Baltimore. N Engl J Med 332(18):1205–1209. https://doi.org/10.1056/NEJM199505043321806
Mitchell P, Hayes P, Wang JJ (1997) Visual impairment in nursing home residents: the Blue Mountains Eye Study. Med J Aust 166(2):73–76
Finger RP, Fimmers R, Holz FG, Scholl HPN (2011) Prevalence and causes of registered blindness in the largest federal state of Germany. Br J Ophthalmol 95(8):1061–1067. https://doi.org/10.1136/bjo.2010.194712
Varma R, Vajaranant TS, Burkemper B et al (2016) Visual impairment and blindness in adults in the United States. JAMA Ophthalmol 134(7):802. https://doi.org/10.1001/jamaophthalmol.2016.1284
Gaugler JE, Yu F, Krichbaum K, Wyman JF (2009) Predictors of nursing home admission for persons with dementia. Med Care 47(2):191–198. https://doi.org/10.1097/MLR.0b013e31818457ce
Thibault L, Kergoat H (2016) Eye care services for older institutionalised individuals affected by cognitive and visual deficits: a systematic review. Ophthalmic Physiol Opt 36(5):566–583. https://doi.org/10.1111/opo.12311
Garin N, Olaya B, Lara E et al (2014) Visual impairment and multimorbidity in a representative sample of the Spanish population. BMC Public Health 14(1):815. https://doi.org/10.1186/1471-2458-14-815
Mojon-Azzi SM, Sousa-Poza A, Mojon DS (2008) Impact of low vision on well-being in 10 European countries. Ophthalmologica 222(3):205–212. https://doi.org/10.1159/000126085
Rogers MAM, Langa KM (2010) Untreated poor vision: a contributing factor to late-life dementia. Am J Epidemiol 171(6):728–735. https://doi.org/10.1093/aje/kwp453
Bowen M, Edgar DF, Hancock B et al (2016) The prevalence of visual impairment in people with dementia (the PrOVIDe study): a cross-sectional study of people aged 60–89 years with dementia and qualitative exploration of individual, carer and professional perspectives. Heal Serv Deliv Res 4(21):1–200. https://doi.org/10.3310/hsdr04210
Hoffmann W, van den Berg N, Stenzel U et al (2014) Demografischer Wandel. Ophthalmologe 53(5):428–437. https://doi.org/10.1007/s00347-013-2923-x.
Wolfram C, Pfeiffer N (2012) Weißbuch zur Situation der ophthalmologischen Versorgung in Deutschland. DOG Deutsche Ophthalmologische Gesellschaft, München
Fang PP, Schnetzer A, Kupitz DG et al (2017) Ophthalmologische Versorgung in Seniorenheimen: Die OVIS-Studie. Ophthalmologe 114(9):818–827. https://doi.org/10.1007/s00347-017-0557-0
Swenor BK, Muñoz B, West SK (2013) Does visual impairment affect mobility over time? The Salisbury Eye Evaluation study. Investig Ophthalmol Vis Sci 54(12):7683–7690. https://doi.org/10.1167/iovs.13-12869
Gräßel E, Donath C, Lauterberg J et al (2008) Demenzkranke und pflegestufen: Wirken sich krankheitssymptome auf die einstufung aus? Gesundheitswesen 70(3):129–136. https://doi.org/10.1055/s-2008-1062733
World Health Organization (2016) ICD-10 Version: 2016. http://apps.who.int/classifications/icd10/browse/2016/en#!/H53-H54. Accessed 9 May 2018
Finger RP (2007) Blindheit in Deutschland: Dimensionen und Perspektiven. Ophthalmologe 104(10):839–844. https://doi.org/10.1007/s00347-007-1600-3
Finger RP, Bertram B, Wolfram C, Holz FG (2012) Blindness and visual impairment in Germany: a slight fall in prevalence. Dtsch Arztebl Int 109(27–28):484–489. https://doi.org/10.3238/arztebl.2012.0484
Klaver CC, Wolfs RC, Vingerling JR et al (1998) Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam study. Arch Ophthalmol 116(5):653–658
Limburg H, Keunen JEE (2009) Blindness and low vision in the Netherlands from 2000 to 2020 — modeling as a tool for focused intervention. Ophthalmic Epidemiol 16(6):362–369. https://doi.org/10.3109/09286580903312251
Newland HS, Hiller JE, Casson RJ, Obermeder S (1996) Prevalence and causes of blindness in the South Australian population aged 50 and over. Ophthalmic Epidemiol 3(2):97–107
Bourne RRA, Jonas JB, Bron AM et al (2018) Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: magnitude, temporal trends and projections. Br J Ophthalmol 102(5):575–585. https://doi.org/10.1136/bjophthalmol-2017-311258
Kleina T, Horn A, Suhr R, Schaeffer D (2017) Zur Entwicklung der ärztlichen Versorgung in stationären Pflegeeinrichtungen. Ergebnisse einer empirischen Untersuchung. Das Gesundheitswes 79(05):382–387. https://doi.org/10.1055/s-0035-1549971
Acknowledgments
This study was supported by the Ernst und Bertha Grimmke Foundation, Germany (PPL and TUK).
Funding
The Department of Ophthalmology, University of Bonn, received research funding from the Stiftung Auge (German Eye Foundation) of the German Ophthalmological Society (DOG) with support of Bayer and Novartis for the OVIS study. The Medical Biometry and Epidemiology Unit of Witten/Herdecke University received research funding from the University of Bonn (Eye Hospital) for the methodological counseling of this investigation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure of potential conflicts of interest
S. Thiele reports personal fees from Carl Zeiss MediTec, Heidelberg Engineering, and Optos, outside the submitted work. T. U. Krohne reports personal fees from Alimera Sciences, Bayer, Heidelberg Engineering, and Novartis, outside the submitted work. F. Ziemssen has received honoraria for consultation and research from Alimera, Allergan, Bayer, Biogen, MSD, Novartis, NovoNordisk and Roche, none was related to the topic. F.G. Holz reports personal fees from Acucela, Allergan, Bayer, Bioeq, Boehringer Ingelheim, Carl Zeiss MediTec, Genentech/Roche, Heidelberg Engineering, Merz, NightstarX, Novartis, Optos, Pixium and Thea, outside the submitted work. R. P. Finger reports personal fees from Bayer, Opthea, Santen, Novartis, Retina Implant and Novelion, outside the submitted work.
None of the sponsors had any role in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication. None of the authors has any proprietary or competing interests to disclose.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local ethic committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants or their legal guardians included in the study.
Appendix
Appendix
Contributing Centers and Members Participating in the OVIS Study
-
Department of Ophthalmology, University of Frankfurt, Germany: Prof. Dr. Thomas Kohnen, Dr. Lubka Naycheva, Maximilian Jochem
-
Department of Ophthalmology, University of Freiburg, Germany: Prof. Dr. Thomas Reinhard, Prof. Dr. Daniel Böhringer, Dr. Diana Engesser, Prof. Dr. Wolf Lagrèze, Claudia Müller, Carolin Wolff, Jessica Schmitz
-
Department of Ophthalmology, University of Gießen, Germany: Prof. Dr. Birgit Lorenz, Chrysanthi Papadopoulou-Laiou, Kerstin Holve, Silke Schweinfurth
-
Department of Ophthalmology, University of Göttingen, Germany: Prof. Dr. Hans Hoerauf, Dr. Wiebke Schwarz
-
Department of Ophthalmology, University of Hamburg, Germany: Prof. Dr. Martin Spitzer, PD Dr. Lars Wagenfeld, Paul Bertram
-
Department of Ophthalmology, University of Heidelberg, Germany: Prof. Dr. Gerd Auffarth, Branka Gavrilović
-
Department of Ophthalmology, University of Cologne, Germany: Prof. Dr. Claus Cursiefen, Dr. Friederike Schaub, Anna Lentzsch, Dr. Gerhard Welsandt
-
Department of Ophthalmology, University of Magdeburg, Germany: Prof. Dr. Hagen Thieme, Dr. Melanie Weigel, Diyala Hidaya, Angela Ehmer
-
Department of Ophthalmology, Ludwig-Maximilians University Munich, Germany: Prof. Dr. Siegfried Priglinger, Dr. Bettina von Livonius, Carina Drexler, Jessica Semmelsberger
-
Department of Ophthalmology, University of Münster, Germany: Prof. Dr. Nicole Eter, PD Dr. Florian Alten, Annika Sigleur, Dorothee Sieber, Andrea Bräutigam, Friederike Härter, Adeline Adorf
-
Department of Ophthalmology, St. Franziskus-Hospital Münster, Germany: Prof. Dr. Daniel Pauleikhoff, Dr. Angela Robering
-
Department of Ophthalmology, University of Regensburg, Germany: Prof. Dr. Horst Helbig, Dr. Caroline Brandl
-
Department of Ophthalmology, University of Tübingen, Germany: Prof. Dr. Focke Ziemssen, Dr. Daniel Röck
-
Institute for Medical Biometry and Epidemiology, University of Witten/Herdecke, Germany: Prof. Dr. Frank Krummenauer, Sabrina Tulka, M. Sc.
-
Department of Ophthalmology, University of Bonn, Germany: Prof. Dr. Frank G. Holz, Prof. Dr. Robert P. Finger, Prof. Bettina Wabbels, Dr. David. G. Kupitz, Dr. Arno P. Göbel, Dr. Julia Steinberg, Dr. Petra P. Larsen, Anne Schnetzer, Bianka Kobialka, Beate Prinz, Danielle Kutten, Pia Schneider, Olivia Toczko, Thanushiya Yoganathan
Rights and permissions
About this article
Cite this article
Larsen, P.P., Thiele, S., Krohne, T.U. et al. Visual impairment and blindness in institutionalized elderly in Germany. Graefes Arch Clin Exp Ophthalmol 257, 363–370 (2019). https://doi.org/10.1007/s00417-018-4196-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4196-1