Abstract
Purpose
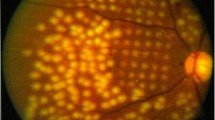
Retinal diseases are closely associated with both decreased oxygenation and increased inflammation. It is not known if hypoxia-induced vascular endothelial growth factor (VEGF) expression in the retina itself evokes inflammation, or whether inflammation is a prerequisite for the development of neovascularization.
Methods
Human ARPE-19 cell line and primary human retinal pigment epithelium (RPE) cells were used. ARPE-19 cells were kept either under normoxic (24 h or 48 h) or hypoxic conditions (1% O2, 24 h). Part of the cells were re-oxygenated (24 h). Some ARPE-19 cells were additionally pre-treated with bacterial lipopolysaccharide (LPS). The levels of IL-6, IL-8, IL-1β, and IL-18 were determined from medium samples by an enzyme-linked immunosorbent assay (ELISA) method. Primary human RPE cells were exposed to hypoxia for 24 h, and the subsequent release of IL-6 and IL-8 was measured with ELISA. VEGF secretion from ARPE-19 cells was determined up to 24 h.
Results
Hypoxia induced significant (P < 0.01) increases in the levels of both IL-6 and IL-8 in ARPE-19 cells, and LPS pre-treatment further enhanced these responses. Hypoxia exposure did not affect the IL-1β or IL-18 release irrespective of LPS pre-treatment. If primary RPE cells were incubated for 4 h in hypoxic conditions, IL-6 and IL-8 concentrations were increased by 7 and 8-fold respectively. Hypoxia increased the VEGF secretion from ARPE-19 cells in a similar manner with or without pre-treatment with LPS.
Conclusions
Hypoxia causes an inflammatory reaction in RPE cells that is potentiated by pre-treatment with the Toll-like receptor-activating agent, LPS. The secretion of VEGF from these cells is regulated directly by hypoxia and is not mediated by inflammation.




Similar content being viewed by others
References
Arjamaa O, Nikinmaa M (2006) Oxygen-dependent diseases in the retina: role of hypoxia-inducible factors. Exp Eye Res 83:473–483
Arjamaa O, Nikinmaa M, Salminen A, Kaarniranta K (2009) Regulatory role of HIF-1α in the pathogenesis of age-related macular degeneration (AMD). Ageing Res Rev 8:349–358
Lange CA, Stavrakas P, Luhmann UF, de Silva DJ, Ali RR, Gregor ZJ, Bainbridge JW (2011) Intraocular oxygen distribution in advanced proliferative diabetic retinopathy. Am J Ophthalmol 152:406–412
Rius J, Guma M, Schachtrup C, Akassoglou K, Zinkernagel AS, Nizet V, Johnson RS, Haddad GG, Karin M (2008) NF-kB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1α. Nature 453:807–811
Taylor CT (2008) Interdependent roles of hypoxia inducible factor and nuclear factor-kB in hypoxic inflammation. J Physiol 586:4055–4059
D’Ignazio L, Bandarra D, Rocha S (2016) NF-kB and HIF crosstalk in immune responses. FEBS J 283:413–424
Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF (1983) Tumor cells secrete a vascular permeability actor that promotes accumulation of ascites fluid. Science 219:9835–9836
Biddlestone J, Bandarra D, Rocha S (2015) The role of hypoxia in inflammatory disease. Int J Mol Med 35:859–869
Fearon U, Canavan M, Biniecka M, Veale DJ (2016) Hypoxia, mitochondrial dysfunction and synovial invasiveness in rheumatoid arthritis. Nat Rev Rheumatol 12:385–897
Simats A, Garcia-Berrocoso T, Montaner J (2016) Neuroinflammatory biomarkers: from stroke diagnosis and prognosis to therapy. Biochim Biophys Acta 1862:411–424
Wu J, Stefaniak J, Hafner C, Schramel JP, Kaun C, Wojta J, Ullrich R, Tretter VE, Markstaller K, Klein KU (2016) Intermittent hypoxia causes inflammation and injury to human adult cardiac myocytes. Anesth Analg 122:373–380
Ramakrishnan S, Anand V, Roy S (2014) Vascular endothelial growth factor signaling in hypoxia and inflammation. J Neuroimmune Pharmacol 9:142–160
Semeraro F, Cancarini A, dell’Omo R, Rezzola S, Romano MR, Costagliola C (2015) Diabetic retinopathy: vascular and inflammatory disease. J Diabetes Res 2015:1–16
Kauppinen A, Paterno JJ, Blasiak J, Salminen A, Kaarniranta K (2016) Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci 73:1765–1786
dell’Omo R, Semeraro F, Bamonte G, Cifariello F, Romano MR, Costagliola C (2013) Vitreous mediators in retinal hypoxic diseases. Mediat Inflamm 2013:1–16
Canataroglu H, Varinli I, Ozcan AA, Canataroglu A, Doran F, Varinli S (2005) Interleukin (IL)-6, interleukin (IL)-8 levels and cellular composition of the vitreous humor in proliferative diabetic retinopathy, proliferative vitreoretinopathy, and traumatic proliferative vitreoretinopathy. Ocul Immunol Inflamm 13:375–381
Arjamaa O, Pöllönen M, Kinnunen K, Ryhänen T, Kaarniranta K (2011) Increased IL-6 levels are not related to NF-kB or HIF-1α transcription factors activity in the vitreous of proliferative diabetic retinopathy. J Diabetes Complications 25:393–397
Koskela UE, Kuusisto SM, Nissinen AE, Savolainen MJ, Liinamaa MJ (2013) High vitreous concentrations of IL-6 and IL-8, but not of adhesion molecules in relation to plasma concentrations in proliferative diabetic retinopathy. Ophthalmic Res 49:108–114
Chernykh VV, Varvarinsky EV, Smirnov EV, Chernykh DV, Trunov AN (2015) Proliferative and inflammatory factors in the vitreous of patients with proliferative diabetic retinopathy. Indian J Ophthalmol 63:33–36
Xu Y, Cheng Q, Yang B, Yu S, Xu F, Lu L, Liang X (2015) Increased sCD200 levels in vitreous of patients with proliferative diabetic retinopathy and its correlation with VEGF and pro-inflammatory cytokines. Invest Ophthalmol Vis Sci 56:6565–6572
Kovacs K, Marra KV, Yu G, Wagley S, Ma J, Teague GC, Nandakumar N, Lashkari K, Arroyo JG (2015) Angiogenic and inflammatory vitreous biomarkers associated with increasing levels of retinal ischemia. Invest Ophthalmol Vis Sci 56:6523–6530
Szatmári-Tóth M, Kristóf E, Veréb Z, Akhtar S, Facskó A, Fésüs L, Kauppinen A, Kaarniranta K, Petrovski G (2016) Clearance of autophagy-associated dying retinal pigment epithelial cells — a possible source for inflammation in age-related macular degeneration. Cell Death Dis 7(9):e2367. doi:10.1038/cddis.2016.133
Klettner A, Kauppinen A, Blasiak J, Roider J, Salminen A, Kaarniranta K (2013) Cellular and molecular mechanisms of age-related macular degeneration: from impaired autophagy to neovascularization. Int J Biochem Cell Biol 45:1457–1467
Kauppinen A, Niskanen H, Suuronen T, Kinnunen K, Salminen A, Kaarniranta K (2012) Oxidative stress activates NLRP3 inflammasomes in ARPE-19 cells — implications for age-related macular degeneration (AMD). Immunol Lett 147:29–33
Yellon DM, Hausenloy DJ (2007) Myocardial reperfusion injury. N Engl J Med 357:1121–1135
Lally DR, Shah CP, Heier JS (2016) Vascular endothelial growth factor and diabetic macular edema. Surv Ophthalmol. doi:10.1016/j.survophthal.2016.03.010
Diabetic Retinopathy Clinical Research Network (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 372:1193–1203
Acknowledgements
We warmly thank Dr. Ewen MacDonald for the language revision and Res. Dir. Emeritus Antero Salminen for the valuable collaboration, discussions, and critical review of the manuscript. Part of the results was published as an abstract at EVER meeting (Acta Ophthalmol. 2015, http://dx.doi.org/10.1111/j.1755-3768.2015.0426).
Author information
Authors and Affiliations
Contributions
OA, VA, KK, and AK: designing, supervision, and reporting of the study. NP, VA, AK, TC, and GP: collection, analysis, and interpretation of the data as well as critical revision of the manuscript.
Corresponding author
Ethics declarations
All procedures performed in the experiments involving human material were in accordance with the local institutional ethical review board and with the Helsinki Declaration. For this type of a study, a formal consent was not required.
Funding
The research was financially supported by the Academy of Finland (Health Research Council project 297,267), the Finnish Cultural Foundation (Central and North-Savo Foundations), the Alfred Kordelin Foundation, the Emil Aaltonen Foundation, the Finnish Eye Foundation, and the Kuopio University Hospital (VTR funding), GINOP- 2.3.2–15–2016-00006 (Hungary), co-financed by the EU and the European Regional Development Fund.
Conflict of interest
All authors certify that they have no involvement in any organization with any financial interest in the subject matter or the materials discussed in the this manuscript.
Competing interests
None declared.
Rights and permissions
About this article
Cite this article
Arjamaa, O., Aaltonen, V., Piippo, N. et al. Hypoxia and inflammation in the release of VEGF and interleukins from human retinal pigment epithelial cells. Graefes Arch Clin Exp Ophthalmol 255, 1757–1762 (2017). https://doi.org/10.1007/s00417-017-3711-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3711-0